Clinical trial jobs represent a vital sector within the healthcare industry, directly impacting the development of new medicines and medical treatments. These roles are on the front lines of scientific discovery, translating laboratory research into tangible benefits for patients. Consider the path from a promising compound in a petri dish to a validated therapy in a clinic; clinical trials are the rigorous bridge that makes this journey possible. The demand for skilled professionals in this field is steadily growing, driven by an aging population and the ongoing need for innovative healthcare solutions. Navigating this landscape can seem complex, but understanding the core components and career pathways can illuminate the opportunities available.
Clinical trials are research studies conducted with human volunteers to answer specific questions about new treatments, vaccines, or devices. They serve as the final and most crucial step in the long process of bringing a new medical intervention to the public. Without well-designed and efficiently executed clinical trials, promising scientific breakthroughs would remain theoretical, unable to reach those who need them. The regulatory framework governing these trials is extensive, designed to ensure participant safety and data integrity. This framework, which includes bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), dictates the standards and procedures that must be followed.
Phases of Clinical Trials
Understanding the different phases of clinical trials is fundamental to grasping the scope of this work. Each phase has a distinct purpose and involves a progressively larger number of participants.
Phase 0 Studies
These are very early-stage, exploratory studies that involve a small number of participants (typically 10-15) and very small doses of a drug. The primary goal is to gather initial data on how the drug is absorbed, distributed, metabolized, and excreted by the body in humans. They are not designed to assess efficacy or safety in a broad sense, but rather to inform more extensive early-stage research.
Phase I Studies
This phase marks the first time a new drug or treatment is given to a small group of people (typically 20-100) to evaluate its safety, determine a safe dosage range, and identify side effects. Participants in Phase I studies are usually healthy volunteers, although in some cases (like cancer drug trials), patients with the condition being treated may participate.
Phase II Studies
Once a drug has been deemed safe in Phase I, it moves to Phase II. Here, the drug is given to a larger group of people (typically 100-300) who have the condition being treated. The focus shifts to assessing the drug’s effectiveness (efficacy) and further evaluating its safety. Researchers look for signs that the drug works against the disease or condition.
Phase III Studies
These are large-scale studies that involve hundreds or even thousands of participants (typically 300-3,000 or more) with the condition being treated. The primary goal is to confirm the drug’s effectiveness, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug or treatment to be used safely. This phase is critical for collecting the robust data needed for regulatory approval.
Phase IV Studies (Post-Marketing Surveillance)
After a drug or treatment has been approved and is available on the market, Phase IV studies continue to monitor its safety and effectiveness in larger, more diverse populations. These studies can identify rare or long-term side effects that may not have been apparent in earlier phases and can explore new uses for the drug.
The Importance of Clinical Trials in Healthcare Advancement
Without clinical trials, the development of new treatments would be a haphazard and potentially dangerous endeavor. They are the engine of medical progress, meticulously testing hypotheses and validating the efficacy and safety of interventions. Imagine a doctor prescribing a new medication without knowing its actual impact or potential harms; this is the scenario clinical trials prevent. They provide the evidence base upon which modern medicine is built, offering patients access to the latest innovations and driving improvements in health outcomes.
