Electronic Data Capture (EDC) systems have become a cornerstone of modern clinical trials and healthcare research. These digital platforms facilitate the collection, management, and reporting of data, replacing traditional paper-based methods. Understanding the nuances between EDC, electronic Patient-Reported Outcomes (ePRO), and electronic Clinical Outcome Assessments (eCOA) is crucial for anyone involved in research and development. This exploration aims to shed light on these technologies, their functionalities, benefits, and applications.
At their heart, EDC, ePRO, and eCOA are all digital tools designed to enhance data collection. However, they serve distinct, though often overlapping, roles. Think of them as different lenses through which you view and gather information about a study’s progress and outcomes.
Electronic Data Capture (EDC) Systems
EDC systems are the overarching framework for collecting and managing clinical trial data electronically. They are the central hub where information flows from various sources within a study.
The Evolution from Paper to Pixels
Historically, clinical trials relied on paper Case Report Forms (CRFs). Researchers meticulously recorded patient data by hand, which then underwent laborious data entry into databases. This process was prone to errors, time-consuming, and presented significant challenges for real-time monitoring and analysis. The advent of EDC systems offered a paradigm shift, akin to moving from handwritten letters to instant messaging for communication.
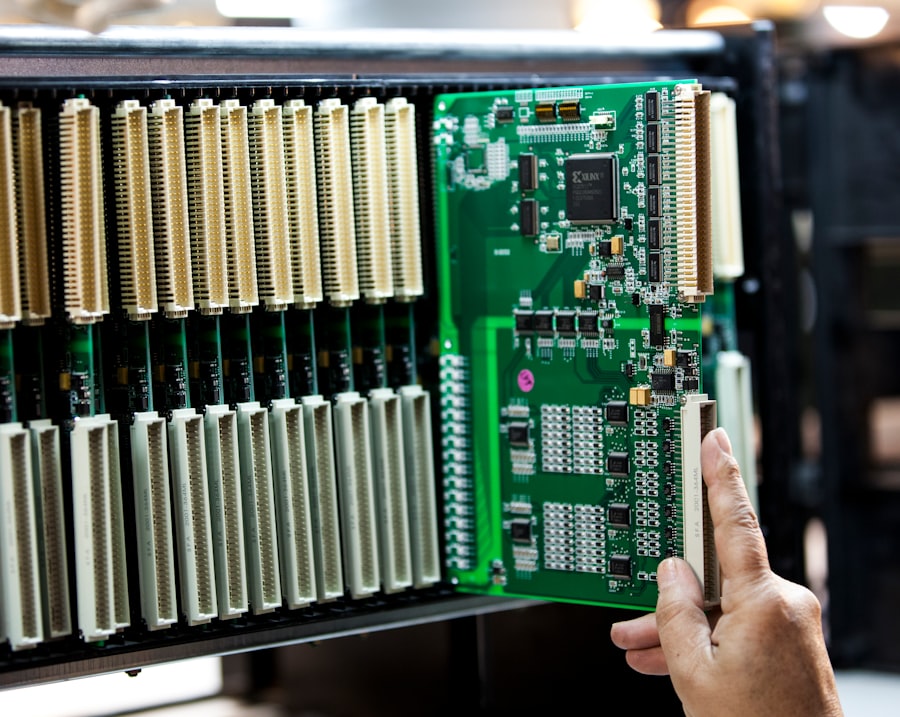
Key Components of an EDC System
An EDC system typically comprises several interconnected components:
- Electronic Case Report Forms (eCRFs): These are the digital equivalents of paper CRFs, designed to capture specific data points for each study participant at predetermined time points. eCRFs can incorporate various question types, including text fields, dropdown menus, numerical inputs, and date pickers.
- Database Management: The EDC system provides a secure and structured database to store all collected data. This database is designed to ensure data integrity, prevent duplication, and facilitate efficient querying.
