Central Nervous System (CNS) clinical trials are pivotal in advancing our understanding and treatment of neurological and psychiatric disorders. These trials encompass a wide range of conditions, including Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, epilepsy, and various mood disorders. The complexity of the CNS, characterized by its intricate network of neurons and glial cells, presents unique challenges for researchers.
The brain’s protective barriers, such as the blood-brain barrier, complicate drug delivery and efficacy, making the design and execution of clinical trials particularly demanding. As a result, CNS clinical trials often require innovative methodologies and a multidisciplinary approach to address the multifaceted nature of these disorders. The significance of CNS clinical trials cannot be overstated.
They not only contribute to the development of new therapeutic agents but also enhance our understanding of disease mechanisms. By investigating the efficacy and safety of potential treatments, these trials play a crucial role in translating laboratory discoveries into clinical practice. Furthermore, they provide valuable insights into patient populations, disease progression, and treatment responses, which are essential for tailoring personalized medicine approaches.
As the global burden of CNS disorders continues to rise, the urgency for effective interventions underscores the importance of robust clinical trial frameworks.
Key Takeaways
- CNS clinical trials are evolving with significant technological and therapeutic innovations.
- Patient-centric approaches are increasingly prioritized to improve trial outcomes and participant experience.
- Regulatory frameworks are adapting to support novel CNS therapies and trial methodologies.
- Advances in biomarkers and imaging techniques enhance diagnosis, monitoring, and treatment evaluation.
- Despite challenges, future CNS trials hold promise through integrated technologies and personalized medicine.
Technological Advancements in CNS Clinical Trials
Recent years have witnessed remarkable technological advancements that have transformed the landscape of CNS clinical trials. One of the most significant developments is the integration of digital health technologies, including wearable devices and mobile health applications. These tools enable continuous monitoring of patients’ neurological functions and behavioral patterns outside traditional clinical settings.
For instance, wearable sensors can track movement patterns in Parkinson’s disease patients, providing real-time data that can be used to assess treatment efficacy and disease progression. This shift towards remote monitoring not only enhances data collection but also improves patient engagement and adherence to study protocols. Moreover, artificial intelligence (AI) and machine learning are increasingly being utilized to analyze complex datasets generated from CNS trials.
These technologies can identify patterns and correlations that may not be apparent through conventional statistical methods. For example, AI algorithms can analyze neuroimaging data to predict treatment responses in patients with depression or anxiety disorders. By harnessing the power of big data, researchers can refine patient selection criteria, optimize trial designs, and ultimately improve the likelihood of successful outcomes.
The convergence of technology and neuroscience is paving the way for more efficient and effective clinical trials in the CNS domain.
Innovative Therapies in CNS Clinical Trials
The exploration of innovative therapies in CNS clinical trials has gained momentum as researchers seek to address unmet medical needs in this field. One notable area of focus is gene therapy, which holds promise for treating genetic disorders affecting the CNS. For instance, recent trials investigating adeno-associated virus (AAV)-based gene therapies have shown potential in treating conditions like spinal muscular atrophy (SMA) and certain forms of inherited blindness.
By delivering therapeutic genes directly to affected neurons, these approaches aim to restore normal function at a molecular level, offering hope for patients with previously untreatable conditions. Another exciting avenue is the development of monoclonal antibodies targeting specific pathological processes in neurodegenerative diseases. For example, amyloid-beta-targeting antibodies have been at the forefront of Alzheimer’s disease research.
Clinical trials evaluating drugs like aducanumab have sparked significant debate regarding their efficacy and safety profiles. Despite mixed results, these therapies represent a paradigm shift in how we approach neurodegeneration, moving from symptomatic treatment to targeting underlying disease mechanisms. The ongoing exploration of innovative therapies underscores the dynamic nature of CNS clinical research and its potential to revolutionize patient care.
