Phase 3 clinical trials are essential in drug development, bridging laboratory research to market approval. These trials evaluate a treatment’s efficacy and safety in large populations of hundreds to thousands of participants. Their primary purpose is comparing the new intervention against existing treatments or placebos, generating comprehensive data for regulatory evaluation.
As typically the final step before regulatory submission, Phase 3 trials are crucial in advancing treatments from concept to clinical application. These trials employ sophisticated designs, primarily randomized controlled methodologies, to eliminate bias and ensure scientific validity. Participants are selected through specific criteria to create uniform study populations that yield clear results about drug performance.
Many Phase 3 trials operate across multiple centers to increase participant diversity and make findings more broadly applicable. The resulting data influences not only regulatory decisions but also shapes clinical guidelines and treatment protocols, significantly impacting healthcare delivery.
Key Takeaways
- Phase 3 clinical trials provide critical data on treatment efficacy and safety in large patient populations.
- Promising results indicate significant improvements in patient outcomes compared to existing therapies.
- Safety profiles reveal manageable side effects, supporting the treatment’s overall benefit-risk balance.
- Successful Phase 3 outcomes are pivotal for regulatory approval and subsequent market access.
- Future research will explore broader applications and long-term impacts on healthcare practices.
Overview of Promising Results
Recent Phase 3 clinical trials have yielded promising results across various therapeutic areas, showcasing advancements in treatment options for conditions that have long posed challenges to healthcare providers. For instance, in oncology, several Phase 3 trials have demonstrated significant improvements in overall survival rates for patients with advanced cancers. A notable example is the use of immunotherapy agents, such as checkpoint inhibitors, which have shown remarkable efficacy in treating melanoma and lung cancer.
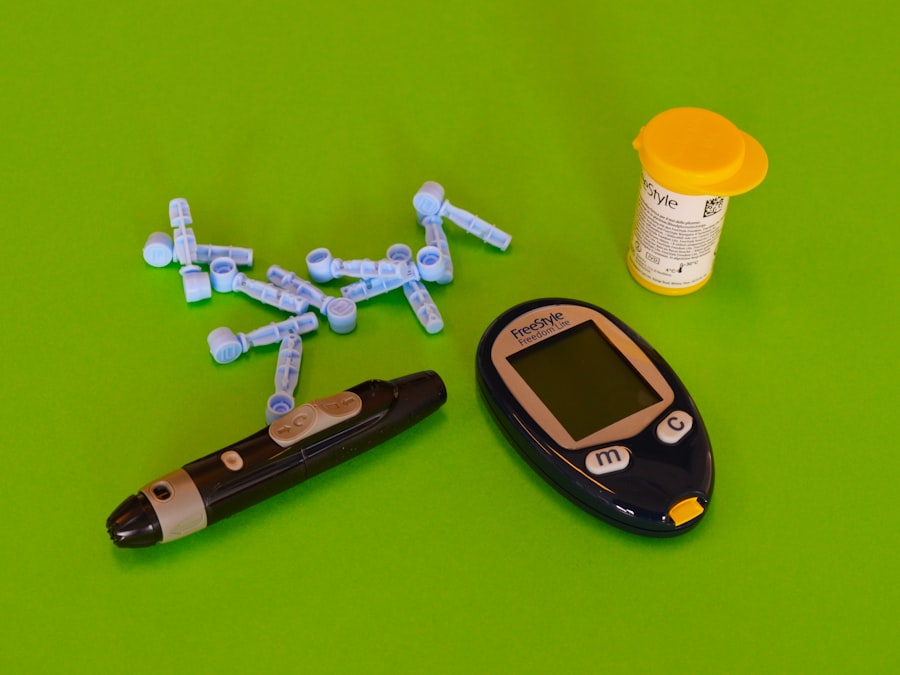
In these studies, patients receiving the new therapies exhibited not only longer survival times but also improved quality of life compared to those on standard treatments. In addition to oncology, Phase 3 trials in chronic diseases such as diabetes and cardiovascular conditions have also produced encouraging outcomes. For example, a recent trial evaluating a novel GLP-1 receptor agonist for type 2 diabetes management reported substantial reductions in HbA1c levels and weight loss among participants.
These results suggest that the new medication could offer a more effective alternative to existing therapies, potentially transforming the standard of care for millions of patients. Such promising findings underscore the importance of Phase 3 trials in validating new treatments that can significantly impact patient health and well-being.
Impact on Patient Outcomes
The implications of successful Phase 3 clinical trials extend far beyond statistical significance; they have profound effects on patient outcomes and overall public health. When a new treatment demonstrates superior efficacy or safety compared to existing options, it can lead to improved management of chronic conditions, reduced morbidity, and enhanced quality of life for patients. For instance, the introduction of novel anticoagulants following successful Phase 3 trials has revolutionized the management of atrial fibrillation, significantly lowering the risk of stroke while minimizing bleeding complications compared to traditional therapies like warfarin.
Moreover, the impact of these trials is not limited to individual patients; they can also influence healthcare systems and policies. As new treatments become available and gain approval based on Phase 3 results, healthcare providers may adopt updated clinical guidelines that reflect the latest evidence-based practices. This shift can lead to widespread changes in treatment protocols, ultimately improving patient outcomes on a population level.
For example, the approval of new biologics for rheumatoid arthritis has prompted a reevaluation of treatment strategies, allowing for earlier intervention and better disease control among affected individuals.
Potential Side Effects and Safety Profile
While Phase 3 clinical trials are instrumental in establishing the efficacy of new treatments, they also play a crucial role in assessing safety profiles and potential side effects. The larger participant pool allows researchers to identify adverse events that may not have been apparent in earlier phases of testing. This comprehensive evaluation is essential for understanding the risk-benefit ratio of a new drug.
