Clinical trials represent the primary methodology for evaluating the safety and efficacy of new medical treatments, pharmaceuticals, and devices in human subjects. These controlled studies follow standardized protocols and operate under stringent regulatory oversight to protect participant welfare while generating reliable scientific data. Results from clinical trials directly inform regulatory approval decisions and clinical practice guidelines that shape modern healthcare delivery.
Clinical trials serve multiple research objectives beyond drug testing, including investigation of disease pathophysiology, biomarker identification, and development of targeted therapeutic strategies. Each study addresses specific research hypotheses through controlled comparisons between experimental interventions and established treatments or placebos. The translation of laboratory findings to clinical applications requires systematic evaluation through multiple trial phases, with each stage designed to assess different aspects of treatment safety, dosing, and effectiveness before potential implementation in standard medical practice.
Key Takeaways
- Clinical trials progress through phases I to III, focusing on safety, efficacy, and large-scale testing.
- Preclinical studies and Investigational New Drug applications are essential before human trials begin.
- Regulatory approval follows successful trials, with ongoing post-market surveillance to monitor safety.
- Patients must provide informed consent and have access to information when participating in trials.
- Understanding each trial phase helps patients navigate the clinical trial process effectively.
Preclinical Phase and Investigational New Drug Application
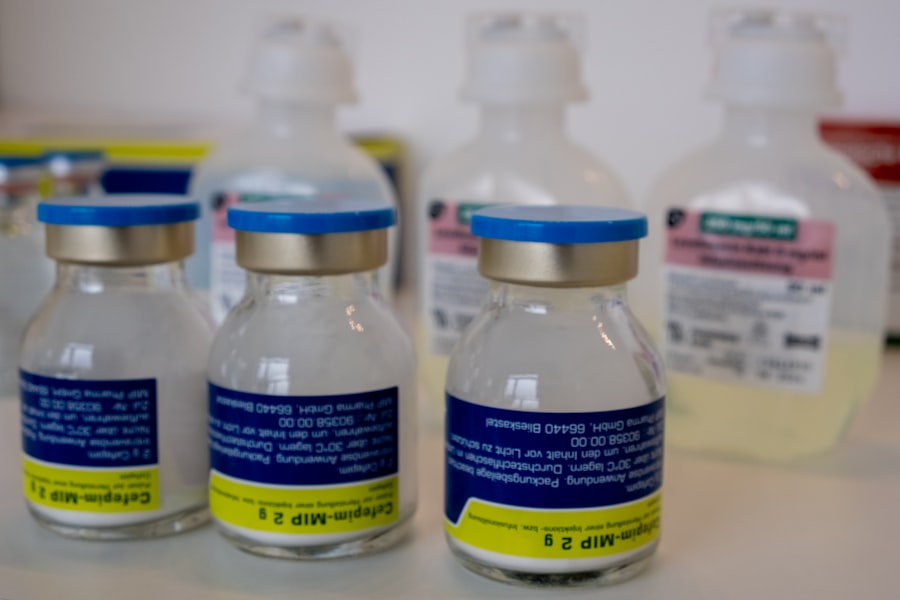
Before a new drug can be tested in humans, it undergoes a preclinical phase that involves extensive laboratory research and animal studies. This phase is critical for assessing the pharmacological properties of a drug candidate, including its mechanism of action, pharmacokinetics, and potential toxicity. Researchers conduct experiments to determine how the drug behaves in biological systems, which helps identify safe dosage ranges and potential side effects.
The preclinical phase serves as a foundational step that informs the design of subsequent clinical trials. Once sufficient data is gathered from preclinical studies, researchers must submit an Investigational New Drug (IND) application to regulatory authorities, such as the U.S. Food and Drug Administration (FDA).
This application includes comprehensive information about the drug’s chemical composition, manufacturing processes, proposed clinical trial protocols, and results from preclinical studies. The IND application is a critical gatekeeping mechanism that ensures only those drugs with promising safety profiles and therapeutic potential proceed to human testing. Regulatory agencies review this application meticulously, assessing the risk-benefit ratio before granting approval for clinical trials to commence.
Phase I Clinical Trials: Safety and Dosage

Phase I clinical trials mark the first time a new drug is administered to humans, typically involving a small group of healthy volunteers or patients. The primary objective of this phase is to evaluate the safety profile of the drug, determine appropriate dosage levels, and identify any adverse effects. Researchers closely monitor participants for any signs of toxicity or unexpected reactions, gathering data on how the drug is metabolized and excreted by the body.
This phase is crucial for establishing a safe dosage range that can be used in subsequent trials. In addition to safety assessments, Phase I trials often employ dose-escalation strategies. This means that participants may receive increasing doses of the drug over time to identify the maximum tolerated dose (MTD).
By carefully observing how different individuals respond to varying doses, researchers can pinpoint the optimal amount that balances efficacy with minimal side effects. The findings from Phase I trials lay the groundwork for Phase II studies, where the focus shifts from safety to evaluating the drug’s effectiveness in treating specific conditions.
