Clinical research serves as the backbone of medical advancement, providing the necessary framework for understanding diseases, developing new treatments, and improving patient care. It encompasses a wide array of studies, including clinical trials, observational studies, and epidemiological research, all aimed at generating evidence that can inform clinical practice. The primary goal of clinical research is to evaluate the safety and efficacy of new interventions, whether they be drugs, devices, or therapeutic procedures.
This rigorous process not only helps in the development of innovative therapies but also ensures that existing treatments are continually assessed for their effectiveness and safety. The significance of clinical research extends beyond the confines of laboratories and hospitals; it has profound implications for public health policy and healthcare systems worldwide. By systematically investigating health-related questions, clinical research contributes to the body of knowledge that shapes clinical guidelines and informs healthcare decisions.
The process is inherently collaborative, involving a diverse range of stakeholders, including researchers, healthcare professionals, regulatory bodies, and patients. As the landscape of healthcare evolves, so too does the field of clinical research, adapting to new challenges and opportunities that arise in the quest for improved health outcomes.
Key Takeaways
- Clinical research is evolving with the integration of emerging technologies enhancing study efficiency.
- Advanced data analysis methods improve the accuracy and interpretation of clinical trial results.
- Ethical considerations remain central to protecting patient rights and ensuring research integrity.
- Collaborations among institutions and stakeholders foster innovation and resource sharing in clinical studies.
- Future trends emphasize patient-centered approaches and adapting to regulatory changes for better outcomes.
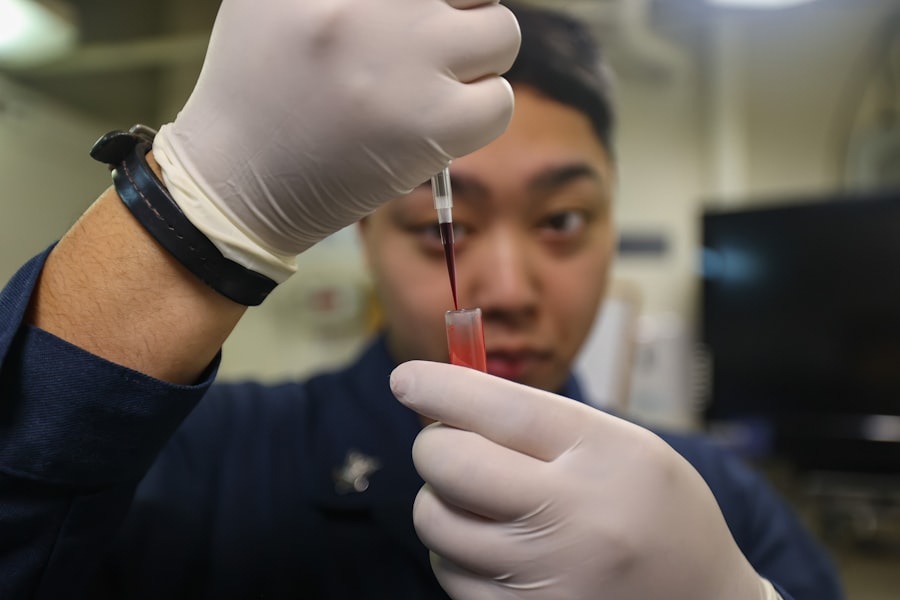
Emerging Technologies in Clinical Research
The integration of emerging technologies into clinical research is revolutionizing how studies are designed, conducted, and analyzed. One of the most significant advancements is the use of digital health technologies, such as wearable devices and mobile health applications. These tools enable real-time data collection from patients, allowing researchers to monitor health metrics continuously and gather insights that were previously unattainable.
For instance, wearable devices can track vital signs, physical activity levels, and even sleep patterns, providing a comprehensive view of a patient’s health status over time. This shift towards remote monitoring not only enhances data accuracy but also increases patient engagement by allowing individuals to take an active role in their health management. Artificial intelligence (AI) and machine learning are also making substantial inroads into clinical research.
These technologies can analyze vast amounts of data at unprecedented speeds, identifying patterns and correlations that may elude human researchers. For example, AI algorithms can sift through electronic health records to identify potential candidates for clinical trials based on specific inclusion criteria, streamlining the recruitment process. Additionally, predictive analytics powered by machine learning can help researchers forecast patient responses to treatments, enabling more personalized approaches to therapy.