Key Roles in Clinical Trials
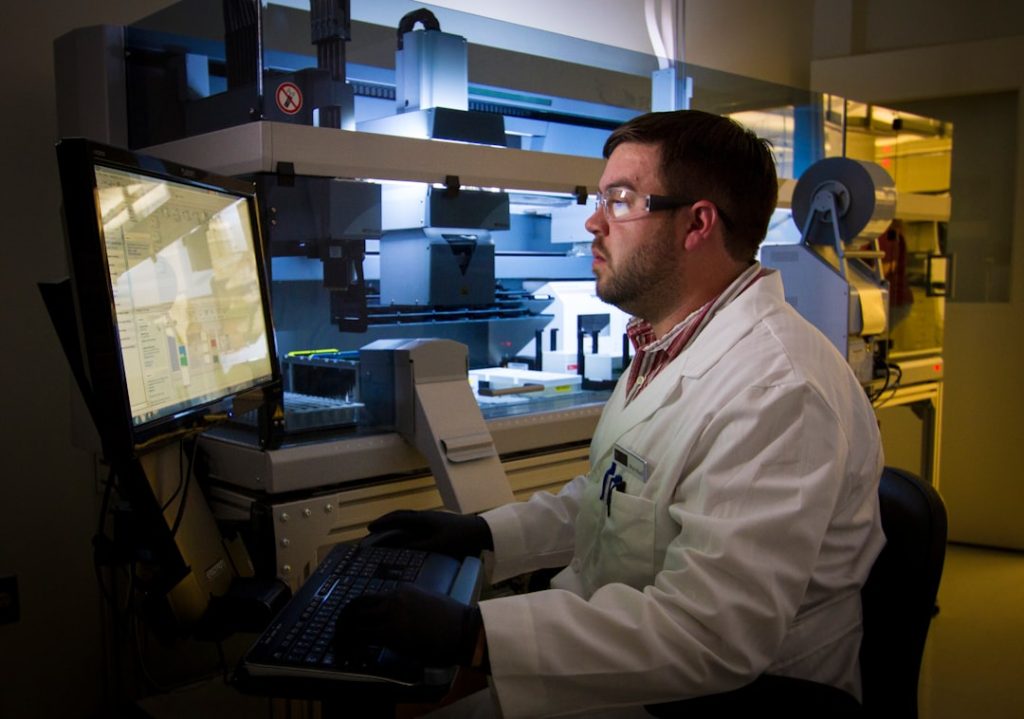
The successful execution of a clinical trial requires a diverse team of professionals, each contributing specialized skills. These roles are often interconnected, working collaboratively to ensure the trial runs smoothly and ethically. The complexity of trial design, participant recruitment, data management, and regulatory compliance necessitates a wide array of expertise.
Clinical Research Coordinators (CRCs)
CRCs are the operational backbone of clinical trials. They work closely with investigators to manage the day-to-day activities of the trial at a research site. Their responsibilities are broad and can include recruiting and screening participants, scheduling appointments, collecting and processing laboratory samples, maintaining study documentation, and ensuring adherence to the trial protocol. A CRC is often the primary point of contact for trial participants, guiding them through the study process.
Day-to-Day Responsibilities
A typical day for a CRC might involve reviewing new patient referrals, conducting screening visits to assess eligibility, administering study-related questionnaires, preparing and dispensing investigational products, performing and documenting vital signs, and liaising with the principal investigator to discuss participant progress. They are the navigators of the study at the site level.
Essential Skills for CRCs
Strong organizational skills are paramount, as CRCs manage multiple tasks and detailed records. Excellent communication and interpersonal skills are also crucial for interacting effectively with participants, physicians, and other team members. A solid understanding of medical terminology, research ethics, and regulatory requirements is also essential.
Clinical Research Associates (CRAs) / Monitors
CRAs, also known as Clinical Monitors, are typically employed by pharmaceutical companies or contract research organizations (CROs). Their role is to oversee clinical trials conducted at multiple research sites, ensuring that the trial is progressing according to the protocol, good clinical practice (GCP) guidelines, and applicable regulatory requirements. They act as auditors of the research process.
Monitoring Site Activities
CRAs conduct regular site visits to review source documents, verify data accuracy and completeness, ensure investigational products are stored and dispensed correctly, and confirm that participant rights and safety are protected. They act as the eyes and ears of the sponsor at the research site.
Regulatory Compliance and Data Integrity
A key focus for CRAs is ensuring that research sites comply with all relevant regulations (e.g., FDA regulations, ICH-GCP). They identify any deviations from the protocol or regulatory requirements and work with site staff to implement corrective actions. The integrity of the data collected is a primary concern.
Principal Investigators (PIs)
The Principal Investigator is the lead researcher responsible for the overall conduct of the clinical trial at a specific research site. Typically a physician with expertise in the disease area being studied, the PI has ultimate responsibility for the safety of the trial participants and the scientific integrity of the data collected. They are the captains of the ship in terms of medical oversight.
