World Clinical Trials (WCT) constitute a fundamental component of medical research, designed to evaluate new treatments, pharmaceuticals, and medical devices across diverse global populations. These studies systematically assess the safety, efficacy, and therapeutic impact of medical interventions on human subjects. WCTs operate across multiple geographical locations and healthcare settings, including hospitals, clinical research centers, and community health facilities, enabling researchers to gather data on treatment performance under varied real-world conditions.
The international scope of these trials enables the recruitment of participants from different ethnic, genetic, and socioeconomic backgrounds, providing essential data on how various demographic groups respond to medical interventions. This diversity is crucial for establishing the generalizability of research findings and ensuring that new treatments are effective across different populations. WCTs serve multiple functions in the healthcare system beyond data generation.
They provide the evidence base for clinical practice guidelines and regulatory approval decisions for new therapies. The data generated from these trials directly informs healthcare policy development and clinical decision-making processes. Additionally, WCTs function as the critical link between preclinical laboratory research and clinical implementation, facilitating the translation of scientific discoveries into practical medical applications.
As medical science advances and healthcare needs evolve globally, WCTs remain essential for generating the evidence required to improve patient care and advance therapeutic options.
Key Takeaways
- WCT clinical trials play a crucial role in advancing medical research by testing new treatments and therapies.
- The process involves careful planning, patient recruitment, and strict adherence to ethical standards.
- Ensuring informed consent and protecting patient rights are fundamental ethical considerations in WCT trials.
- Challenges include recruitment difficulties, regulatory hurdles, and managing trial limitations.
- Future directions focus on improving trial design, increasing efficiency, and enhancing patient engagement.
Importance of WCT Clinical Trials in Advancing Medical Research
WCT clinical trials play an indispensable role in advancing medical research by generating high-quality evidence that informs clinical practice. The rigorous methodologies employed in these trials ensure that findings are reliable and can be generalized to broader populations. For instance, when a new drug is tested in a WCT, it undergoes a series of phases that meticulously evaluate its safety and efficacy.
This structured approach not only protects participants but also enhances the credibility of the results, which can lead to regulatory approvals and subsequent integration into standard treatment protocols. Moreover, WCTs contribute significantly to the understanding of disease mechanisms and treatment responses. By enrolling diverse patient populations, researchers can identify variations in treatment efficacy based on genetic, environmental, and lifestyle factors.