As these technologies continue to evolve, they hold the promise of transforming clinical research into a more efficient and effective endeavor.
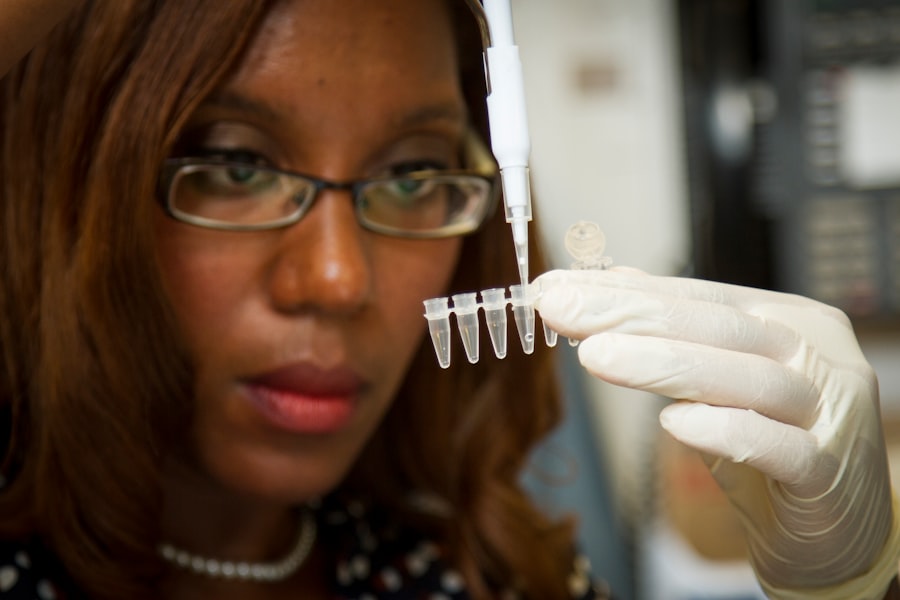
Advancements in Data Analysis and Interpretation
The ability to analyze and interpret data effectively is crucial in clinical research, as it directly impacts the validity and reliability of study findings. Recent advancements in statistical methodologies and computational tools have significantly enhanced researchers’ capacity to draw meaningful conclusions from complex datasets. For instance, the advent of big data analytics allows researchers to integrate information from multiple sources—such as genomic data, clinical records, and patient-reported outcomes—into a cohesive framework for analysis.
This holistic approach enables a more nuanced understanding of disease mechanisms and treatment effects. Moreover, advancements in bioinformatics have transformed how researchers interpret biological data. With the increasing availability of genomic sequencing technologies, researchers can now analyze genetic variations associated with diseases at an unprecedented scale.
This has led to the identification of novel biomarkers that can predict treatment responses or disease progression. For example, in oncology, genomic profiling of tumors has become a standard practice, allowing for targeted therapies that are tailored to the specific genetic makeup of a patient’s cancer. As data analysis techniques continue to advance, they will empower researchers to uncover insights that can lead to breakthroughs in treatment strategies.
Ethical Considerations in Clinical Research
Ethical considerations are paramount in clinical research, as they ensure the protection of human subjects and uphold the integrity of scientific inquiry. The principles outlined in the Declaration of Helsinki and the Belmont Report serve as foundational guidelines for ethical conduct in research involving human participants. Informed consent is a critical component of this ethical framework; participants must be fully aware of the risks and benefits associated with their involvement in a study before agreeing to participate.
This process not only respects individual autonomy but also fosters trust between researchers and participants. Additionally, ethical dilemmas often arise in the context of vulnerable populations who may be at greater risk for exploitation or harm. Special considerations must be taken when conducting research involving children, pregnant women, or individuals with cognitive impairments.
Researchers are tasked with ensuring that these populations are not only protected but also that their voices are included in the research process. This may involve adapting consent processes or employing surrogate decision-makers when necessary. As clinical research continues to evolve, ongoing discussions about ethics will be essential to navigate the complexities of modern studies while safeguarding participant welfare.