For instance, during Phase 3 trials for certain antidepressants, researchers may uncover side effects such as increased suicidal ideation in specific populations, prompting further investigation and careful consideration before approval. The safety monitoring process during Phase 3 trials is rigorous and often involves independent data monitoring committees that review adverse events as they occur. This oversight ensures that any emerging safety concerns are addressed promptly, allowing for adjustments in trial protocols or even halting the trial if necessary.
Furthermore, once a drug is approved and enters the market, ongoing surveillance continues through post-marketing studies and registries to monitor long-term safety and effectiveness. This vigilance is crucial for maintaining public trust in new therapies and ensuring that any potential risks are communicated effectively to healthcare providers and patients alike.
Comparison with Previous Phases
| Clinical Trial Stage | Description | Primary Objective | Typical Duration | Number of Participants | Success Rate (%) |
|---|---|---|---|---|---|
| Preclinical | Laboratory and animal testing to assess safety and biological activity | Evaluate safety and biological effect | 1-2 years | Not applicable | Variable |
| Phase 1 | First trials in humans, focusing on safety and dosage | Assess safety, tolerability, and pharmacokinetics | Several months | 20-100 healthy volunteers | 70% |
| Phase 2 | Evaluate efficacy and side effects in patients with the condition | Assess efficacy and side effects | Several months to 2 years | 100-300 patients | 33% |
| Phase 3 | Large-scale testing to confirm effectiveness and monitor adverse reactions | Confirm efficacy and monitor adverse reactions | 1-4 years | 1,000-3,000 patients | 25-30% |
| Phase 4 | Post-marketing studies to gather additional information on risks and benefits | Monitor long-term effects and effectiveness | Varies (ongoing) | Thousands of patients | Not applicable |
Phase 3 clinical trials differ significantly from earlier phases in terms of scale, objectives, and complexity. In Phase 1 trials, the primary focus is on assessing safety and tolerability in a small group of healthy volunteers or patients with specific conditions. These studies typically involve fewer participants and are designed to establish dosage ranges and identify any immediate adverse effects.
Phase 2 trials build upon this foundation by evaluating efficacy in a larger cohort while continuing to monitor safety. However, these phases often lack the statistical power needed to draw definitive conclusions about treatment effectiveness across diverse populations. In contrast, Phase 3 trials are characterized by their larger sample sizes and more rigorous methodologies.
They aim not only to confirm efficacy but also to provide comprehensive data on safety across varied demographics. The randomized controlled design employed in Phase 3 studies allows for more reliable comparisons between treatment groups, reducing bias and enhancing the validity of results. This distinction is crucial because it ensures that findings can be generalized to broader patient populations, ultimately informing clinical practice and regulatory decisions.
Regulatory Implications and Approval Process
The outcomes of Phase 3 clinical trials carry significant regulatory implications that can determine whether a new treatment receives approval from agencies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA). Following the completion of these trials, sponsors submit a New Drug Application (NDA) or Biologics License Application (BLA) that includes comprehensive data on efficacy, safety, manufacturing processes, and proposed labeling.
Regulatory bodies meticulously review this information to assess whether the benefits of the new treatment outweigh its risks. The approval process can be lengthy and complex, often involving advisory committee meetings where external experts evaluate the trial data and provide recommendations. In some cases, regulatory agencies may request additional studies or post-marketing commitments to further assess long-term safety or specific subpopulations before granting approval.
The rigorous nature of this process underscores the importance of Phase 3 trials in ensuring that only safe and effective treatments reach patients. Moreover, successful navigation through this regulatory landscape can pave the way for expedited pathways or priority reviews for drugs addressing unmet medical needs.
Future Directions and Potential Applications
As medical science continues to evolve, the landscape of Phase 3 clinical trials is also changing, with innovative methodologies and technologies shaping future research directions. One notable trend is the increasing use of adaptive trial designs, which allow for modifications to be made during the trial based on interim results. This flexibility can enhance efficiency by enabling researchers to identify effective treatments more quickly while minimizing exposure to ineffective ones.
Such designs are particularly valuable in rapidly evolving fields like oncology, where treatment paradigms shift frequently based on emerging evidence. Additionally, advancements in personalized medicine are influencing how Phase 3 trials are conducted. The integration of biomarkers and genetic profiling into trial designs allows for more targeted approaches that can identify which patient populations are most likely to benefit from specific therapies.
This shift toward precision medicine not only enhances the likelihood of successful outcomes but also optimizes resource allocation within healthcare systems. As researchers continue to explore novel therapeutic avenues—such as gene therapies or regenerative medicine—the role of Phase 3 trials will remain pivotal in validating these innovative approaches before they become standard practice.
Conclusion and Implications for Healthcare
The significance of Phase 3 clinical trials extends far beyond their immediate outcomes; they play an essential role in shaping healthcare practices and policies worldwide. By providing robust evidence on the efficacy and safety of new treatments, these trials inform clinical guidelines that ultimately influence patient care decisions. As healthcare continues to evolve with advancements in technology and scientific understanding, the importance of rigorous clinical testing remains paramount.
Moreover, successful Phase 3 trials can lead to transformative changes in treatment landscapes across various medical fields. They not only offer hope for patients facing challenging health conditions but also drive innovation within pharmaceutical research and development. As we look toward the future, ongoing investment in clinical research will be crucial for addressing unmet medical needs and improving health outcomes on a global scale.
The journey from laboratory discovery to clinical application is complex, but it is through Phase 3 trials that we can ensure safe and effective therapies reach those who need them most.