Patient-Centric Approaches in CNS Clinical Trials
In recent years, there has been a growing recognition of the importance of patient-centric approaches in CNS clinical trials. Traditionally, clinical research has often been conducted with a top-down perspective, where researchers dictate study parameters without sufficient input from patients. However, involving patients in the design and execution of trials can lead to more relevant outcomes and improved recruitment and retention rates.
For instance, initiatives that incorporate patient feedback on trial protocols can help identify barriers to participation and enhance the overall experience for participants. Furthermore, patient-centric approaches extend beyond trial design to encompass communication strategies throughout the study process. Clear and transparent communication about trial objectives, potential risks, and expected outcomes is essential for fostering trust between researchers and participants.
Engaging patients as partners in research not only empowers them but also enriches the data collected during trials. By prioritizing patient perspectives, researchers can ensure that clinical trials are more aligned with the needs and preferences of those affected by CNS disorders.
Regulatory Developments in CNS Clinical Trials
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of Active CNS Clinical Trials | Total ongoing clinical trials focused on central nervous system disorders | 1,250 | Trials |
| Most Common CNS Indication | Disorder most frequently studied in CNS clinical trials | Alzheimer’s Disease | – |
| Average Trial Duration | Mean length of CNS clinical trials from start to completion | 24 | Months |
| Phase Distribution | Percentage of trials by clinical phase | Phase 1: 30%, Phase 2: 40%, Phase 3: 25%, Phase 4: 5% | Percentage |
| Enrollment Size | Average number of participants per CNS clinical trial | 150 | Participants |
| Top Recruiting Country | Country with the highest number of CNS clinical trial sites | United States | – |
| Common Intervention Type | Most frequently used intervention in CNS trials | Pharmacological | – |
The regulatory landscape governing CNS clinical trials has evolved significantly in response to advancements in science and technology. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) have recognized the need for adaptive trial designs that allow for flexibility in response to emerging data.
This approach is particularly relevant in CNS research, where patient populations can be heterogeneous, and treatment responses may vary widely. Adaptive designs enable researchers to modify trial parameters based on interim results, potentially accelerating the development timeline for promising therapies. Additionally, regulatory frameworks are increasingly accommodating innovative methodologies such as real-world evidence (RWE) and digital health technologies.
The FDA has issued guidance on incorporating RWE into regulatory decision-making processes, acknowledging its potential to complement traditional clinical trial data. This shift reflects a broader understanding that real-world data can provide valuable insights into treatment effectiveness and safety in diverse patient populations. As regulatory agencies continue to adapt to the evolving landscape of CNS research, they play a crucial role in facilitating the development of novel therapies while ensuring patient safety.
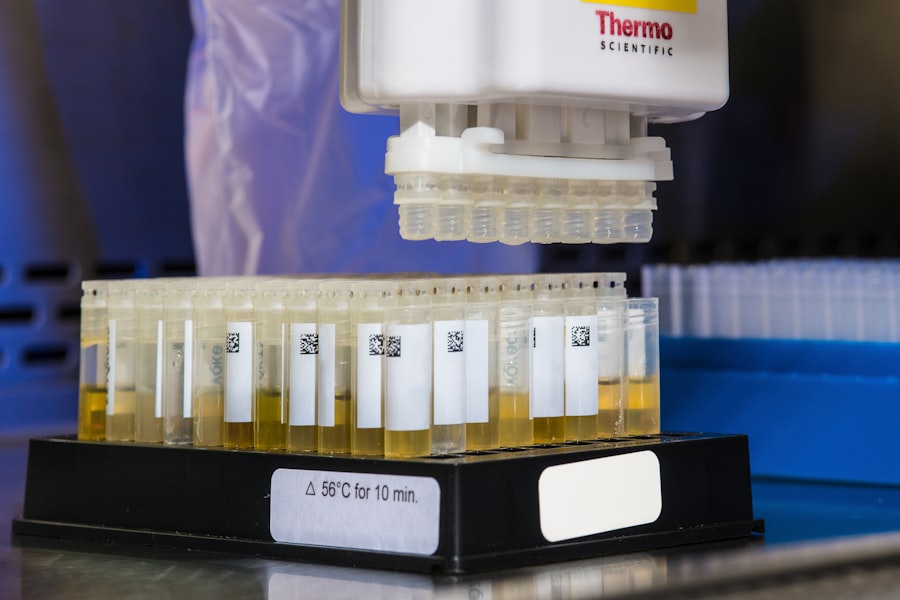
Advancements in Biomarkers and Imaging Techniques in CNS Clinical Trials

The identification and validation of biomarkers have become integral components of CNS clinical trials, offering insights into disease mechanisms and treatment responses. Biomarkers can serve as objective measures of disease progression or therapeutic efficacy, enabling more precise patient stratification in clinical studies. For instance, neurofilament light chain (NfL) has emerged as a promising biomarker for neurodegenerative diseases such as Alzheimer’s and multiple sclerosis.
