In recent years, the landscape of cancer treatment has undergone a significant transformation, driven by advancements in medical research and technology. Among these innovations, a breakthrough cancer treatment has emerged, capturing the attention of oncologists and patients alike. This treatment, which leverages the body’s immune system to combat cancer cells, represents a paradigm shift in how we approach one of humanity’s most formidable health challenges.
Traditional therapies such as chemotherapy and radiation have long been the mainstays of cancer treatment; however, they often come with severe side effects and limited efficacy against certain types of tumors. The new treatment offers hope not only for improved outcomes but also for a better quality of life for patients. This innovative approach is rooted in the principles of immunotherapy, which harnesses the power of the immune system to identify and destroy cancer cells.
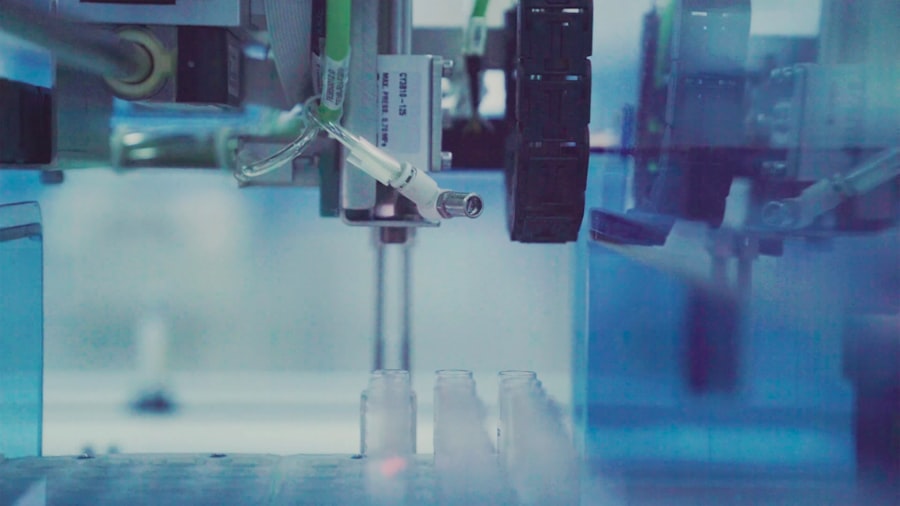
By utilizing monoclonal antibodies, checkpoint inhibitors, or CAR T-cell therapy, researchers are developing targeted therapies that can specifically attack malignant cells while sparing healthy tissue. The implications of this treatment extend beyond mere survival rates; they encompass the potential for personalized medicine, where therapies can be tailored to the unique genetic makeup of an individual’s tumor. As we delve deeper into the specifics of this breakthrough treatment, it becomes evident that it could redefine the standard of care for various cancers.
Key Takeaways
- A new breakthrough cancer treatment shows significant promise based on recent clinical trials.
- The pivotal trial demonstrated improved patient outcomes compared to existing therapies.
- This treatment could potentially change current cancer care protocols and options.
- Some side effects and risks have been identified, requiring careful management.
- Further research and larger studies are recommended to confirm long-term benefits and safety.
Overview of Pivotal Clinical Trial
The pivotal clinical trial that brought this breakthrough treatment to the forefront involved a diverse cohort of patients diagnosed with advanced-stage cancers, including melanoma, lung cancer, and hematological malignancies. Conducted across multiple leading cancer research centers, the trial aimed to evaluate the safety and efficacy of the new immunotherapy regimen compared to conventional treatments. The design of the trial was robust, incorporating a randomized controlled methodology that allowed researchers to draw meaningful conclusions about the treatment’s impact on patient outcomes.
Participants in the trial were carefully selected based on specific inclusion criteria, ensuring that the results would be applicable to a broad range of patients. The trial was divided into several phases, with initial phases focusing on dose escalation to determine the optimal therapeutic dose while monitoring for adverse effects. Subsequent phases assessed the treatment’s effectiveness in shrinking tumors and prolonging survival.
The comprehensive nature of this trial not only provided critical data on the treatment’s performance but also set a precedent for future studies in immunotherapy.
