In the realm of clinical trials, the integration of technology has revolutionized the way researchers manage and monitor their studies. One of the most significant advancements in this area is the Interactive Response Technology (IRT) system. IRT systems facilitate real-time data collection and management, enabling researchers to streamline processes such as randomization, drug supply management, and patient enrollment.
By automating these critical components, IRT systems not only enhance operational efficiency but also contribute to the overall integrity of clinical trials. As the demand for more sophisticated and efficient trial management solutions grows, understanding the role and impact of IRT systems becomes increasingly essential. The implementation of IRT systems in clinical trials is not merely a technological upgrade; it represents a paradigm shift in how clinical research is conducted.
These systems allow for dynamic interaction between trial sites, sponsors, and patients, fostering a more collaborative environment. The ability to access real-time data means that researchers can make informed decisions quickly, addressing issues as they arise and adapting protocols to better meet the needs of participants. This responsiveness is crucial in maintaining patient safety and ensuring that trials adhere to regulatory standards.
As we delve deeper into the significance of patient outcomes and the role of IRT systems, it becomes clear that these technologies are pivotal in shaping the future of clinical research.
Key Takeaways
- IRT systems play a crucial role in managing clinical trial logistics and enhancing patient outcomes.
- Effective use of IRT systems can streamline patient randomization, drug supply, and data collection.
- Implementing strategic approaches with IRT systems leads to improved patient adherence and trial efficiency.
- Case studies demonstrate successful outcomes when IRT systems are integrated thoughtfully into clinical trials.
- Overcoming challenges in IRT system utilization is essential for maximizing their impact on patient outcomes and future trial success.
The Importance of Patient Outcomes in Clinical Trials
Patient outcomes are at the heart of clinical trials, serving as the ultimate measure of a treatment’s efficacy and safety. The focus on patient-centered outcomes has gained momentum in recent years, driven by a growing recognition that clinical research should prioritize the experiences and well-being of participants. This shift is not only ethical but also practical; understanding how a treatment impacts patients’ lives can provide invaluable insights that go beyond traditional clinical endpoints.
For instance, measuring quality of life, symptom relief, and functional status can offer a more comprehensive view of a treatment’s benefits. Moreover, regulatory agencies such as the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) are increasingly emphasizing the importance of patient-reported outcomes (PROs) in clinical trial design. By incorporating PROs into trial protocols, researchers can capture data that reflects patients’ perspectives on their health status and treatment experiences.
This approach not only enhances the relevance of trial findings but also fosters greater patient engagement and adherence to study protocols. As a result, focusing on patient outcomes can lead to more successful trials and ultimately improve the quality of care provided to patients.
Understanding the Role of IRT Systems in Clinical Trials
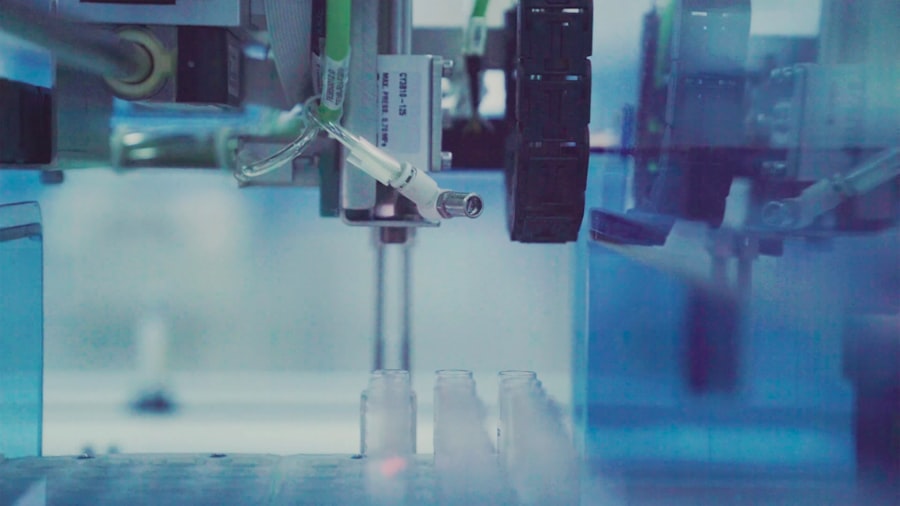
IRT systems play a multifaceted role in clinical trials, serving as a backbone for various operational processes. At their core, these systems facilitate randomization, ensuring that participants are assigned to treatment groups in a manner that minimizes bias. This is crucial for maintaining the scientific validity of a trial.
Additionally, IRT systems manage drug supply logistics, tracking inventory levels and ensuring that trial sites have access to the necessary medications when needed. This capability is particularly important in multi-site trials where coordination can be complex. Furthermore, IRT systems enhance data collection by providing real-time access to participant information and trial metrics.
This immediacy allows researchers to monitor patient enrollment rates, adherence to protocols, and adverse events as they occur. By having this information at their fingertips, clinical trial teams can make timely adjustments to study designs or operational strategies, ultimately improving patient outcomes. The integration of IRT systems also supports regulatory compliance by maintaining accurate records and facilitating audits, thereby reinforcing the integrity of the trial process.