Medical Oversight and Participant Safety
The PI provides medical direction for the trial, makes key clinical decisions regarding participant care, and is responsible for the informed consent process. They must ensure that participants are adequately informed about the risks and benefits of participating and that their well-being is prioritized at all times.
Scientific and Ethical Conduct
The PI is accountable for ensuring that the trial is conducted in accordance with the approved protocol, scientific principles, and ethical standards. They must monitor the progress of the trial, evaluate the data, and report any serious adverse events promptly to the sponsor and regulatory authorities.
Data Managers
Data managers are responsible for the collection, cleaning, validation, and storage of clinical trial data. This role is critical for generating reliable and statistically sound results. They are the architects of the information that will ultimately determine the success or failure of a new drug.
Database Design and Management
Data managers design and manage the electronic data capture (EDC) systems used to collect trial data. They develop data entry screens, edit checks, and data validation procedures to ensure accuracy and consistency. This requires a meticulous approach to detail.
Data Analysis and Reporting
They work closely with statisticians to ensure that the data is in a format suitable for statistical analysis. Data managers also play a role in generating data queries and resolving data discrepancies, ensuring the dataset is robust for regulatory submissions.
Statisticians
Biostatisticians are essential for designing clinical trials and analyzing the collected data. Their expertise ensures that the study design allows for meaningful conclusions to be drawn and that the data is interpreted correctly. They are the interpreters of the trial’s findings.
Trial Design and Protocol Development
Statisticians contribute to the design of the trial protocol, including defining the sample size, randomization procedures, and statistical analysis plan. This ensures the study is powered to detect meaningful treatment effects if they exist.
Data Interpretation and Reporting
They perform the statistical analysis of the trial data, interpret the results, and contribute to the drafting of clinical study reports, which are submitted to regulatory agencies. Their insights are crucial for understanding the significance of the findings.
Career Paths and Education

The field of clinical trials offers diverse career trajectories, catering to individuals with varying educational backgrounds and interests. From entry-level positions to specialized scientific roles, there are pathways to suit a range of aspirations. The journey into clinical trials can begin with academic pursuits or through gaining practical experience.
Entry-Level Positions
Many individuals enter the clinical trial industry through entry-level positions. These roles often provide a solid foundation for understanding trial operations and allow for on-the-job training.
Clinical Trial Assistant (CTA)
CTAs provide administrative support to the clinical research team. They may assist with document management, data entry, scheduling, and other tasks, providing crucial support to CRCs and CRAs. This is often a stepping stone to becoming a CRC.
Research Assistant
In academic medical centers or research institutions, research assistants support PIs in conducting experiments and collecting data. Their roles can vary widely depending on the specific research area.
Academic Requirements and Qualifications
Educational backgrounds are diverse, with many roles requiring a bachelor’s degree as a minimum. However, specific fields often benefit from advanced degrees.
Bachelor’s Degrees
Degrees in life sciences (biology, chemistry, biochemistry), nursing, health sciences, or related fields are common. These provide a foundational understanding of scientific principles and human physiology.
Advanced Degrees
Master’s degrees or Doctorates are often required for more specialized roles, such as biostatistics, epidemiology, clinical pharmacology, or advanced research scientist positions. These degrees equip individuals with deeper theoretical knowledge and research methodologies.
Certifications and Specialized Training
While not always mandatory, professional certifications can enhance a candidate’s credentials and demonstrate commitment to the field. Continuous learning is a hallmark of this dynamic sector.
Certified Clinical Research Professional (CCRP)
Offered by the Society of Clinical Research Associates (SOCRA), this certification validates the knowledge and skills of clinical research professionals.
Certified Clinical Research Coordinator (CCRC)
The Association of Clinical Research Professionals (ACRP) offers this certification, recognizing the expertise of CRCs.
Good Clinical Practice (GCP) Training
GCP training is fundamental for all individuals involved in clinical trials. It ensures adherence to ethical and scientific quality standards for designing, conducting, recording, and reporting trials that involve the participation of human subjects.
