Investigational Device Exemptions (IDE) represent a critical component in the landscape of medical device development and clinical research. An IDE allows for the use of investigational medical devices in clinical studies to collect safety and effectiveness data, which is essential for regulatory approval. This regulatory pathway is overseen by the U.S.
Food and Drug Administration (FDA) and is designed to facilitate innovation while ensuring patient safety. The IDE process is particularly significant for devices that are novel or have not yet been widely tested in human subjects, allowing researchers to gather necessary data that can lead to breakthroughs in medical technology. The importance of IDE medical devices cannot be overstated, as they often serve as the bridge between laboratory research and clinical application.
These devices can range from cutting-edge surgical instruments to advanced diagnostic tools, each with the potential to transform patient care. The IDE process not only provides a framework for evaluating new technologies but also encourages collaboration among manufacturers, researchers, and healthcare providers. By fostering an environment where innovative ideas can be tested and refined, IDE medical devices play a pivotal role in advancing healthcare solutions.
Key Takeaways
- IDE medical devices offer innovative solutions that enhance diagnostic and therapeutic capabilities in healthcare.
- They significantly improve patient care by enabling more accurate, timely, and personalized treatments.
- The future of IDE devices promises greater integration with AI and remote monitoring technologies.
- Challenges include regulatory hurdles, ethical concerns, and ensuring device safety and efficacy.
- Successful case studies demonstrate the transformative potential of IDE devices in clinical practice.
Advantages of IDE Medical Devices in Healthcare
One of the primary advantages of IDE medical devices is their ability to accelerate the development of new technologies that can significantly improve patient outcomes. By allowing for early-stage clinical trials, the IDE process enables researchers to gather real-world data on device performance and safety. This data is invaluable, as it helps identify potential issues before a device reaches the market, ultimately leading to safer and more effective products.
For instance, a novel stent designed for patients with coronary artery disease may undergo rigorous testing under an IDE, allowing researchers to assess its efficacy compared to existing options. Moreover, IDE medical devices often provide healthcare professionals with access to cutting-edge technology that may not yet be available through traditional channels. This access can lead to improved treatment options for patients who may have limited alternatives.
For example, a new type of implantable device for managing chronic pain could be made available through an IDE study, offering hope to patients who have exhausted other treatment avenues. The ability to participate in clinical trials also empowers patients, giving them a sense of agency in their healthcare journey while contributing to the advancement of medical science.
The Impact of IDE Medical Devices on Patient Care
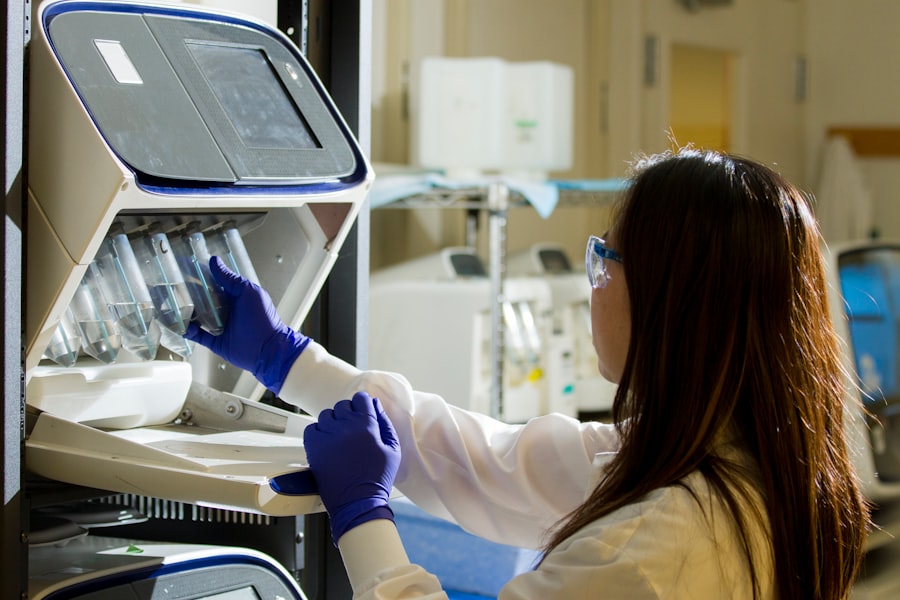
The impact of IDE medical devices on patient care is profound and multifaceted. These devices often lead to enhanced diagnostic capabilities, allowing for earlier detection and intervention in various medical conditions. For instance, an investigational imaging device that utilizes advanced algorithms may provide more accurate assessments of tumors, enabling oncologists to tailor treatment plans more effectively.
This early intervention can be crucial in improving survival rates and quality of life for patients facing serious illnesses. Additionally, IDE medical devices can facilitate personalized medicine approaches, where treatments are tailored to individual patient needs based on specific characteristics or genetic profiles. For example, a new wearable device designed to monitor glucose levels in real-time could be tested under an IDE framework, providing diabetic patients with more precise data to manage their condition.
This level of personalization not only enhances patient engagement but also fosters better adherence to treatment regimens, ultimately leading to improved health outcomes.