- Data Validation Rules: Built-in validation checks are a critical feature of EDC systems. These rules flag discrepancies, missing data, or out-of-range values in real-time, allowing for immediate correction and reducing the need for extensive data cleaning later in the trial. This is like having a diligent proofreader constantly reviewing your work as you write.
- User Management and Access Control: EDC systems offer granular control over user roles and permissions, ensuring that only authorized personnel can access and modify specific data. This is vital for maintaining data privacy and security, adhering to regulations like HIPAA and GDPR.
- Audit Trails: A comprehensive audit trail meticulously logs every action taken within the system, including data entry, modifications, and deletions. This provides a transparent record of data handling, essential for regulatory compliance and study integrity.
Benefits of EDC Systems
The adoption of EDC systems has yielded significant advantages:
- Improved Data Quality: Real-time data validation minimizes errors and inconsistencies, leading to higher quality data for analysis.
- Increased Efficiency: Streamlined data entry and reduced manual processes save time and resources, accelerating the trial timeline.
- Enhanced Data Security: Robust security measures protect sensitive patient information.
- Real-time Data Access and Monitoring: Study sponsors and monitors can access data as it is collected, enabling timely identification of trends or issues.
- Cost Reduction: While initial investment may be required, EDC systems often lead to long-term cost savings by reducing paper-related expenses, data entry errors, and the time spent on data cleaning.
Electronic Patient-Reported Outcomes (ePRO)
ePRO refers to the use of electronic means to capture health status information directly from patients. This bypasses intermediates, such as clinicians or research staff, who might otherwise record this information.
What Constitutes a Patient-Reported Outcome?
Patient-reported outcomes (PROs) are assessments of a patient’s health condition, symptom experience, or functional status as reported by the patient. These can include measures of pain, fatigue, quality of life, mental well-being, and the occurrence of specific symptoms. Essentially, PROs capture the patient’s perspective, which is often unique and invaluable.
The Transition to ePRO
Similar to the shift from paper CRFs to eCRFs, ePRO represents the digital evolution of traditional paper questionnaires and diaries given to patients. Patients can now complete these assessments using various electronic devices.
Methods of ePRO Data Collection
ePRO data can be collected through several common methods:
- Web-Based Portals: Patients access a secure online portal via a web browser to complete their assessments. This is akin to filling out an online survey.
- Mobile Applications: Patients download dedicated mobile apps to their smartphones or tablets to record their data. This offers convenience and accessibility, especially for frequent data collection.
- Interactive Voice Response (IVR) Systems: In some cases, patients can provide their responses over the phone by interacting with an automated system. This can be useful for patients with limited literacy or access to digital devices.
- Wearable Devices: Although still evolving, integration with wearable devices can automatically capture certain physiological data that contributes to PROs, such as activity levels or sleep patterns.
Advantages of ePRO
The implementation of ePRO systems offers significant benefits:
- Direct Patient Voice: Captures unfiltered patient experiences, providing a more authentic understanding of their condition and treatment effects.
- Reduced Reporting Bias: Minimizes potential bias introduced by healthcare professionals interpreting or recording patient symptoms.
- Increased Patient Engagement: Empowering patients to actively participate in their data recording can foster greater engagement in their healthcare journey.
- Improved Data Accuracy and Timeliness: Patients can report symptoms or events as they occur, leading to more accurate and timely data compared to retrospective recall.
- Flexibility in Data Collection: Assessments can be completed at home, while traveling, or at other convenient times for the patient.
Electronic Clinical Outcome Assessments (eCOA)
eCOA is a broader term that encompasses the electronic collection of any data that measures a clinical outcome. This includes not only patient-reported outcomes but also data collected by clinicians, raters, or other healthcare professionals.
Defining Clinical Outcome Assessments
Clinical outcome assessments (COAs) are tools used to measure the results of clinical interventions. They can evaluate a wide range of outcomes, from the effectiveness of a drug in reducing tumor size (objective measure) to the patient’s perceived improvement in daily functioning (subjective measure). COAs provide the evidence base for therapeutic claims and regulatory approvals.
