Clinical trials are essential for bringing new medical treatments to patients. These carefully designed studies help researchers understand if a new drug, device, or procedure is safe and effective. Think of them as a rigorous multi-stage journey, where each phase builds upon the knowledge gained from the previous one, ultimately charting a course towards improved human health.
Before diving into the individual phases, it’s crucial to grasp why clinical trials are undertaken. The fundamental goal is to answer specific scientific questions about a new medical intervention. This involves meticulously gathering data to determine:
Evaluating Safety and Dosage
A primary concern is always safety. Researchers need to confirm that a new treatment does not cause unacceptable harm.
Identifying Potential Side Effects
Every medication, even the most common, carries a risk of side effects. Clinical trials aim to identify and document these, assessing their severity and frequency.
Determining the Optimal Dosage
Finding the “sweet spot” for how much of a treatment to administer is critical. Too little might be ineffective, while too much could lead to toxicity. This involves exploring different dose levels to find the most beneficial and well-tolerated amount.
Assessing Efficacy
Beyond safety, the core question is: does it work? Clinical trials are designed to demonstrate whether a new treatment produces the desired therapeutic effect.
Measuring Therapeutic Benefit
Researchers look for measurable improvements in a patient’s condition, such as reduced tumor size, lower blood pressure, or alleviation of symptoms.
Comparing to Existing Treatments or Placebos
Often, new treatments are compared to existing standard treatments or a placebo (an inactive substance that looks like the real treatment). This comparison helps establish if the new treatment is truly better or offers a comparable benefit with fewer side effects.
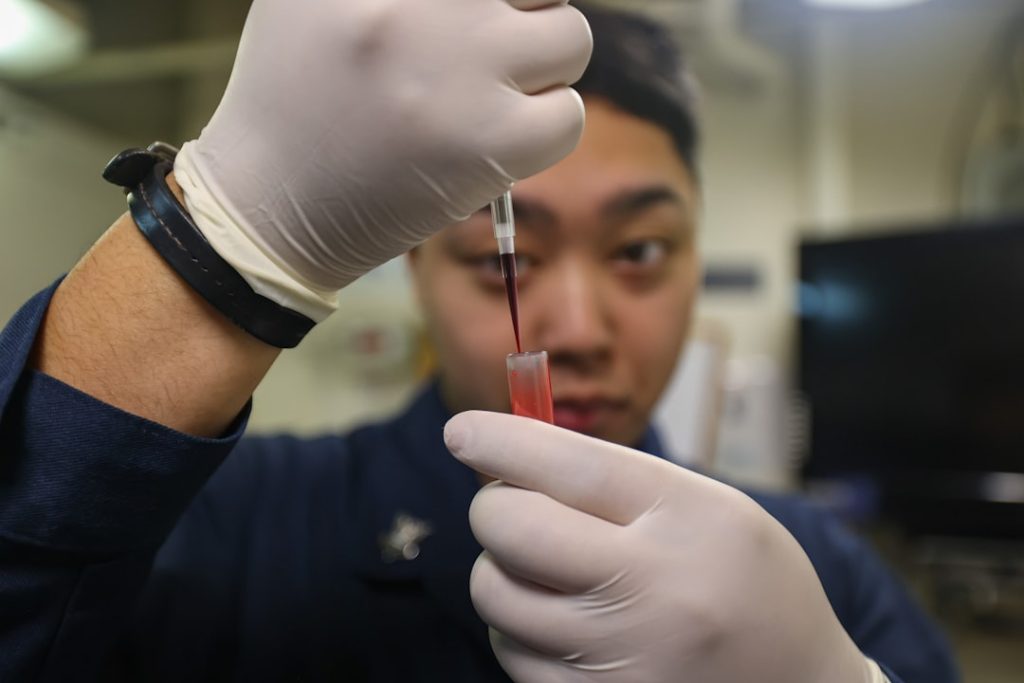
Phase 1: The Initial Safety Check
Phase 1 trials are the very first time a new drug or treatment is tested in human volunteers. This stage is primarily about safety, not necessarily efficacy. Imagine this phase as the careful initial test flight of a new aircraft before it carries passengers.