Phase II Clinical Trials: Efficacy and Side Effects
Phase II clinical trials build upon the safety data gathered in Phase I by focusing on the efficacy of the drug in a larger group of participants who have the condition the drug aims to treat. This phase typically involves hundreds of patients and aims to provide preliminary evidence of whether the drug has a beneficial effect on the targeted disease or condition. Researchers employ various endpoints to measure efficacy, such as improvement in symptoms, reduction in disease progression, or overall survival rates.
In addition to assessing efficacy, Phase II trials continue to monitor participants for side effects and adverse reactions. This dual focus allows researchers to gain a more comprehensive understanding of how the drug performs in real-world scenarios. For instance, if a new cancer therapy shows promise in shrinking tumors but also leads to significant side effects like nausea or fatigue, researchers must weigh these factors when considering further development.
The data collected during this phase is critical for determining whether the drug should advance to Phase III trials, where larger populations will be studied.
Phase III Clinical Trials: Large-Scale Testing
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety and dosage | 20-100 healthy volunteers | Several months | Safety, side effects, pharmacokinetics | 70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Effectiveness, optimal dose, short-term side effects | 33% |
| Phase 3 | Confirm effectiveness and monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Comparison with standard treatments, long-term safety | 25-30% |
| Phase 4 | Post-marketing surveillance | Various (thousands) | Ongoing | Long-term effects, rare side effects, real-world use | N/A |
Phase III clinical trials represent a pivotal stage in the drug development process, as they involve large-scale testing across diverse populations. These trials typically include thousands of participants and are designed to confirm the efficacy observed in Phase II while further assessing safety in a broader context. Randomized controlled trials are often employed during this phase, where participants are randomly assigned to receive either the new treatment or a standard therapy/placebo.
This design helps eliminate bias and provides robust data on how well the new drug performs compared to existing options. The outcomes of Phase III trials are critical for regulatory approval. If the results demonstrate that the new treatment is significantly more effective than current therapies or offers unique benefits with manageable side effects, it can pave the way for marketing authorization.
However, if the data reveals that the new drug does not provide sufficient advantages or poses unacceptable risks, it may be rejected at this stage. The comprehensive nature of Phase III trials ensures that any new treatment introduced into clinical practice has undergone rigorous evaluation and meets high standards for safety and efficacy.
Regulatory Approval and Post-Market Surveillance
Following successful completion of Phase III trials, pharmaceutical companies submit a New Drug Application (NDA) or Biologics License Application (BLA) to regulatory agencies for approval. This application includes all data collected throughout the clinical trial phases, along with proposed labeling information and manufacturing details. Regulatory bodies conduct thorough reviews of this documentation to ensure that the benefits of the new treatment outweigh any potential risks before granting approval for public use.
Even after a drug receives regulatory approval, its journey does not end there. Post-market surveillance is an essential component of ongoing safety monitoring once a drug is available on the market. This phase involves collecting real-world data on how the drug performs in diverse patient populations over time.
Adverse events may still occur after approval, necessitating continuous monitoring through systems like the FDA’s Adverse Event Reporting System (FAERS). This vigilance helps identify rare side effects or long-term consequences that may not have been evident during clinical trials, ensuring that patient safety remains a priority throughout a drug’s lifecycle.
Accessing Clinical Trials and Informed Consent
Accessing clinical trials can provide patients with opportunities to receive cutting-edge treatments that are not yet widely available. However, participation in these studies requires careful consideration and informed consent. Informed consent is a fundamental ethical requirement that ensures participants understand the nature of the trial, potential risks and benefits, and their rights as subjects.
Researchers must provide clear information about what participation entails, including any procedures involved, possible side effects, and the right to withdraw at any time without penalty. Patients interested in participating in clinical trials can find opportunities through various channels, including healthcare providers, clinical trial registries, and patient advocacy organizations. These resources help connect patients with ongoing studies that align with their medical conditions and treatment needs.
However, navigating this landscape can be complex; patients must weigh their options carefully and consider factors such as eligibility criteria, location of trials, and potential impacts on their current treatment plans.
Navigating the Phases of Clinical Trials: Patient Perspectives
From a patient perspective, navigating the phases of clinical trials can be both daunting and empowering. Many patients view participation as an opportunity to contribute to medical research while potentially gaining access to innovative therapies that may improve their health outcomes. However, concerns about safety and uncertainty regarding treatment efficacy can create apprehension.
Patients often grapple with questions about whether they will receive a placebo or an active treatment and how participation might affect their quality of life. Moreover, personal motivations for joining clinical trials vary widely among patients. Some may be driven by a desire to help advance science for future generations or find hope when conventional treatments have failed them.
Others may seek additional support from healthcare teams who are often more engaged in monitoring their health during trial participation. Ultimately, understanding both the potential benefits and risks associated with clinical trials empowers patients to make informed decisions about their involvement in this critical aspect of medical research.



