Clinical trials represent the fundamental framework of contemporary medical research, functioning as the standard methodology for assessing the safety and effectiveness of novel treatments, pharmaceuticals, and medical devices. These studies are carefully structured investigations involving human subjects that are critical for converting laboratory findings into practical therapeutic solutions. Clinical trials fulfill both regulatory mandates and ethical responsibilities by ensuring new medical interventions demonstrate safety and efficacy prior to public distribution.
The development pathway from initial concept or laboratory discovery to commercial product typically spans multiple years to decades. Clinical trials provide value beyond treatment approval by expanding scientific understanding of diseases and therapeutic approaches. Through systematic data collection on how diverse patient populations respond to different interventions, researchers determine treatment effectiveness while identifying potential adverse effects and drug interactions.
This comprehensive data serves as the foundation for evidence-based clinical guidelines that inform healthcare provider decision-making. Clinical trials therefore constitute an essential component in the advancement of medical science and the enhancement of patient care outcomes.
Key Takeaways
- Clinical trials progress through phases I to III, each assessing safety, efficacy, and dosage.
- Preclinical research involves laboratory and animal studies to evaluate potential treatments before human trials.
- Regulatory approval requires comprehensive data from all trial phases to ensure treatment safety and effectiveness.
- Ethical considerations and challenges, such as informed consent and participant safety, are critical throughout trials.
- Future medical research focuses on innovative methods and technologies to improve trial efficiency and patient outcomes.
Preclinical Research and Development
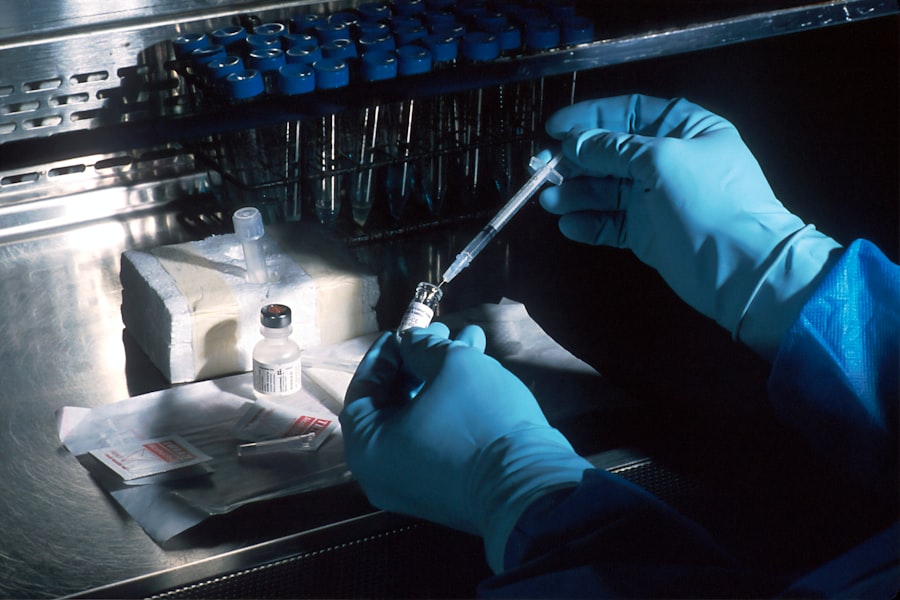
Before any clinical trial can commence, extensive preclinical research is conducted to assess the feasibility of a new treatment. This phase typically involves laboratory experiments and animal studies designed to gather preliminary efficacy, toxicity, and pharmacokinetic data. Researchers aim to understand how a potential drug interacts with biological systems, its mechanism of action, and its potential side effects.
For instance, if a new cancer drug is being developed, scientists may first test it on cancer cell lines in vitro before moving on to animal models that mimic human disease. Preclinical studies are critical for identifying promising candidates for further development. They help researchers determine the appropriate dosages and delivery methods, as well as establish safety profiles that inform the design of subsequent clinical trials.
Regulatory agencies, such as the U.S. Food and Drug Administration (FDA), require comprehensive preclinical data before granting permission to initiate human trials. This rigorous vetting process ensures that only those treatments with a reasonable expectation of safety and efficacy progress to the next stage of development.
Phase I Clinical Trials

Phase I clinical trials mark the first time a new treatment is tested in humans, typically involving a small group of healthy volunteers or patients with the target condition. The primary objective of Phase I trials is to evaluate the safety of the drug, determine a safe dosage range, and identify any side effects. These trials often employ a dose-escalation design, where participants receive increasing doses of the drug until adverse effects are observed or a maximum tolerated dose is established.
In addition to safety assessments, Phase I trials also provide valuable pharmacokinetic data, which describes how the drug is absorbed, distributed, metabolized, and excreted by the body. For example, researchers may use blood samples to measure drug concentrations over time, helping them understand how long the drug remains active in the system. This information is crucial for determining dosing regimens in later phases of clinical trials.
While Phase I trials typically involve a small number of participants—often fewer than 100—their findings lay the groundwork for subsequent phases by ensuring that only safe and tolerable treatments advance.