Small Group of Participants
Typically, Phase 1 trials involve a small number of healthy volunteers, although sometimes patients with the specific condition being treated may be included if the drug is expected to be highly toxic.
Focus on Safety and Tolerability
The main objective is to determine how the drug is metabolized and excreted by the body, and to identify any adverse effects. Researchers administer varying doses to assess the highest dose that can be given safely without causing severe side effects.
Dose Escalation Studies
In many Phase 1 trials, researchers use a dose escalation design. They start with a very low dose and gradually increase it in subsequent groups of participants. This process allows them to identify the maximum tolerated dose (MTD).
Pharmacokinetics and Pharmacodynamics
Crucial data gathered includes pharmacokinetic information – how the body absorbs, distributes, metabolizes, and excretes the drug – and pharmacodynamic information – how the drug affects the body and its targets.
Limited Efficacy Data
While some preliminary indications of efficacy might be observed, Phase 1 trials are not designed to prove a treatment works. The focus remains squarely on understanding how the human body responds to the new agent.
Phase 2: Exploring Efficacy and Side Effects
Once a new treatment has demonstrated acceptable safety in Phase 1, it moves to Phase 2. This phase is where the first real hints of effectiveness emerge, though the primary focus remains on further evaluating safety and determining the optimal dosing. Think of Phase 2 as testing the aircraft on a short, controlled route to see if it performs as expected.
Larger Group of Participants with the Condition
Phase 2 trials involve a larger group of people who have the specific disease or condition that the treatment is intended to address.
Assessing Efficacy and Side Effects
Researchers rigorously monitor the treatment’s effects on the condition and continue to track side effects. The goal is to determine if the treatment has a positive impact and to refine the understanding of its safety profile in the target population.
Measuring Treatment Response
Data is collected to measure how well the treatment alleviates symptoms or changes disease markers. This could involve tests, scans, or patient-reported outcomes.
Identifying the Best Dosing Regimen
Based on Phase 1 data and early Phase 2 findings, researchers can further refine the dosage and frequency of administration to maximize benefit while minimizing risks.
Further Safety Monitoring
As more people receive the treatment, a clearer picture of its potential side effects emerges. This phase allows for the identification of less common adverse events that might not have been apparent in the smaller Phase 1 studies.
Often Placebo-Controlled or Compared to Standard Care
Many Phase 2 trials are designed as randomized controlled trials, comparing the new treatment to a placebo or the current standard of care. This helps to objectively assess the treatment’s effectiveness.
Phase 3: Confirming Efficacy and Comparing to Standards

Phase 3 trials are the most extensive and critical stage in the clinical trial process, serving as the ultimate test before regulatory approval. This is akin to putting the aircraft through a full, long-haul flight, rigorously measuring its performance against established benchmarks.
Large, Diverse Patient Populations
These trials involve hundreds or even thousands of participants, often spread across multiple research centers and countries. This large sample size allows for greater statistical power and helps to identify rarer side effects.
Confirming Effectiveness and Monitoring Adverse Reactions
The primary goals are to confirm the treatment’s effectiveness in a large and diverse population and to monitor for adverse reactions in greater detail.
Randomized Controlled Trials (RCTs)
Phase 3 trials are almost always randomized controlled trials. Participants are randomly assigned to receive either the new treatment or a placebo or the current standard of care. This randomization is crucial for minimizing bias.
Statistical Significance
Researchers collect vast amounts of data to determine if the observed benefits of the new treatment are statistically significant, meaning they are unlikely to have occurred by chance.
Long-Term Safety Data
The prolonged duration of Phase 3 trials allows for the collection of crucial data on the long-term safety and potential long-term side effects of the treatment.
Basis for Regulatory Approval
Positive results from successful Phase 3 trials provide the evidence that regulatory agencies, such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA), review to decide whether to approve a new treatment for public use.