Collaborations and Partnerships in Clinical Research
| Metric | Value | Description |
|---|---|---|
| Number of Clinical Trials | 150+ | Total active clinical trials conducted by Frontier Clinical Research |
| Therapeutic Areas | 10+ | Range of therapeutic areas covered including oncology, cardiology, neurology, etc. |
| Patient Enrollment Rate | 95% | Percentage of target patient enrollment achieved on time |
| Study Start-Up Time | 30 days | Average time from protocol approval to first patient enrolled |
| Data Accuracy Rate | 99.5% | Percentage of clinical data verified as accurate and compliant |
| Regulatory Approval Success | 90% | Rate of successful regulatory submissions and approvals |
| Global Reach | 20+ countries | Number of countries where clinical trials are conducted |
| Average Study Duration | 18 months | Typical length of a clinical trial from initiation to completion |
Collaboration is a cornerstone of successful clinical research, as it brings together diverse expertise and resources to address complex health challenges. Partnerships between academic institutions, pharmaceutical companies, healthcare providers, and regulatory agencies can enhance the efficiency and effectiveness of research initiatives. For example, public-private partnerships have emerged as a powerful model for accelerating drug development processes.
By pooling resources and knowledge from various sectors, these collaborations can streamline clinical trial designs and facilitate faster access to innovative therapies. Moreover, international collaborations are becoming increasingly important in addressing global health issues. Diseases do not respect borders; therefore, multinational studies can provide valuable insights into disease prevalence and treatment efficacy across different populations.
The COVID-19 pandemic highlighted the necessity for global cooperation in clinical research, as researchers from around the world collaborated to develop vaccines at an unprecedented pace. Such partnerships not only enhance scientific rigor but also promote knowledge sharing and capacity building among researchers in low- and middle-income countries.
Patient-Centered Approaches in Clinical Research
The shift towards patient-centered approaches in clinical research reflects a growing recognition of the importance of incorporating patient perspectives into study design and implementation. Engaging patients as active partners in research can lead to more relevant questions being asked and more meaningful outcomes being measured. For instance, patient-reported outcomes (PROs) are increasingly being integrated into clinical trials to capture patients’ experiences with treatments beyond traditional clinical endpoints.
This approach acknowledges that patients’ perceptions of their health and quality of life are critical components of treatment success. Furthermore, involving patients in the design phase of studies can help ensure that research addresses their needs and preferences. Patient advisory boards or focus groups can provide valuable insights into what aspects of a study are most important to participants.
This collaborative approach not only enhances recruitment efforts but also fosters a sense of ownership among patients regarding the research process. As patient-centered methodologies gain traction, they have the potential to transform clinical research into a more inclusive and responsive endeavor.
Regulatory Updates and Challenges in Clinical Research
The regulatory landscape governing clinical research is continually evolving in response to advancements in science and technology as well as societal expectations regarding patient safety and ethical conduct. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) play crucial roles in overseeing clinical trials and ensuring that new therapies meet rigorous safety and efficacy standards before they reach the market.
Recent updates have focused on streamlining approval processes for innovative therapies while maintaining robust oversight. However, navigating regulatory requirements can pose significant challenges for researchers. The complexity of regulations can vary widely across different jurisdictions, complicating multinational studies.
Additionally, as new technologies emerge—such as gene editing or digital therapeutics—regulatory frameworks must adapt to address unique safety concerns associated with these innovations. Researchers must remain vigilant about compliance with evolving regulations while also advocating for policies that facilitate timely access to new treatments for patients.
Future Trends in Clinical Research
Looking ahead, several trends are poised to shape the future landscape of clinical research significantly. One notable trend is the increasing emphasis on real-world evidence (RWE) derived from observational studies and post-marketing surveillance. As healthcare systems seek to understand how treatments perform outside controlled trial settings, RWE will play an essential role in informing clinical guidelines and reimbursement decisions.
Additionally, personalized medicine is expected to gain further traction as advancements in genomics continue to unveil insights into individual variability in drug responses. Tailoring treatments based on genetic profiles will not only enhance efficacy but also minimize adverse effects for patients. The integration of artificial intelligence into this paradigm will facilitate more precise predictions regarding treatment outcomes based on genetic data.
Finally, as patient engagement becomes more central to clinical research design, we may see an increase in decentralized trials that leverage technology to allow participants to engage from their homes. This shift could enhance recruitment diversity by making participation more accessible to individuals who may face barriers to traditional trial enrollment. In summary, the future of clinical research is likely to be characterized by greater collaboration across sectors, innovative use of technology for data collection and analysis, heightened ethical scrutiny, and an unwavering commitment to placing patients at the heart of research endeavors.
As these trends unfold, they will undoubtedly contribute to a more effective and responsive healthcare landscape that prioritizes patient needs while advancing scientific knowledge.