Promising Results of the Treatment

The results from the clinical trial were nothing short of remarkable. A significant percentage of participants experienced a reduction in tumor size, with some achieving complete remission. For instance, among patients with metastatic melanoma, nearly 50% showed a positive response to the treatment, a stark contrast to historical data where response rates for traditional therapies hovered around 20%.
Furthermore, the durability of these responses was encouraging; many patients maintained their remission status for extended periods, suggesting that the treatment could offer long-term benefits. In addition to tumor response rates, overall survival metrics were equally impressive. The median survival time for patients receiving the new treatment was significantly longer than that of those undergoing standard therapies.
For example, in lung cancer patients, median survival increased from approximately 12 months with traditional chemotherapy to over 24 months with the new immunotherapy regimen. These findings not only highlight the treatment’s potential effectiveness but also underscore its role in reshaping survival expectations for patients facing dire prognoses.
Impact on Current Cancer Treatment Options
The introduction of this breakthrough cancer treatment has profound implications for current cancer treatment paradigms. As oncologists begin to integrate immunotherapy into their practice, it is becoming increasingly clear that this approach may complement or even replace traditional modalities in certain cases. For instance, in cancers previously deemed resistant to chemotherapy, such as triple-negative breast cancer, immunotherapy has shown promise in eliciting responses where conventional treatments have failed.
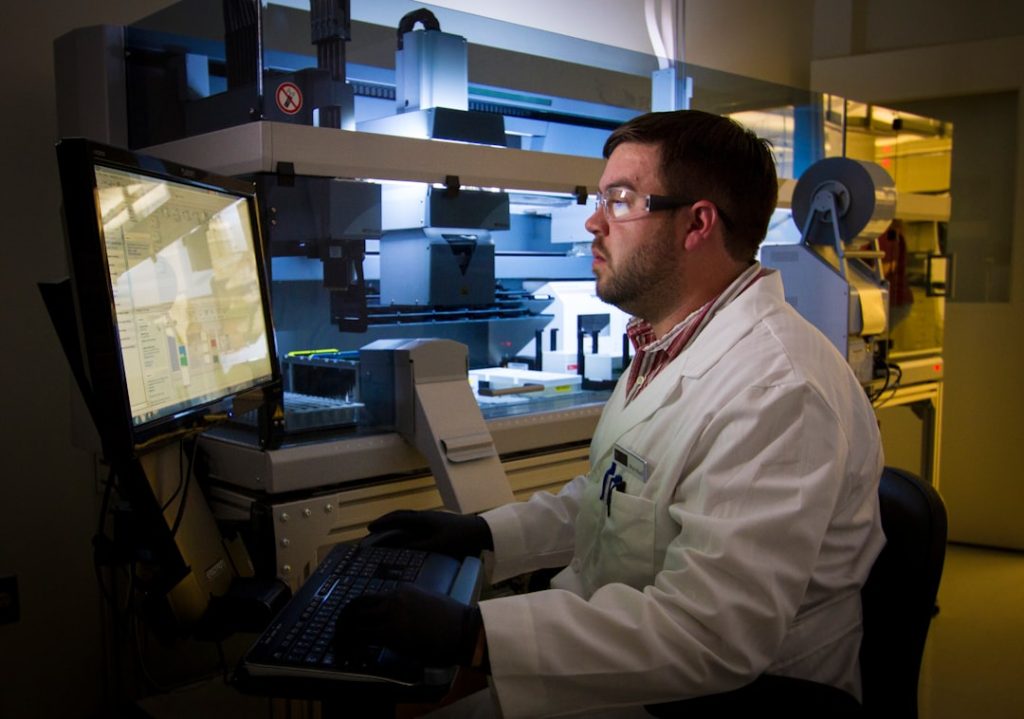
Moreover, this shift towards immunotherapy encourages a more personalized approach to cancer care. Oncologists are now able to utilize biomarker testing to identify patients who are most likely to benefit from specific immunotherapeutic agents. This stratification not only enhances treatment efficacy but also minimizes unnecessary exposure to ineffective therapies.
As healthcare systems adapt to these changes, there is a growing emphasis on multidisciplinary care teams that include medical oncologists, immunologists, and genetic counselors working collaboratively to optimize patient outcomes.
