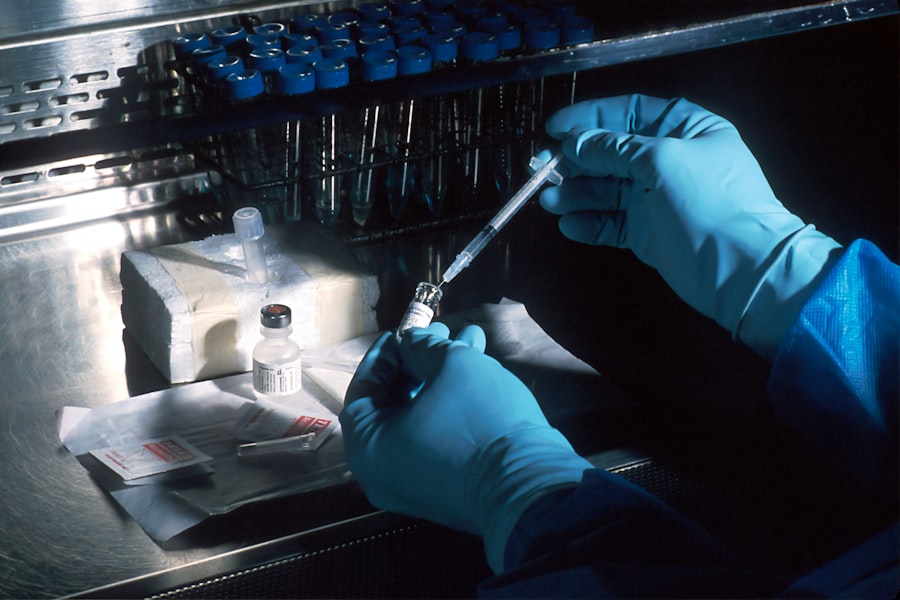
The preclinical phase of medical research serves as a critical foundation for the development of new therapies and interventions. This stage typically involves laboratory and animal studies designed to assess the safety, efficacy, and biological activity of a potential drug or treatment before it is tested in humans. Researchers utilize various models, including cell cultures and animal models, to gather preliminary data that can inform the design of clinical trials.
The preclinical phase is not merely a formality; it is a rigorous process that aims to identify any potential risks associated with a new treatment and to establish a rationale for its use in human subjects. During this phase, researchers conduct a series of experiments to evaluate pharmacokinetics (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamics (the effects of the drug on the body). For instance, if a new cancer drug is being developed, preclinical studies might involve testing its effects on tumor cells in vitro and then in vivo using animal models.
These studies help to elucidate the mechanism of action of the drug, determine optimal dosing regimens, and identify any toxicological concerns. The data generated during this phase is crucial for justifying the transition to clinical trials, as it provides the first insights into how a treatment might perform in humans.
Key Takeaways
- Preclinical research is crucial for assessing safety and efficacy before human trials begin.
- Transitioning to clinical trials faces challenges like data reliability and biological differences.
- Robust preclinical data guides the design and success of clinical trial protocols.
- Ethical and regulatory considerations are key in ensuring responsible advancement to human studies.
- Collaboration and emerging technologies are shaping future improvements in bridging preclinical and clinical research.
Challenges in Transitioning from Preclinical to Clinical Trials
Transitioning from preclinical to clinical trials presents numerous challenges that can impede the development of new therapies. One significant hurdle is the inherent variability between animal models and human physiology. While animal studies can provide valuable insights, they do not always accurately predict human responses.
For example, a drug that shows promise in mice may fail in humans due to differences in metabolism or immune response. This discrepancy can lead to costly delays and setbacks in the clinical development process. Another challenge lies in the complexity of designing clinical trials based on preclinical data.
Researchers must carefully consider factors such as patient population, dosing strategies, and endpoints that will be used to measure efficacy and safety. The transition requires not only a thorough understanding of the preclinical findings but also an ability to translate those findings into a clinical context. This often involves extensive discussions with regulatory bodies to ensure that the proposed trial design meets ethical and scientific standards.
The pressure to move quickly can sometimes lead to oversights in trial design, which can compromise the validity of the results.
Importance of Preclinical Data in Designing Clinical Trials
Preclinical data plays an indispensable role in shaping the design of clinical trials. It provides the necessary evidence to support hypotheses about how a treatment will behave in humans, guiding decisions about trial design elements such as dosage, administration routes, and patient selection criteria. For instance, if preclinical studies indicate that a drug is most effective at a specific concentration, this information will directly influence the dosing strategy employed in clinical trials.
Moreover, understanding the pharmacokinetics and pharmacodynamics from preclinical studies helps researchers anticipate potential side effects and adverse reactions. Additionally, preclinical data aids in identifying appropriate biomarkers that can be used to monitor treatment response in clinical trials. Biomarkers are biological indicators that can provide insights into disease progression or treatment efficacy.
For example, if a preclinical study reveals that a particular biomarker correlates with treatment response, this biomarker can be incorporated into the clinical trial design as an endpoint for evaluating efficacy. This integration of preclinical findings into clinical trial design not only enhances the likelihood of success but also ensures that trials are more scientifically robust.