This information is crucial for developing personalized medicine approaches that tailor treatments to individual patient needs. For example, in oncology, WCTs have led to the identification of specific biomarkers that predict how patients will respond to certain therapies, thereby optimizing treatment strategies and minimizing unnecessary side effects.
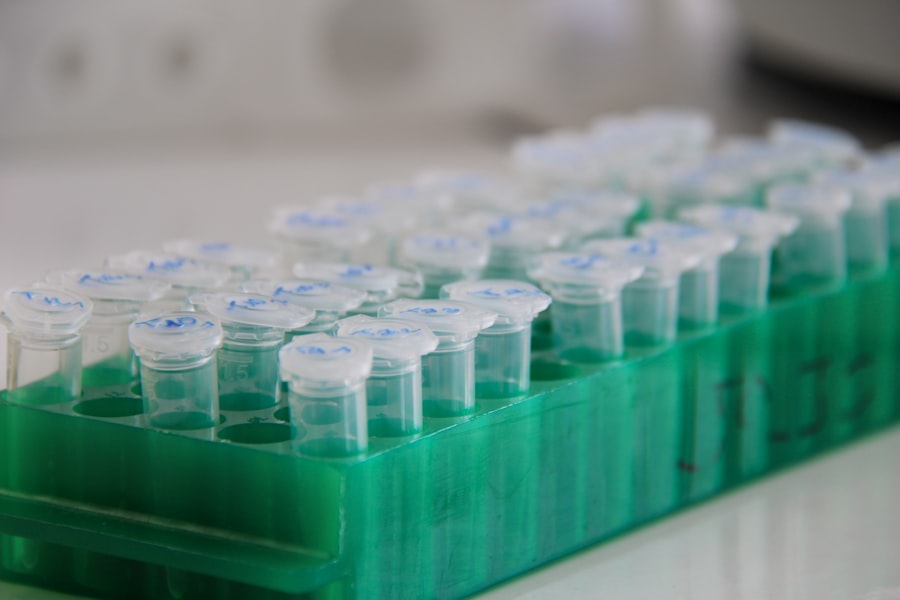
Process of Conducting WCT Clinical Trials
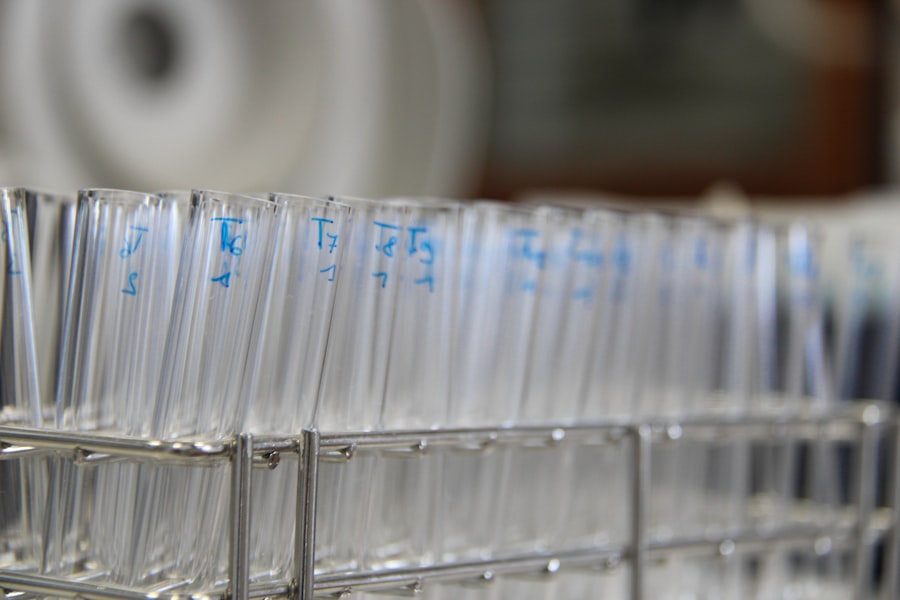
The process of conducting WCT clinical trials is multifaceted and involves several key stages, each designed to ensure the integrity and validity of the research. Initially, researchers must develop a clear study protocol that outlines the objectives, design, methodology, and statistical analysis plan. This protocol serves as a roadmap for the trial and must be approved by regulatory bodies and ethics committees before any participant recruitment can begin.
The design of the trial—whether it be randomized controlled trials (RCTs), observational studies, or adaptive trials—will significantly influence the quality of the data collected. Once the protocol is approved, the next step involves recruiting participants who meet specific inclusion and exclusion criteria. This phase is critical as it determines the representativeness of the study population.
Researchers often employ various strategies to reach potential participants, including outreach through healthcare providers, community organizations, and online platforms. After recruitment, participants undergo informed consent processes where they are educated about the trial’s purpose, procedures, potential risks, and benefits. This transparency is essential for fostering trust and ensuring that participants are fully aware of their involvement in the research.
Ethical Considerations in WCT Clinical Trials
Ethical considerations are paramount in WCT clinical trials, as they involve human subjects who may be vulnerable or at risk. The principle of “do no harm” is foundational in clinical research ethics, guiding researchers to prioritize participant safety throughout the trial process. Institutional Review Boards (IRBs) or Ethics Committees play a crucial role in reviewing study protocols to ensure that ethical standards are upheld.
They assess factors such as risk-benefit ratios, informed consent processes, and the adequacy of safety monitoring plans. In addition to participant safety, ethical considerations also encompass issues related to data integrity and transparency. Researchers are obligated to report findings honestly and without bias, regardless of whether results are favorable or unfavorable.
This commitment to transparency is vital for maintaining public trust in medical research and ensuring that findings can be reliably used to inform clinical practice. Furthermore, ethical guidelines emphasize the importance of equitable participant selection to avoid exploitation of vulnerable populations while ensuring that diverse groups are represented in research.