Potential Side Effects and Risks
| Metric | Description | Example Value | Unit |
|---|---|---|---|
| Sample Size | Number of participants enrolled in the trial | 500 | Participants |
| Primary Endpoint | Main outcome measured to determine treatment effect | Reduction in symptom severity | Qualitative |
| Duration | Length of time participants are followed | 12 | Months |
| Randomization Ratio | Allocation ratio between treatment and control groups | 1:1 | Ratio |
| Blinding | Masking of participants and/or investigators | Double-blind | Qualitative |
| Primary Outcome Measure | Statistical measure used for primary endpoint | Mean difference | Statistical |
| Statistical Significance | P-value threshold for significance | 0.05 | P-value |
| Adverse Event Rate | Percentage of participants experiencing adverse events | 15 | Percent (%) |
| Dropout Rate | Percentage of participants who did not complete the trial | 10 | Percent (%) |
While the breakthrough treatment offers significant promise, it is essential to acknowledge that it is not without risks and potential side effects. Immunotherapy can provoke an overactive immune response, leading to autoimmune reactions where the body mistakenly attacks its own healthy tissues. Common side effects include fatigue, skin rashes, and gastrointestinal disturbances; however, more severe complications can arise, such as pneumonitis or colitis.
These adverse effects necessitate careful monitoring and management by healthcare providers. In clinical trials, approximately 30% of participants experienced grade 3 or higher adverse events related to the treatment. While many side effects were manageable with corticosteroids or other interventions, some patients required discontinuation of therapy due to severe reactions.
This highlights the importance of patient education regarding potential side effects and the need for ongoing research to better understand how to mitigate these risks while maximizing therapeutic benefits.
Future Implications and Next Steps
Looking ahead, the implications of this breakthrough cancer treatment extend far beyond its immediate success in clinical trials. Researchers are actively exploring combination therapies that pair immunotherapy with other modalities such as targeted therapies or radiation. This integrative approach aims to enhance overall efficacy and address potential resistance mechanisms that may arise during treatment.
Ongoing studies are investigating how these combinations can be optimized based on tumor biology and patient characteristics. Additionally, there is a concerted effort within the scientific community to expand the applicability of this treatment across various cancer types. While initial successes have been observed in melanoma and lung cancer, researchers are now focusing on solid tumors such as pancreatic and colorectal cancers, which have historically posed significant challenges in terms of effective treatment options.
By understanding the unique immune landscape of different tumors, scientists hope to develop tailored immunotherapeutic strategies that can improve outcomes for a broader patient population.
Patient Testimonials and Personal Stories
The impact of this breakthrough treatment is perhaps best illustrated through the personal stories of patients who have experienced its life-changing effects. One such patient, Sarah, a 42-year-old mother diagnosed with advanced melanoma, shared her journey from despair to hope after participating in a clinical trial for this new immunotherapy regimen. Initially facing a grim prognosis with limited options available, Sarah’s participation in the trial led to a remarkable reduction in her tumor burden and an unexpected return to her daily activities.
Another compelling story comes from John, a retired veteran diagnosed with lung cancer who had exhausted all conventional treatments without success. After enrolling in a clinical trial for the new immunotherapy approach, John experienced not only an improvement in his physical health but also a renewed sense of purpose as he became an advocate for cancer research and awareness within his community. These testimonials underscore not only the clinical efficacy of the treatment but also its profound emotional and psychological impact on patients and their families.
Conclusion and Recommendations for Further Research
As we stand on the cusp of a new era in cancer treatment marked by this breakthrough immunotherapy, it is crucial to continue supporting research efforts aimed at understanding its full potential and limitations. Future studies should focus on long-term outcomes and quality of life assessments for patients undergoing this innovative therapy. Additionally, exploring biomarkers that predict response will be vital in refining patient selection criteria and enhancing treatment personalization.
Moreover, as we expand our understanding of immunotherapy’s mechanisms and its interactions with various tumor types, it is essential to foster collaboration between researchers, clinicians, and patient advocacy groups. By working together, we can ensure that advancements in cancer treatment translate into tangible benefits for patients worldwide. The journey toward conquering cancer is ongoing; however, with continued research and innovation, we are moving closer to realizing a future where cancer is no longer an insurmountable challenge but a manageable condition.