Phase II Clinical Trials
Once a treatment has demonstrated safety in Phase I trials, it progresses to Phase II trials, which focus on evaluating its efficacy and further assessing its safety in a larger group of participants. Phase II trials usually involve several hundred patients who have the condition that the treatment aims to address. The primary goal during this phase is to determine whether the drug has a beneficial effect on the disease or condition being treated.
Phase II trials are often designed as randomized controlled trials (RCTs), where participants are assigned to receive either the experimental treatment or a placebo. This design helps eliminate bias and allows researchers to draw more reliable conclusions about the treatment’s effectiveness. For instance, if a new antidepressant is being tested, researchers would compare outcomes between those receiving the medication and those receiving a placebo over a specified period.
Additionally, Phase II trials may explore different dosing regimens or combinations with other therapies to optimize treatment strategies.
Phase III Clinical Trials
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 0 | Microdosing to gather preliminary data on pharmacodynamics and pharmacokinetics | 10-15 | Several months | Safety and biological activity | Not applicable |
| Phase I | Assess safety, dosage range, and side effects | 20-100 healthy volunteers | Several months | Safety and dosage | Approximately 70% |
| Phase II | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Efficacy and side effects | Approximately 33% |
| Phase III | Confirm effectiveness, monitor side effects, compare to commonly used treatments | 1,000-3,000 patients | 1-4 years | Effectiveness and safety | Approximately 25-30% |
| Phase IV | Post-marketing studies to delineate additional information including the drug’s risks, benefits, and optimal use | Various (thousands) | Varies (years) | Long-term safety and effectiveness | Ongoing monitoring |
Phase III clinical trials represent a critical juncture in the drug development process, as they involve large-scale testing across diverse populations to confirm efficacy and monitor adverse reactions in a more comprehensive manner. These trials typically enroll thousands of participants and are designed to provide definitive evidence regarding the treatment’s effectiveness compared to standard care or placebo. The results from Phase III trials are pivotal for regulatory approval and can significantly influence clinical practice.
In these trials, researchers often employ multi-center designs that allow for greater generalizability of results across different demographics and geographic locations. For example, if a new vaccine is being tested, it may be administered in various settings—urban hospitals, rural clinics, and community health centers—to ensure that findings are applicable to a broad population. The data collected during Phase III trials not only informs regulatory decisions but also shapes clinical guidelines and recommendations for healthcare providers once the treatment is approved for public use.
Regulatory Approval and Post-Market Surveillance
Following successful completion of Phase III trials, pharmaceutical companies submit their findings to regulatory agencies such as the FDA or the European Medicines Agency (EMA) for review and approval. This submission includes comprehensive data from all phases of clinical trials, along with manufacturing information and proposed labeling for the drug. Regulatory bodies meticulously evaluate this information to ensure that the benefits of the new treatment outweigh any potential risks before granting marketing authorization.
Once a drug is approved, it does not enter the market without ongoing scrutiny. Post-market surveillance is an essential component of ensuring long-term safety and efficacy. This phase involves monitoring adverse events reported by healthcare providers and patients after the drug has been released into general use.
Regulatory agencies may require additional studies—known as Phase IV trials—to further assess long-term effects or specific populations that were underrepresented in earlier trials. For instance, if a newly approved medication shows unexpected side effects in certain demographics post-approval, regulatory agencies may issue warnings or require additional research to address these concerns.
Challenges and Ethical Considerations in Clinical Trials
Conducting clinical trials presents numerous challenges that researchers must navigate carefully. One significant challenge is recruitment; finding suitable participants who meet specific eligibility criteria can be difficult, particularly for rare diseases or conditions with strict inclusion/exclusion parameters. Additionally, maintaining participant retention throughout lengthy trial periods can be problematic due to factors such as side effects or logistical issues related to trial visits.
Ethical considerations also play a crucial role in clinical trial design and implementation. Researchers must ensure informed consent is obtained from all participants, meaning they fully understand the nature of the trial, potential risks, and their right to withdraw at any time without penalty. The ethical principle of beneficence requires that researchers prioritize participant welfare while balancing scientific advancement with patient safety.
Institutional Review Boards (IRBs) are tasked with reviewing trial protocols to ensure ethical standards are upheld throughout the research process.
Future Directions in Medical Research
The landscape of clinical trials is evolving rapidly due to advancements in technology and an increasing emphasis on personalized medicine. One promising direction is the integration of digital health technologies into clinical trial designs. Wearable devices can collect real-time data on patient health metrics, allowing for more dynamic monitoring of treatment effects outside traditional clinical settings.
This approach not only enhances data collection but also improves patient engagement by allowing them to participate more actively in their care. Moreover, there is a growing focus on adaptive trial designs that allow for modifications based on interim results without compromising scientific integrity. These designs enable researchers to make real-time adjustments to trial parameters—such as dosage or participant allocation—based on emerging data trends.
This flexibility can lead to more efficient trials that reduce time and costs while still providing robust evidence for regulatory approval. As we look toward the future of medical research, collaboration among stakeholders—including academia, industry, regulatory bodies, and patient advocacy groups—will be essential for addressing complex health challenges. By fostering partnerships that prioritize transparency and shared goals, we can enhance the efficiency of clinical trials while ensuring that patient safety remains at the forefront of all research endeavors.