Progression and Specialization
Career progression in clinical trials often involves specialization. Professionals can move from operational roles to data management, monitoring, project management, or even into regulatory affairs or drug safety.
Moving into Management
With experience, individuals can advance into project management roles, overseeing entire clinical trials from inception to completion. This requires strong leadership and organizational skills.
Specializing in Therapeutic Areas
Many professionals choose to specialize in specific therapeutic areas, such as oncology, cardiology, neurology, or infectious diseases. This allows for deeper expertise and understanding of the nuances of trials within those fields.
Regulatory Affairs and Quality Assurance
The regulatory landscape governing clinical trials is stringent, designed to protect participants and ensure the integrity of research. Professionals in regulatory affairs and quality assurance play a critical role in navigating these complex requirements. They are the guardians of the process, ensuring compliance and ethical conduct.
Understanding Regulatory Frameworks
Professionals in this area must have a thorough understanding of the guidelines and regulations set forth by national and international health authorities.
FDA Regulations
In the United States, the Food and Drug Administration (FDA) sets forth regulations for clinical trials, including Good Clinical Practice (GCP), Investigational New Drug (IND) applications, and New Drug Applications (NDAs).
ICH-GCP Guidelines
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) has developed harmonized guidelines for Good Clinical Practice, which are widely adopted globally. These guidelines provide a common standard for clinical trial conduct.
European Medicines Agency (EMA) Guidelines
The EMA oversees drug approval in the European Union, with its own set of regulations and guidelines that complement ICH-GCP.
Roles in Regulatory Affairs
This field involves ensuring that all aspects of a clinical trial comply with legal and ethical requirements.
Regulatory Affairs Specialists
These professionals prepare and submit regulatory documents, such as IND applications and amendments, to health authorities. They also liaise with regulatory agencies during the trial and ensure ongoing compliance.
Regulatory Affairs Managers
Managers oversee the regulatory strategy for a drug development program, ensuring that all submissions and activities meet regulatory requirements and timelines. They provide leadership and strategic direction.
Quality Assurance (QA) in Clinical Trials
Quality Assurance is about establishing and maintaining systems that ensure the reliability and integrity of clinical trial processes and data. It’s about building confidence in the results.
Developing and Implementing Quality Systems
QA professionals develop and implement standard operating procedures (SOPs) and quality management systems. They ensure that all trial activities are conducted according to established protocols and regulatory standards.
Auditing and Ensuring Compliance
They conduct internal and external audits of clinical trial sites, vendors, and internal processes to assess compliance. Audits are like health checks for the trial’s operations. They identify areas for improvement and ensure corrective actions are taken.
Pharmacovigilance (Drug Safety)
Pharmacovigilance is the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problem.
Monitoring Safety Data
Pharmacovigilance professionals monitor incoming safety data from clinical trials, including adverse event reports. They assess the severity and causality of these events.
Reporting Adverse Events
They are responsible for reporting serious adverse events to regulatory authorities and ethics committees in a timely and accurate manner, ensuring that any safety concerns are addressed promptly.
The Future of Clinical Trials and Career Opportunities
| Job Title | Average Salary | Required Education | Key Responsibilities | Experience Level |
|---|---|---|---|---|
| Clinical Research Associate (CRA) | 75,000 – 95,000 | Bachelor’s in Life Sciences | Monitor clinical trials, ensure compliance, data collection | Entry to Mid-level |
| Clinical Trial Manager | 90,000 – 120,000 | Bachelor’s or Master’s in Health Sciences | Oversee trial operations, manage teams, budget management | Mid to Senior-level |
| Data Manager | 70,000 – 90,000 | Bachelor’s in Computer Science or Life Sciences | Manage clinical trial data, database design, data validation | Mid-level |
| Regulatory Affairs Specialist | 65,000 – 85,000 | Bachelor’s in Pharmacy, Biology, or related field | Prepare regulatory submissions, ensure compliance with laws | Mid-level |
| Clinical Project Coordinator | 55,000 – 70,000 | Bachelor’s degree | Coordinate trial activities, communication between teams | Entry-level |
The field of clinical trials is dynamic and continuously evolving, driven by technological advancements and a growing understanding of disease. This evolution presents exciting new opportunities for professionals. The future is not a static destination; it’s a constantly shifting horizon that requires adaptation and innovation.