Bridging the Gap: Strategies for Successful Transition
| Strategy | Key Metric | Measurement | Impact | Implementation Timeframe |
|---|---|---|---|---|
| Comprehensive Training Programs | Employee Readiness Score | Pre- and post-training assessments (scale 1-10) | Improves skill alignment by 40% | 3 months |
| Mentorship and Coaching | Mentorship Engagement Rate | Percentage of employees paired with mentors | Increases retention by 25% | Ongoing |
| Clear Communication Channels | Communication Effectiveness Index | Employee feedback surveys (scale 1-5) | Reduces misunderstandings by 30% | 1 month |
| Goal Alignment Workshops | Goal Clarity Percentage | Percentage of employees with clear goals | Boosts productivity by 20% | 2 months |
| Feedback and Continuous Improvement | Feedback Implementation Rate | Percentage of feedback acted upon | Enhances process efficiency by 15% | Ongoing |
To successfully bridge the gap between preclinical and clinical research, several strategies can be employed. One effective approach is the use of advanced modeling techniques that better mimic human physiology. For instance, researchers are increasingly utilizing organ-on-a-chip technology, which allows for the creation of microenvironments that replicate human organ systems.
These models can provide more accurate predictions of how a drug will behave in humans compared to traditional animal models. Another strategy involves fostering collaboration between academic institutions, industry partners, and regulatory agencies. By working together, these stakeholders can share insights and resources that enhance the quality of preclinical research and its translation into clinical settings.
Collaborative efforts can also facilitate access to larger patient populations for clinical trials, thereby increasing the statistical power of study findings. Furthermore, engaging with regulatory bodies early in the development process can help ensure that preclinical data meets the necessary standards for advancing to clinical trials.
Ethical Considerations in Moving from Preclinical to Clinical Research
Ethical considerations are paramount when transitioning from preclinical to clinical research. The primary ethical concern revolves around ensuring patient safety and informed consent. Before initiating clinical trials, researchers must demonstrate that they have thoroughly evaluated the potential risks associated with a new treatment based on preclinical data.
This includes conducting comprehensive risk-benefit analyses to ensure that the potential benefits of participating in a trial outweigh any risks involved. Informed consent is another critical ethical component. Participants must be fully aware of what their involvement entails, including potential side effects and the experimental nature of the treatment being tested.
Researchers have an ethical obligation to communicate clearly and transparently with participants about what is known from preclinical studies and what remains uncertain. This transparency fosters trust between researchers and participants and ensures that individuals are making informed decisions about their participation in clinical trials.
Regulatory Hurdles in Advancing from Preclinical to Clinical Trials

Navigating regulatory hurdles is a significant aspect of advancing from preclinical to clinical trials. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA) impose stringent requirements for data submission before granting approval for clinical trials.
These requirements often include detailed documentation of preclinical findings, including safety assessments and proposed trial designs. One common regulatory challenge is ensuring compliance with Good Laboratory Practice (GLP) standards during preclinical studies. GLP guidelines are designed to ensure that research is conducted consistently and reliably, which is essential for generating credible data that regulatory agencies will accept.
Failure to adhere to these standards can result in delays or rejections of trial applications. Additionally, regulatory agencies may require additional studies or modifications to trial designs based on their review of preclinical data, further complicating the transition process.
Role of Collaboration in Facilitating the Transition
Collaboration plays a vital role in facilitating the transition from preclinical to clinical research. By fostering partnerships among academic institutions, pharmaceutical companies, and regulatory bodies, stakeholders can leverage diverse expertise and resources to enhance research outcomes. Collaborative networks can provide access to specialized knowledge in areas such as biomarker discovery, patient recruitment strategies, and regulatory compliance.
Moreover, collaboration can help streamline processes by sharing best practices and lessons learned from previous trials. For instance, organizations may establish consortia focused on specific therapeutic areas where they can collectively address common challenges faced during the transition phase. These collaborative efforts not only enhance scientific rigor but also promote innovation by encouraging interdisciplinary approaches to problem-solving.
Future Trends in Bridging the Gap between Preclinical and Clinical Research
As medical research continues to evolve, several trends are emerging that aim to bridge the gap between preclinical and clinical research more effectively. One notable trend is the increasing use of artificial intelligence (AI) and machine learning algorithms to analyze preclinical data and predict outcomes in clinical settings. These technologies can help identify patterns within large datasets that may not be immediately apparent to researchers, thereby informing more targeted trial designs.
Another trend is the growing emphasis on patient-centric approaches in clinical trial design. Researchers are increasingly recognizing the importance of incorporating patient perspectives into trial planning, which can enhance recruitment efforts and improve retention rates. By engaging patients early in the research process and considering their preferences and experiences, researchers can design trials that are more aligned with patient needs.
Additionally, advancements in personalized medicine are reshaping how treatments are developed and tested. The ability to tailor therapies based on individual genetic profiles or specific disease characteristics allows for more precise targeting of interventions during clinical trials. This shift towards precision medicine not only enhances treatment efficacy but also minimizes unnecessary exposure to ineffective therapies.
In summary, bridging the gap between preclinical and clinical research requires a multifaceted approach that addresses scientific, ethical, regulatory, and collaborative challenges. As researchers continue to innovate and adapt their methodologies, there is hope for more efficient pathways from laboratory discoveries to effective treatments for patients.




