Clinical operations management is a critical component of healthcare systems, encompassing the planning, execution, and oversight of clinical services to ensure that patient care is delivered efficiently and effectively. This discipline integrates various functions, including patient care delivery, resource allocation, and compliance with regulatory standards. The primary goal of clinical operations management is to enhance the quality of care while optimizing operational efficiency, ultimately leading to improved patient outcomes and satisfaction.
In an era where healthcare demands are rapidly evolving due to technological advancements, demographic shifts, and changing patient expectations, the importance of robust clinical operations management cannot be overstated. Healthcare organizations are increasingly challenged to deliver high-quality services while managing costs and maintaining compliance with stringent regulations. As a result, clinical operations management has emerged as a vital area of focus for healthcare leaders seeking to navigate these complexities and drive organizational success.
Key Takeaways
- Clinical operations management focuses on optimizing healthcare delivery processes for better patient outcomes.
- Key areas for optimization include patient flow, scheduling, communication, and supply chain management.
- Technology implementation and data analytics are critical tools for enhancing efficiency and informed decision-making.
- Effective communication and collaboration among staff improve overall clinical operations performance.
- Continuous improvement strategies ensure sustainable advancements in clinical operations management.
Identifying Key Areas for Optimization
To effectively enhance clinical operations, it is essential to identify key areas that require optimization. This process begins with a comprehensive assessment of current workflows, resource utilization, and patient outcomes. By conducting a thorough analysis, healthcare organizations can pinpoint inefficiencies and bottlenecks that hinder operational performance.
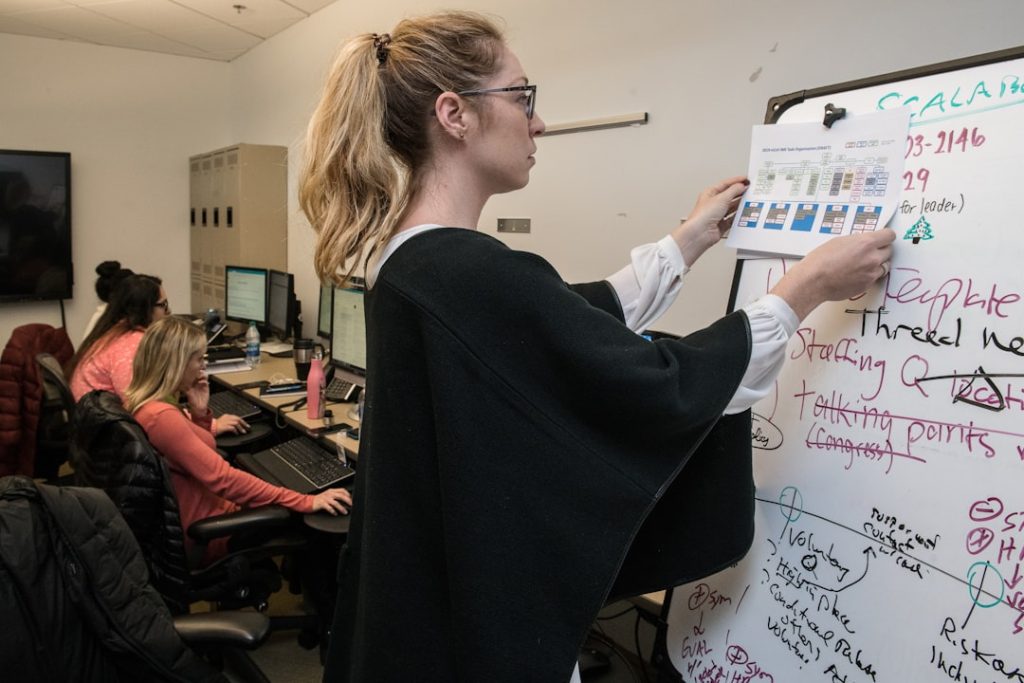
For instance, examining patient wait times, appointment scheduling processes, and staff allocation can reveal critical insights into areas that may benefit from targeted improvements. Moreover, engaging frontline staff in this evaluation process is crucial. Those who work directly with patients often have valuable perspectives on operational challenges and opportunities for enhancement.
By fostering a culture of open communication and collaboration, healthcare organizations can harness the collective expertise of their teams to identify specific areas for optimization. This collaborative approach not only empowers staff but also fosters a sense of ownership in the improvement initiatives that follow.
Streamlining Patient Flow and Scheduling

One of the most significant challenges in clinical operations is managing patient flow and scheduling effectively. Inefficient scheduling can lead to increased wait times, reduced patient satisfaction, and ultimately, compromised care quality. To address these issues, healthcare organizations can implement strategies that streamline patient flow from the moment an appointment is made until the patient leaves the facility.
One effective approach is the use of advanced scheduling algorithms that take into account various factors such as patient acuity, provider availability, and historical appointment data. These algorithms can optimize appointment slots to ensure that patients are seen in a timely manner while minimizing gaps in the schedule. Additionally, implementing a centralized scheduling system can enhance coordination among different departments and specialties, reducing the likelihood of scheduling conflicts and improving overall patient experience.
Furthermore, organizations can adopt lean principles to analyze and redesign patient flow processes. By mapping out the patient journey and identifying non-value-added steps, healthcare providers can eliminate waste and streamline operations. For example, reducing unnecessary paperwork or simplifying check-in procedures can significantly enhance the overall efficiency of patient flow.