The Scope of eCOA
eCOA acts as a unifying platform for various types of electronic assessments in a clinical trial. It’s like a comprehensive library where different types of books are stored and organized.
Types of Data Captured by eCOA
eCOA systems can capture data from multiple sources:
- Electronic PROs (ePROs): As discussed previously, patient-reported data is a significant component of eCOA.
- Clinician-Reported Outcome Measures (eCOs): Data collected by healthcare professionals, such as physicians, nurses, or therapists, regarding their observations and assessments of a patient’s condition. This could include physical examination findings, diagnostic test results, or assessments of disease severity.
- Observer-Reported Outcome Measures (ObsROs): Data captured by individuals other than the patient or clinician, such as a caregiver or family member, who can provide insights into the patient’s functioning or well-being.
- Performance Outcome Measures (PerfOs): Data acquired through objective performance-based tests, measuring a patient’s ability to perform specific tasks. Examples include gait analysis, cognitive function tests, or motor skill assessments.
Why eCOA is Important
The adoption of eCOA reflects a strategic approach to data collection:
- Holistic Data Capture: Provides a comprehensive view of a patient’s health status and treatment response by integrating data from multiple perspectives.
- Standardization: Promotes consistent administration and scoring of outcome measures, regardless of who is collecting the data.
- Flexibility and Adaptability: Can accommodate a wide range of assessment tools and methodologies.
- Streamlined Data Integration: Facilitates the integration of diverse data types into a central EDC system, simplifying analysis.
The Interplay Between EDC, ePRO, and eCOA
While distinct, these systems are not isolated. They often work in concert to create a robust data collection ecosystem.
How They Fit Together in a Clinical Trial
In a typical clinical trial, an EDC system serves as the master repository for all study data. Within this framework, ePRO modules or applications are used to gather patient-reported information, and eCOA tools (which may include ePROs and clinician-reported measures) capture other critical outcome data.
Imagine a symphony orchestra. The EDC system is the conductor, ensuring all sections play in harmony and at the right time. The ePRO instruments (like violins) provide the lyrical melodies of the patient’s experience, while the eCOA instruments (like brass and percussion) bring in the objective measurements and clinician observations, creating a rich and complete composition of the trial’s narrative.
Data Flow and Integration
Data collected via ePRO and other eCOA tools is typically transmitted to the central EDC system. This integration ensures that all relevant data sets are consolidated for review, analysis, and reporting. This seamless flow is crucial for efficient trial management.
The Central Role of EDC
The EDC system acts as the backbone of this data collection process. It dictates the structure, validation rules, and security protocols for all information, regardless of its origin. Without a well-designed EDC, the integration of ePRO and eCOA could become chaotic.
Advanced Features and Considerations

As these systems mature, they incorporate more sophisticated functionalities and require careful planning for implementation.
Data Validation and Quality Control
Beyond basic checks, advanced EDC systems offer sophisticated data validation algorithms that can detect complex patterns and anomalies. This proactive approach to quality control is vital for generating reliable research findings.
Security and Privacy
Ensuring the security and privacy of sensitive patient data is paramount. Researchers and system developers must adhere to stringent regulatory requirements and implement robust data encryption, authentication, and access control mechanisms. This is not merely a technical consideration but a fundamental ethical obligation.
Usability and User Experience
The success of ePRO and eCOA heavily relies on user adoption. Systems must be intuitive and easy to use for both patients and healthcare professionals. Poor usability can lead to frustration, errors, and reduced compliance. This is where thoughtful design, like an easily navigable map for a complex journey, becomes critical.
Regulatory Compliance
The implementation of EDC, ePRO, and eCOA systems must align with various regulatory guidelines, including those from the FDA, EMA, and other health authorities. Understanding and adhering to these regulations, such as the principles of Good Clinical Practice (GCP) and data privacy laws, is non-negotiable.