Phase 4: Post-Market Surveillance and Long-Term Studies
| Phase | Purpose | Number of Participants | Duration | Key Metrics | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety, dosage, and side effects | 20-100 healthy volunteers or patients | Several months | Maximum tolerated dose, pharmacokinetics, adverse events | 60-70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients with the condition | Several months to 2 years | Effectiveness, optimal dose, short-term side effects | 30-40% |
| Phase 3 | Confirm effectiveness, monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Clinical efficacy, safety, comparison to standard treatments | 25-30% |
| Phase 4 | Post-marketing surveillance | Thousands of patients | Ongoing | Long-term effectiveness, rare side effects, quality of life | Varies |
After a new treatment has been approved and is available to the public, it enters Phase 4, also known as post-market surveillance. This phase is about understanding the treatment’s performance and safety in the real world, over the long haul, and in broader populations. Imagine this as the ongoing monitoring and maintenance of the aircraft once it’s in regular service.
Ongoing Safety Monitoring
Phase 4 studies continue to monitor the safety of the approved treatment in the general patient population. This can reveal rare side effects that were not evident in earlier phases due to smaller sample sizes.
Identifying Rare Side Effects
Some adverse events may only occur in a very small percentage of people and may not be detected until millions of patients have used the treatment.
Drug Interactions
Phase 4 studies can also identify potential interactions between the new treatment and other medications that patients may be taking concurrently.
Further Efficacy and New Uses
Researchers may also explore the treatment’s effectiveness in different patient groups, for different durations, or for new indications not originally studied.
Real-World Evidence
This phase generates “real-world evidence” about how the treatment performs outside the controlled environment of a clinical trial, including in patients with co-existing conditions.
Cost-Effectiveness Studies
Phase 4 can also involve studies examining the cost-effectiveness of the new treatment, comparing its benefits to its cost.
Expanding Knowledge Base
Ultimately, Phase 4 trials contribute to a broader and deeper understanding of the treatment’s benefits, risks, and optimal use, informing clinical practice and potentially leading to further refinements or indications.
Ethical Considerations and Patient Rights
Throughout all phases of a clinical trial, ethical considerations are paramount. The well-being and rights of participants must be protected at all times. This is the guiding compass that ensures the journey is conducted responsibly.
Informed Consent
Potential participants must be fully informed about the trial’s purpose, procedures, potential risks, and benefits before agreeing to participate. This process, known as informed consent, ensures that individuals make voluntary and knowledgeable decisions about their involvement.
Understanding the Risks and Benefits
Participants are educated on what to expect, including any discomfort, potential side effects, and the possibility that the treatment may not work.
Voluntary Participation and Right to Withdraw
Participation is always voluntary, and individuals have the right to withdraw from a trial at any time without penalty, even if they have already consented.
Institutional Review Boards (IRBs) / Ethics Committees
Independent review boards, or ethics committees, meticulously scrutinize trial protocols before they begin. These committees are composed of scientists, ethicists, and community members charged with ensuring that research is conducted ethically and protects the rights and welfare of participants.
Protocol Review
IRBs review study protocols to ensure they are scientifically sound and ethically justified, balancing the potential benefits against the risks.
Ongoing Oversight
The IRB also provides ongoing oversight throughout the trial, reviewing any proposed changes to the protocol and monitoring the trial’s progress to ensure participant safety.
Confidentiality of Data
All data collected during a clinical trial is kept confidential, protecting participants’ privacy. Information is anonymized or de-identified to prevent the disclosure of personal health information.
Data Security
Robust measures are in place to ensure the secure storage and handling of all participant data.
Anonymization and De-identification
Techniques such as anonymization (removing all identifying information) and de-identification (removing direct identifiers but retaining some indirect identifiers that can be linked) are employed to protect privacy.
By meticulously navigating these phases, medical researchers work to bring new and improved treatments from the laboratory bench to the patient’s bedside, a journey of science, ethics, and hope.