Strategies for Improving Patient Outcomes with IRT Systems
To leverage IRT systems effectively for enhancing patient outcomes, several strategies can be employed. First and foremost is the customization of IRT solutions to align with specific trial objectives and patient populations. By tailoring the system to meet the unique needs of a study, researchers can ensure that data collection methods are relevant and that patient interactions are streamlined.
For example, incorporating user-friendly interfaces for patients can facilitate better engagement and adherence to study protocols. Another strategy involves utilizing data analytics capabilities within IRT systems to identify trends and patterns that may impact patient outcomes. By analyzing real-time data on patient responses and treatment effects, researchers can gain insights into which interventions are most effective for specific subgroups.
This information can inform adaptive trial designs, allowing for modifications based on interim results. Additionally, proactive communication with participants through IRT platforms can enhance their experience by providing timely updates on trial progress and addressing any concerns they may have.
Case Studies: Successful Implementation of IRT Systems in Clinical Trials
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of Participants | Total enrolled subjects in the IRT system clinical trial | 250 | Participants |
| Trial Duration | Length of the clinical trial period | 12 | Months |
| Randomization Rate | Percentage of participants randomized using the IRT system | 100 | % |
| Data Entry Accuracy | Accuracy rate of data entered into the IRT system | 99.5 | % |
| Drug Supply Management Efficiency | Percentage of on-time drug shipments managed by the IRT system | 98 | % |
| Adverse Event Reporting Time | Average time to report adverse events via the IRT system | 2 | Hours |
| System Downtime | Total downtime experienced by the IRT system during the trial | 1.5 | Hours |
| Protocol Compliance Rate | Percentage of protocol adherence monitored through the IRT system | 97 | % |
Several case studies illustrate the successful implementation of IRT systems in clinical trials, showcasing their impact on patient outcomes. One notable example is a large-scale oncology trial that utilized an IRT system to manage randomization and drug supply across multiple sites. By automating these processes, the trial was able to reduce enrollment timelines significantly while maintaining rigorous adherence to protocol requirements.
The real-time data access allowed researchers to monitor patient responses closely, leading to timely adjustments in treatment regimens that ultimately improved overall survival rates. Another compelling case involved a cardiovascular study where an IRT system was employed to track patient-reported outcomes alongside clinical endpoints. By integrating PRO measures into the IRT platform, researchers were able to capture valuable insights into patients’ quality of life throughout the trial.
This dual approach not only enriched the data collected but also fostered greater patient engagement, as participants felt their experiences were being valued and considered in the research process. The findings from this study highlighted the importance of addressing both clinical and patient-centered outcomes in evaluating treatment efficacy.
Overcoming Challenges in Utilizing IRT Systems for Improved Patient Outcomes
Despite their numerous advantages, implementing IRT systems in clinical trials is not without challenges. One significant hurdle is ensuring that all stakeholders—researchers, site staff, and patients—are adequately trained to use these systems effectively. A lack of familiarity with technology can lead to errors in data entry or miscommunication regarding trial protocols, ultimately jeopardizing patient safety and study integrity.
To mitigate this risk, comprehensive training programs should be developed that cater to different user groups, ensuring that everyone involved is confident in navigating the IRT system. Another challenge lies in data integration from various sources within a clinical trial ecosystem. Often, IRT systems must interface with electronic health records (EHRs), laboratory information management systems (LIMS), and other databases to provide a holistic view of patient data.
Ensuring seamless integration can be complex and may require significant technical expertise. To address this issue, organizations should invest in robust IT infrastructure and collaborate with experienced vendors who specialize in system integration. By prioritizing these efforts, researchers can enhance data accuracy and accessibility, ultimately leading to improved patient outcomes.
The Future of IRT Systems in Clinical Trials and Patient Outcomes
Looking ahead, the future of IRT systems in clinical trials appears promising as technological advancements continue to evolve. One emerging trend is the incorporation of artificial intelligence (AI) and machine learning algorithms into IRT platforms. These technologies have the potential to enhance data analysis capabilities significantly, allowing researchers to identify patterns and predict outcomes with greater accuracy.
For instance, AI-driven analytics could enable real-time risk assessments for patients based on their individual characteristics and treatment responses. Additionally, as telemedicine becomes more prevalent, integrating remote monitoring capabilities into IRT systems could further improve patient outcomes. By allowing researchers to collect data from patients’ homes through wearable devices or mobile applications, trials can capture more comprehensive information about treatment effects in real-world settings.
This shift towards decentralized clinical trials not only enhances patient convenience but also broadens participation by reducing geographical barriers.
Best Practices for Implementing IRT Systems to Improve Patient Outcomes
To maximize the benefits of IRT systems in clinical trials and enhance patient outcomes effectively, several best practices should be considered. First, involving patients early in the design process can provide valuable insights into their needs and preferences regarding technology use. This participatory approach ensures that IRT systems are user-friendly and aligned with patients’ expectations.
Moreover, continuous monitoring and evaluation of IRT system performance are essential for identifying areas for improvement. Regular feedback from users can inform updates and refinements that enhance functionality and usability over time. Finally, fostering collaboration among all stakeholders—researchers, site staff, patients, and technology providers—can create a supportive environment that prioritizes patient outcomes throughout the clinical trial process.
By embracing these best practices and leveraging the capabilities of IRT systems effectively, researchers can pave the way for more successful clinical trials that prioritize patient well-being while advancing medical knowledge and treatment options.