Interoperability
The ability of different systems to communicate and exchange data is increasingly important. Interoperability ensures that data collected from various sources can be seamlessly integrated, reducing manual effort and potential errors. This is like ensuring that different puzzle pieces from various boxes can still fit together to form the complete picture.
Implementation Challenges and Best Practices
Despite the numerous benefits, implementing these systems can present hurdles.
Challenges in Adoption
- Initial Investment: The upfront cost of acquiring and implementing EDC, ePRO, and eCOA systems can be substantial.
- Technical Infrastructure: Ensuring adequate internet connectivity and compatible devices for patients and sites is essential.
- Training and Support: Comprehensive training for all users is required to ensure proper utilization and prevent errors.
- Change Management: Overcoming resistance to change from individuals accustomed to traditional paper-based methods can be a significant hurdle.
Best Practices for Successful Implementation
- Early Planning and Needs Assessment: Thoroughly assess the specific needs of the trial and select systems that meet those requirements.
- Phased Rollout: Consider a phased implementation approach, starting with a pilot study to identify and address any issues before a full-scale deployment.
- User-Centric Design: Prioritize systems with intuitive interfaces and provide robust user support.
- Comprehensive Training Programs: Develop and deliver effective training programs tailored to different user groups.
- Ongoing Monitoring and Evaluation: Continuously monitor system performance, data quality, and user feedback to identify areas for improvement.
The Future Landscape of Data Capture
| Type of EDC System | Description | Key Features | Common Use Cases | Advantages | Limitations |
|---|---|---|---|---|---|
| Web-Based EDC | Data capture through internet browsers, hosted on cloud or private servers. | Real-time data entry, remote access, multi-user support, automated validation. | Clinical trials, surveys, registries. | Easy access, scalable, no local installation needed. | Dependent on internet connectivity, potential data security concerns. |
| Offline/Standalone EDC | Software installed locally on devices, data entered without internet connection. | Offline data entry, batch upload, local data storage. | Field studies in remote areas, disaster zones. | Works without internet, secure local data control. | Data synchronization delays, limited collaboration. |
| Mobile EDC | Data capture via smartphones or tablets using dedicated apps. | Touch interface, GPS tagging, barcode scanning, offline mode. | Point-of-care data collection, epidemiological studies. | Portability, ease of use, real-time data capture. | Device compatibility issues, battery dependency. |
| Hybrid EDC Systems | Combination of web-based and offline capabilities. | Flexible data entry modes, synchronization features. | Multi-site clinical trials, mixed connectivity environments. | Versatile, supports diverse environments. | Complex setup, higher cost. |
| Electronic Patient-Reported Outcomes (ePRO) | Specialized EDC for capturing patient self-reported data electronically. | Patient-friendly interface, reminders, compliance tracking. | Clinical trials, chronic disease management. | Improves data accuracy, enhances patient engagement. | Requires patient training, potential for user error. |
The evolution of EDC, ePRO, and eCOA is ongoing, driven by technological advancements and the increasing complexity of clinical research.
Emerging Technologies
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML are being explored for automated data cleaning, anomaly detection, and predictive analytics, further enhancing data quality and efficiency.
- Blockchain Technology: The potential for blockchain to enhance data security, transparency, and integrity in clinical trials is an area of active research.
- Decentralized Clinical Trials (DCTs): The rise of DCTs, where various trial activities are conducted remotely, further emphasizes the need for robust and accessible ePRO and eCOA solutions.
The Increasing Importance of Data Integration
As research becomes more complex and data sources diversify, the ability to integrate data from various EDC, ePRO, and eCOA platforms will become even more critical. This will enable a more holistic and comprehensive understanding of study outcomes.
Driving Innovation and Patient Centricity
Ultimately, these technologies are driving innovation in clinical research, making trials more efficient, reliable, and patient-centric. By empowering patients and providing researchers with richer, more accurate data, EDC, ePRO, and eCOA systems are shaping the future of healthcare and scientific discovery. The journey of data from a patient’s experience to a validated scientific insight is becoming more direct, transparent, and impactful, thanks to these digital tools.