Patient Recruitment and Informed Consent in WCT Clinical Trials
| Trial ID | Title | Phase | Status | Condition | Enrollment | Start Date | Completion Date |
|---|---|---|---|---|---|---|---|
| NCT04567890 | WCT for Chronic Wound Healing | Phase 3 | Recruiting | Chronic Wounds | 150 | 2023-01-15 | 2025-06-30 |
| NCT03987654 | WCT in Diabetic Foot Ulcers | Phase 2 | Completed | Diabetic Foot Ulcers | 100 | 2020-05-01 | 2022-12-15 |
| NCT04123456 | WCT for Pressure Ulcers | Phase 1 | Active, not recruiting | Pressure Ulcers | 50 | 2022-03-10 | 2024-09-01 |
| NCT04789123 | WCT Combined with Standard Care | Phase 3 | Recruiting | Venous Leg Ulcers | 200 | 2023-07-01 | 2026-01-31 |
Patient recruitment is one of the most challenging aspects of conducting WCT clinical trials. Effective recruitment strategies are essential for ensuring that trials meet their enrollment targets within specified timelines. Researchers often face obstacles such as limited awareness among potential participants about ongoing trials or misconceptions about what participation entails.
To address these challenges, many research teams implement targeted outreach campaigns that utilize social media platforms, informational webinars, and collaborations with healthcare providers to raise awareness about available studies. Informed consent is another critical component of patient recruitment that requires careful attention. It is not merely a formality but a process that ensures participants understand their rights and the implications of their involvement in a trial.
Researchers must provide clear and comprehensive information about the study’s purpose, procedures, potential risks, benefits, and alternatives to participation. This process often involves discussions with potential participants to address any questions or concerns they may have. Ensuring that consent is truly informed empowers patients to make decisions that align with their values and preferences.
Challenges and Limitations in WCT Clinical Trials
Despite their importance, WCT clinical trials face numerous challenges and limitations that can impact their execution and outcomes. One significant challenge is the variability in regulatory requirements across different countries. Each nation has its own set of regulations governing clinical research, which can complicate multi-site trials and lead to delays in study initiation.
Researchers must navigate these regulatory landscapes carefully to ensure compliance while maintaining the integrity of their research. Another limitation is related to participant diversity and representation. While WCTs aim to include diverse populations, certain groups may be underrepresented due to various factors such as socioeconomic barriers or cultural hesitance towards clinical research participation.
This lack of diversity can limit the generalizability of trial findings and may result in treatments that are less effective for certain populations. Addressing these disparities requires concerted efforts from researchers to engage with communities and build trust through transparent communication about the benefits of participation.
Future Directions for WCT Clinical Trials
The future of WCT clinical trials is poised for transformation as advancements in technology and data science continue to reshape the landscape of medical research. One promising direction is the integration of digital health technologies into trial designs. Wearable devices and mobile health applications can facilitate real-time data collection on patient outcomes and adherence to treatment protocols.
This shift towards remote monitoring not only enhances data accuracy but also improves participant engagement by allowing them to participate from the comfort of their homes. Additionally, there is a growing emphasis on adaptive trial designs that allow for modifications based on interim results. These designs enable researchers to make data-driven decisions during the trial process, such as adjusting sample sizes or treatment regimens based on early findings.
This flexibility can lead to more efficient trials that yield meaningful results more quickly than traditional fixed designs. As regulatory agencies become more receptive to innovative trial methodologies, we can expect an increase in adaptive designs that enhance the responsiveness of clinical research.
Impact of WCT Clinical Trials on Medical Research
The impact of WCT clinical trials on medical research cannot be overstated; they serve as a cornerstone for evidence-based medicine by providing critical insights into new therapies and interventions. Through rigorous methodologies and ethical considerations, these trials contribute significantly to our understanding of health and disease while ensuring participant safety and informed decision-making. As we look ahead, embracing technological advancements and innovative trial designs will be essential for overcoming existing challenges and enhancing the efficiency of clinical research.
In summary, WCT clinical trials are integral to advancing medical knowledge and improving patient care across diverse populations worldwide. Their ability to generate high-quality evidence not only informs clinical practice but also shapes healthcare policies that ultimately benefit society as a whole. As we continue to navigate the complexities of modern medicine, the role of WCTs will remain vital in bridging the gap between scientific discovery and practical application in healthcare settings.



