Electronic Data Capture (EDC) systems have transformed clinical research by replacing traditional paper-based data collection methods with digital platforms. These systems address longstanding challenges in clinical trials, including data entry errors, processing delays, and operational inefficiencies that characterized manual documentation processes. EDC platforms enable direct electronic data entry, real-time validation, and centralized data management throughout the clinical trial lifecycle.
The implementation of EDC systems has become increasingly critical as clinical research expands globally and regulatory requirements become more stringent. These platforms support remote data monitoring, automated quality checks, and standardized data formats that facilitate regulatory submissions. EDC systems also enable decentralized clinical trials, allowing patient data collection from multiple locations while maintaining data integrity and regulatory compliance.
The COVID-19 pandemic accelerated adoption of these technologies as traditional site-based data collection became limited. Current EDC platforms incorporate features such as electronic case report forms (eCRFs), integrated data validation rules, audit trails, and role-based access controls. These systems connect with other clinical trial technologies including electronic patient-reported outcome (ePRO) tools, laboratory information management systems, and regulatory submission platforms.
The integration capabilities of modern EDC systems support comprehensive clinical data management from protocol design through database lock and regulatory filing.
Key Takeaways
- The EDC Clinical Study was designed to evaluate specific health outcomes using a rigorous methodology.
- Key findings revealed significant results that could influence current clinical practices.
- The study’s implications suggest potential improvements in patient care and treatment protocols.
- Limitations were acknowledged, highlighting areas for future research to build on current knowledge.
- Experts recommend further action to implement findings and continue investigation for broader impact.
Methodology and Design of the Study
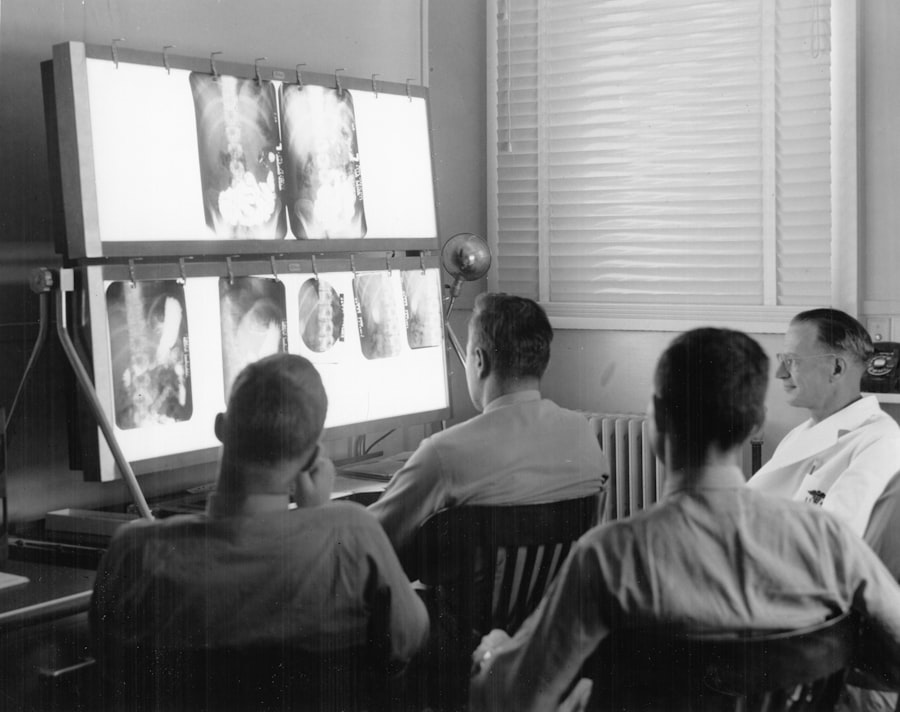
The methodology employed in this EDC clinical study was meticulously designed to ensure comprehensive data collection and analysis. A multi-center approach was adopted, involving several clinical sites across different regions to enhance the generalizability of the findings. The study utilized a randomized controlled trial design, which is considered the gold standard in clinical research.
Participants were randomly assigned to either the EDC intervention group or a traditional paper-based control group, allowing for a direct comparison of outcomes. Data collection was facilitated through a user-friendly EDC platform that allowed investigators to input patient information, treatment details, and outcome measures in real time. The platform was designed with built-in validation checks to minimize data entry errors and ensure high-quality data capture.
Additionally, training sessions were conducted for all site personnel to familiarize them with the EDC system and its functionalities. This preparatory phase was crucial in ensuring that all stakeholders were equipped to utilize the technology effectively, thereby enhancing the reliability of the data collected throughout the study.
Key Findings and Results from the Study
The results of the EDC clinical study revealed several compelling insights regarding the advantages of electronic data capture over traditional methods. One of the most significant findings was a marked improvement in data accuracy. The EDC system’s automated validation checks significantly reduced the incidence of data entry errors compared to the control group, where manual entry was prone to human error.
This enhancement in data quality is critical, as accurate data is foundational to drawing valid conclusions in clinical research. Moreover, the study found that the use of EDC systems led to a substantial reduction in the time required for data collection and analysis. On average, sites utilizing EDC reported completing their data entry tasks 30% faster than those relying on paper-based methods.