The Future of IDE Medical Devices in Healthcare
Looking ahead, the future of IDE medical devices appears promising as technological advancements continue to reshape the healthcare landscape. Innovations such as artificial intelligence (AI), machine learning, and telemedicine are poised to play significant roles in the development and implementation of new devices. For instance, AI-driven diagnostic tools could be tested under the IDE framework, allowing for rapid iteration and refinement based on real-world performance data.
This could lead to faster approvals and wider adoption of effective technologies. Furthermore, as the demand for personalized healthcare solutions grows, IDE medical devices will likely become increasingly integral in developing tailored therapies. The integration of genomics and biotechnology into device design will enable researchers to create solutions that address specific patient populations or conditions more effectively.
As these trends continue to evolve, the collaboration between regulatory bodies, manufacturers, and healthcare providers will be essential in ensuring that IDE medical devices meet both safety standards and patient needs.
Challenges and Limitations of IDE Medical Devices
| Metric | Description | Typical Values | Notes |
|---|---|---|---|
| Device Type | Classification of the IDE medical device | Class I, II, III | Based on risk and regulatory requirements |
| Approval Time | Time taken for Investigational Device Exemption approval | 30 to 75 days | Varies by FDA review process |
| Clinical Trial Duration | Length of clinical study under IDE | 6 months to 3 years | Depends on device complexity and endpoints |
| Number of Subjects | Participants enrolled in IDE clinical trial | 20 to 1000+ | Varies by study design and device type |
| Adverse Event Rate | Percentage of subjects experiencing adverse events | 0.1% to 10% | Monitored closely during trials |
| Success Rate | Percentage of devices meeting primary endpoints | 70% to 95% | Depends on device and trial design |
| Post-Approval Study Requirement | Whether FDA requires additional studies after approval | Yes / No | Often required for high-risk devices |
Despite their advantages, IDE medical devices face several challenges and limitations that can hinder their development and implementation. One significant challenge is the complexity of the regulatory process itself. Navigating the requirements set forth by the FDA can be daunting for manufacturers, particularly smaller companies with limited resources.
The need for extensive documentation, data collection, and compliance with stringent guidelines can slow down the progress of innovative devices from concept to clinical trial. Additionally, there are inherent risks associated with testing new devices on human subjects. While clinical trials are designed to assess safety and efficacy, unforeseen complications can arise during testing phases.
For example, a device that shows promise in preclinical studies may not perform as expected in a diverse patient population due to variations in individual responses. These challenges underscore the importance of robust study designs and thorough risk assessments throughout the IDE process.
Regulatory and Ethical Considerations for IDE Medical Devices

The regulatory landscape surrounding IDE medical devices is complex and multifaceted, requiring careful navigation by manufacturers and researchers alike. The FDA’s oversight ensures that investigational devices are subjected to rigorous evaluation before they can be marketed. This includes not only assessing the safety and effectiveness of the device but also considering ethical implications related to patient consent and data privacy.
Researchers must ensure that participants are fully informed about the risks and benefits associated with their involvement in clinical trials. Ethical considerations extend beyond informed consent; they also encompass issues related to equitable access to investigational devices. As new technologies emerge through the IDE process, it is crucial to address disparities in access among different patient populations.
Ensuring that diverse groups are represented in clinical trials is essential for generating data that is applicable across various demographics. This commitment to inclusivity not only enhances the validity of research findings but also promotes fairness in healthcare delivery.
Case Studies of Successful Implementation of IDE Medical Devices
Several case studies illustrate the successful implementation of IDE medical devices and their transformative impact on patient care. One notable example is the use of investigational cardiac devices designed for patients with heart failure. In a recent clinical trial under an IDE, a novel left ventricular assist device (LVAD) demonstrated significant improvements in survival rates compared to traditional treatment options.
Patients who received this investigational device experienced enhanced quality of life and reduced hospitalizations due to heart-related complications. Another compelling case involves an investigational drug-eluting stent that was tested under an IDE framework. This stent was designed to release medication gradually over time, reducing the risk of restenosis (re-narrowing of blood vessels).
Clinical trials showed that patients who received this stent had lower rates of complications compared to those treated with standard stents. The successful outcomes from these trials not only led to FDA approval but also paved the way for broader adoption of similar technologies in cardiovascular care.
The Role of IDE Medical Devices in Revolutionizing Healthcare
IDE medical devices are at the forefront of revolutionizing healthcare by facilitating innovation while ensuring patient safety through rigorous testing protocols. Their ability to provide access to cutting-edge technologies has transformed patient care across various medical fields, from cardiology to oncology. As we look toward the future, it is clear that these devices will continue to play a pivotal role in shaping personalized medicine and improving health outcomes.
However, navigating the challenges associated with regulatory processes and ethical considerations remains essential for maximizing the potential of IDE medical devices. By fostering collaboration among stakeholders and prioritizing inclusivity in clinical trials, we can ensure that these innovations benefit all patients equitably. As we continue to explore new frontiers in medical technology, IDE medical devices will undoubtedly remain a cornerstone of progress in healthcare delivery.