Elevated levels of NfL in cerebrospinal fluid or blood correlate with neuronal damage and disease activity, making it a valuable tool for monitoring treatment effects. In parallel with biomarker development, advancements in imaging techniques have revolutionized our ability to visualize brain structure and function in real time. Techniques such as functional magnetic resonance imaging (fMRI) allow researchers to assess brain activity associated with specific cognitive tasks or emotional responses.
This capability is particularly relevant in psychiatric disorders where understanding neural correlates of symptoms is crucial for developing targeted interventions. The integration of biomarkers with advanced imaging modalities enhances our understanding of CNS disorders and facilitates more informed decision-making in clinical trial design.
Challenges and Opportunities in CNS Clinical Trials
Despite the progress made in CNS clinical trials, several challenges persist that can hinder research efforts. One significant obstacle is the recruitment and retention of participants, particularly in studies involving rare neurological conditions or specific subpopulations. The complexity of these disorders often necessitates stringent inclusion criteria that can limit eligible participants.
Additionally, patients may face logistical barriers such as travel requirements or time commitments that deter participation. Addressing these challenges requires innovative strategies that prioritize accessibility and convenience for participants. Conversely, these challenges also present opportunities for improvement within the field.
The rise of telemedicine has opened new avenues for conducting CNS clinical trials by allowing remote consultations and monitoring. This approach can enhance patient engagement while reducing barriers associated with traditional trial participation. Furthermore, leveraging community partnerships can facilitate outreach efforts to underrepresented populations, ensuring that diverse voices are included in research initiatives.
By embracing these opportunities, researchers can enhance the robustness and generalizability of findings from CNS clinical trials.
Future Directions in CNS Clinical Trials
Looking ahead, the future of CNS clinical trials is poised for transformative changes driven by ongoing advancements in technology, science, and regulatory frameworks. One promising direction is the continued integration of artificial intelligence into trial design and analysis processes. AI algorithms can streamline patient recruitment by identifying suitable candidates from electronic health records or predicting treatment responses based on historical data.
This capability not only accelerates trial timelines but also enhances the precision with which therapies are developed. Moreover, as our understanding of the human microbiome’s influence on brain health expands, future CNS trials may explore gut-brain interactions as potential therapeutic targets. The interplay between gut microbiota and neurological function presents an exciting frontier for research that could lead to novel interventions for conditions like depression or anxiety disorders.
Additionally, ongoing efforts to develop personalized medicine approaches will likely shape future trial designs by focusing on tailoring treatments based on individual genetic profiles or biomarker signatures. In conclusion, CNS clinical trials are at a critical juncture where technological advancements, innovative therapies, patient-centric approaches, regulatory developments, biomarker discoveries, and emerging challenges converge to shape their future trajectory. As researchers continue to navigate this complex landscape, their efforts hold immense potential for improving outcomes for individuals affected by neurological and psychiatric disorders worldwide.