Implementing Technology for Efficiency
| Metric | Description | Before Implementation | After Implementation | Improvement (%) |
|---|---|---|---|---|
| Process Completion Time | Average time to complete key business processes (hours) | 48 | 24 | 50% |
| Error Rate | Percentage of errors in process outputs | 12% | 4% | 66.7% |
| Employee Productivity | Tasks completed per employee per day | 15 | 22 | 46.7% |
| System Downtime | Hours of system unavailability per month | 10 | 2 | 80% |
| Customer Response Time | Average time to respond to customer inquiries (minutes) | 60 | 20 | 66.7% |
| Cost per Transaction | Operational cost per transaction processed | 5.00 | 3.00 | 40% |
The integration of technology into clinical operations management has revolutionized the way healthcare organizations function. Electronic health records (EHRs), telemedicine platforms, and practice management software are just a few examples of technological advancements that have improved operational efficiency. EHRs facilitate seamless access to patient information, enabling providers to make informed decisions quickly and reducing the risk of errors associated with paper-based records.
Telemedicine has also emerged as a powerful tool for enhancing efficiency in clinical operations. By allowing patients to consult with healthcare providers remotely, telemedicine reduces the burden on physical facilities and optimizes resource utilization. This approach not only improves access to care for patients but also allows providers to manage their time more effectively by minimizing travel-related delays.
Moreover, automation technologies such as robotic process automation (RPA) can streamline administrative tasks within clinical operations. RPA can handle repetitive tasks such as appointment reminders, billing processes, and data entry, freeing up staff to focus on more complex responsibilities that require human intervention. By leveraging technology in these ways, healthcare organizations can enhance operational efficiency while maintaining high standards of patient care.
Improving Communication and Collaboration
Effective communication and collaboration are fundamental to successful clinical operations management. In a healthcare setting where multiple stakeholders are involved—ranging from physicians and nurses to administrative staff and patients—clear communication channels are essential for ensuring that everyone is aligned toward common goals. Poor communication can lead to misunderstandings, errors in patient care, and decreased morale among staff.
To foster better communication within clinical teams, organizations can implement regular interdisciplinary meetings where staff from various departments come together to discuss challenges, share insights, and collaborate on solutions. These meetings create an environment where team members feel valued and empowered to contribute their ideas. Additionally, utilizing communication tools such as secure messaging platforms can facilitate real-time information sharing among team members, enhancing coordination in patient care delivery.
Collaboration extends beyond internal teams; it also involves engaging patients in their care journey. Encouraging open dialogue between providers and patients fosters trust and ensures that patients are active participants in their treatment plans. By providing patients with access to their health information through patient portals or mobile applications, healthcare organizations can empower individuals to take charge of their health while improving overall communication between patients and providers.
Enhancing Inventory and Supply Chain Management

Effective inventory and supply chain management are crucial components of clinical operations management that directly impact cost control and service delivery. Healthcare organizations must ensure that they have the right supplies available at the right time without overstocking or understocking items. This balance is particularly challenging given the unpredictable nature of patient demand and the complexities of managing diverse inventories across multiple departments.
Implementing inventory management systems that utilize real-time tracking technology can significantly enhance supply chain efficiency. These systems allow organizations to monitor stock levels continuously, automate reordering processes, and reduce waste associated with expired or unused supplies. For example, using barcode scanning technology can streamline inventory audits and ensure accurate tracking of supplies throughout the facility.
Additionally, establishing strong relationships with suppliers is essential for optimizing supply chain management. Collaborative partnerships can lead to better pricing agreements, improved delivery schedules, and enhanced responsiveness to changing needs. By working closely with suppliers to forecast demand based on historical data and upcoming procedures, healthcare organizations can create a more agile supply chain that adapts to fluctuations in patient volume.
Utilizing Data Analytics for Decision Making
Data analytics has become an indispensable tool in clinical operations management, enabling healthcare organizations to make informed decisions based on empirical evidence rather than intuition alone. By harnessing data from various sources—such as EHRs, patient surveys, and operational metrics—organizations can gain valuable insights into performance trends, patient outcomes, and areas for improvement. For instance, predictive analytics can be employed to forecast patient admissions based on historical data patterns.
This information allows organizations to allocate resources more effectively by anticipating peak times for patient volume and adjusting staffing levels accordingly. Additionally, analyzing patient feedback through surveys can help identify specific areas where care delivery may be lacking, guiding targeted improvement initiatives. Moreover, data analytics can support quality improvement efforts by tracking key performance indicators (KPIs) related to clinical outcomes and operational efficiency.
By regularly monitoring these metrics, healthcare organizations can identify trends over time and assess the impact of implemented changes on overall performance. This data-driven approach fosters a culture of accountability and continuous improvement within clinical operations.
Strategies for Continuous Improvement and Sustainability
Continuous improvement is a fundamental principle in clinical operations management that emphasizes the need for ongoing evaluation and refinement of processes. To cultivate a culture of continuous improvement, healthcare organizations must establish frameworks that encourage innovation and adaptability among staff at all levels. One effective strategy is the implementation of Plan-Do-Study-Act (PDSA) cycles, which provide a structured approach for testing changes on a small scale before broader implementation.
This iterative process allows teams to assess the effectiveness of new initiatives while minimizing disruption to existing workflows. For example, if a new scheduling protocol is introduced, teams can pilot it in one department before rolling it out organization-wide based on feedback and results. Sustainability is another critical aspect of continuous improvement in clinical operations management.
Organizations must consider not only immediate operational efficiencies but also long-term sustainability in terms of resource utilization and environmental impact. Implementing green practices—such as reducing waste through recycling programs or optimizing energy consumption—can contribute to both cost savings and enhanced community reputation. By fostering a culture that values continuous improvement and sustainability, healthcare organizations position themselves for long-term success in an ever-evolving landscape.
Embracing change as an opportunity rather than a challenge enables organizations to remain agile in responding to emerging trends while consistently delivering high-quality care to patients.