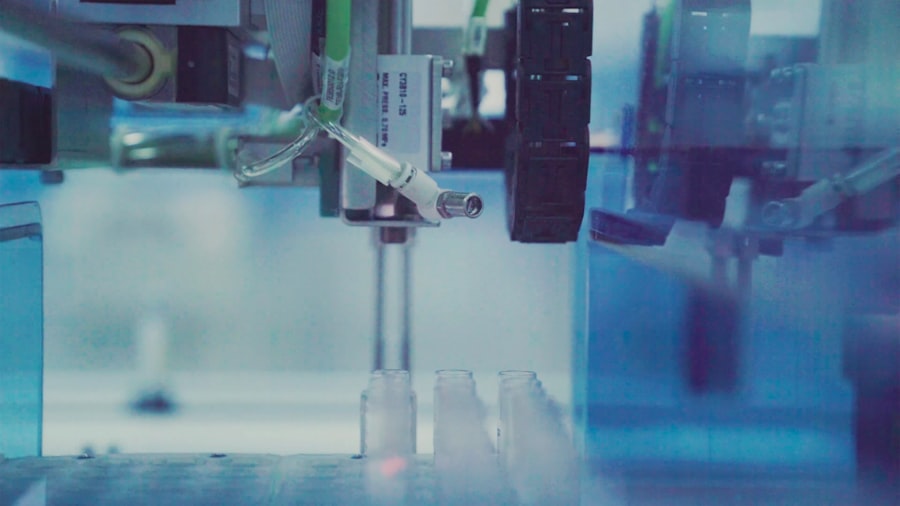
Technological Advancements
Technology is rapidly transforming how clinical trials are designed, conducted, and monitored.
Decentralized Clinical Trials (DCTs)
DCTs, also known as virtual or remote trials, increasingly leverage technology to conduct trial activities outside of traditional clinical settings. This can include remote data collection via wearable devices, telehealth visits, and mobile applications. This approach broadens access and can improve patient convenience.
Artificial Intelligence (AI) and Machine Learning (ML)
AI and ML are being used to optimize trial design, identify suitable participants more efficiently, predict patient outcomes, and analyze large datasets. These tools act as powerful analytical engines, unlocking new insights.
Real-World Data (RWD) and Real-World Evidence (RWE)
The use of RWD, collected from sources outside of traditional clinical trials (e.g., electronic health records, insurance claims), is growing. RWE, derived from these data, can supplement traditional trial data and provide insights into drug effectiveness and safety in broader populations.
Emerging Therapeutic Areas and Research Focus
The focus of clinical research is constantly shifting to address unmet medical needs.
Gene and Cell Therapies
The development of gene and cell therapies represents a significant frontier in medicine, and clinical trials are crucial for bringing these innovative treatments to patients.
Personalized Medicine
Moving beyond a one-size-fits-all approach, personalized medicine aims to tailor treatments to an individual’s genetic makeup, lifestyle, and environment. Clinical trials are essential for validating these tailored treatment strategies.
Impact on Career Opportunities
These advancements are creating new specialized roles and demanding new skill sets.
Data Science and Analytics Roles
With the increasing reliance on data, there is a growing demand for data scientists, statisticians, and bioinformaticians with expertise in handling large, complex datasets.
Technology Integration Specialists
Professionals who can bridge the gap between clinical trial operations and technology are becoming increasingly valuable. This includes roles focused on implementing and managing new digital tools and platforms for trials.
Patient-Centric Trial Design Expertise
As the industry shifts towards more patient-centric approaches, there is an increasing need for professionals who understand patient advocacy, patient engagement strategies, and the design principles that prioritize patient experience and outcomes in clinical trials. The focus is becoming more about serving the individual patient.