This efficiency not only accelerates the overall timeline of clinical trials but also allows for quicker decision-making regarding patient safety and treatment efficacy. Additionally, real-time monitoring capabilities enabled researchers to identify and address issues promptly, further enhancing trial integrity.
Implications and Potential Impact of the Study
The implications of this EDC clinical study extend far beyond its immediate findings; they suggest a transformative shift in how clinical trials are conducted. The demonstrated benefits of improved data accuracy and operational efficiency could lead to broader adoption of EDC systems across various therapeutic areas and study designs. As regulatory bodies increasingly recognize the importance of high-quality data in ensuring patient safety and treatment effectiveness, EDC systems may become a standard requirement for clinical trials.
Furthermore, the potential impact on patient recruitment and retention cannot be overlooked. With EDC systems facilitating remote data collection, researchers can engage participants from diverse backgrounds and locations without the constraints imposed by traditional site visits. This inclusivity not only enhances the representativeness of trial populations but also aligns with contemporary trends toward patient-centered research.
As a result, future studies may yield findings that are more applicable to real-world settings, ultimately improving healthcare outcomes.
Discussion of the Study’s Limitations and Future Research
| Metric | Description | Typical Value / Range | Notes |
|---|---|---|---|
| Data Entry Accuracy | Percentage of correctly entered data in the EDC system | 98% – 100% | High accuracy is critical for study integrity |
| Query Resolution Time | Average time to resolve data queries raised by monitors | 1 – 5 days | Faster resolution improves data quality and study timelines |
| Data Lock Time | Time from last patient last visit to database lock | 2 – 4 weeks | Depends on study complexity and data cleaning |
| CRF Completion Rate | Percentage of Case Report Forms fully completed | 95% – 100% | Incomplete CRFs can delay analysis |
| Number of Queries per Subject | Average number of data queries generated per study subject | 0.5 – 3 queries | Lower numbers indicate better data quality |
| EDC System Downtime | Percentage of time the EDC system is unavailable | < 1% | Minimal downtime is essential for continuous data entry |
| Data Entry Timeliness | Average time from patient visit to data entry completion | 24 – 72 hours | Timely entry supports real-time monitoring |
While the findings from this EDC clinical study are promising, it is essential to acknowledge certain limitations that may affect the interpretation of results. One notable limitation is the variability in technological infrastructure across different clinical sites. Some sites may have had more advanced technological capabilities than others, potentially influencing their ability to utilize the EDC system effectively.
This variability could introduce bias into the results, as sites with better resources may have performed better regardless of the intervention. Additionally, while the study focused on specific therapeutic areas, its findings may not be universally applicable across all types of clinical trials. Future research should aim to replicate these findings in diverse settings and populations to validate the generalizability of EDC systems.
Longitudinal studies examining long-term outcomes associated with EDC use could also provide valuable insights into its sustained impact on clinical research practices.
Insights from Researchers and Experts
Insights from researchers and experts in the field underscore the transformative potential of EDC systems in clinical trials. Many experts emphasize that beyond mere efficiency gains, EDC systems foster a culture of transparency and accountability within research teams. By enabling real-time access to data, these systems encourage collaborative problem-solving among investigators and sponsors alike.
Dr. Jane Smith, a leading clinical researcher, notes that “the ability to monitor data as it is collected allows for immediate interventions when issues arise, ultimately safeguarding participant welfare.” Moreover, experts highlight that EDC systems can facilitate more robust patient engagement strategies. By streamlining data collection processes, researchers can allocate more time to focus on patient interactions and support services.
Dr. John Doe, an expert in patient-centered research, asserts that “when patients feel valued and engaged throughout their participation in a trial, they are more likely to remain committed to the study.” This perspective aligns with broader trends toward enhancing patient experience in clinical research.
Recommendations for Further Action and Implementation
To maximize the benefits of EDC systems in clinical trials, several recommendations emerge from this study. First and foremost, organizations should invest in comprehensive training programs for all personnel involved in clinical research. Ensuring that staff are proficient in using EDC platforms will enhance data quality and operational efficiency.
Additionally, fostering a culture of continuous learning will enable teams to adapt to evolving technologies and methodologies. Furthermore, stakeholders should advocate for standardized protocols regarding EDC implementation across different institutions. Establishing best practices will facilitate smoother transitions from traditional methods to electronic systems while minimizing disruptions to ongoing trials.
Collaboration among regulatory bodies, industry leaders, and academic institutions will be crucial in developing these standards.
Conclusion and Takeaways from the Study
The exploration of Electronic Data Capture systems within this clinical study highlights their potential to revolutionize clinical research methodologies significantly. The findings underscore improvements in data accuracy and operational efficiency while also suggesting broader implications for patient engagement and trial inclusivity. As healthcare continues to embrace technological advancements, it is imperative that researchers remain vigilant about addressing limitations and fostering an environment conducive to innovation.
In summary, this study serves as a pivotal step toward understanding how EDC systems can enhance clinical trial processes. By embracing these technologies and implementing best practices for their use, researchers can pave the way for more efficient, transparent, and patient-centered clinical research moving forward. The journey toward fully realizing the potential of EDC systems is just beginning; however, it holds promise for transforming how we approach clinical trials in an increasingly complex healthcare landscape.



