Small cell lung cancer (SCLC) is a highly aggressive form of lung cancer that accounts for approximately 10-15% of all lung cancer cases. Characterized by its rapid growth and early metastasis, SCLC is often diagnosed at an advanced stage, which significantly complicates treatment options and prognosis. The cancer originates in the neuroendocrine cells of the lungs, leading to the formation of small, oval-shaped cancer cells that proliferate quickly.
This type of lung cancer is closely associated with smoking, with the vast majority of patients having a history of tobacco use. The pathophysiology of SCLC involves complex genetic mutations and alterations, including the inactivation of tumor suppressor genes such as TP53 and RB1, which play critical roles in cell cycle regulation and apoptosis. The clinical presentation of SCLC can vary widely among patients, but common symptoms include persistent cough, chest pain, weight loss, and shortness of breath.
Due to its aggressive nature, SCLC often spreads to other parts of the body, including the liver, brain, and bones, at the time of diagnosis. Staging is crucial in determining the extent of the disease and guiding treatment decisions. SCLC is typically classified into two stages: limited stage (LS-SCLC), where the cancer is confined to one lung and nearby lymph nodes, and extensive stage (ES-SCLC), where the disease has spread beyond the initial site.
The prognosis for SCLC remains poor, with a five-year survival rate of only about 6%, underscoring the urgent need for effective treatment strategies and ongoing research.
Key Takeaways
- Small cell lung cancer (SCLC) is an aggressive form of lung cancer with limited current treatment options.
- Clinical trials play a crucial role in developing and improving therapies for SCLC.
- Recent clinical trials have led to breakthroughs, introducing promising new therapies and treatment approaches.
- Challenges in SCLC trials include patient recruitment, side effects, and limited understanding of disease biology.
- Future research focuses on personalized medicine, novel drug combinations, and increased patient involvement in trials.
Current Treatment Options for Small Cell Lung Cancer
The treatment landscape for small cell lung cancer has traditionally been dominated by chemotherapy and radiation therapy. For patients diagnosed with limited stage SCLC, a combination of chemotherapy and thoracic radiation therapy is often employed as the standard treatment approach. The most commonly used chemotherapeutic agents include cisplatin or carboplatin combined with etoposide.
This regimen has been shown to improve survival rates significantly compared to chemotherapy alone. However, despite initial responses to treatment, most patients experience relapse within a year due to the inherent resistance of SCLC to conventional therapies. For extensive stage SCLC, treatment options are more limited, as the disease has already disseminated beyond the lungs.
In this scenario, systemic chemotherapy remains the cornerstone of treatment. The same combination of cisplatin or carboplatin with etoposide is frequently utilized, although newer agents such as topotecan may be considered for patients who have relapsed after initial therapy. Unfortunately, the prognosis for extensive stage SCLC is particularly grim, with median survival rates often falling below one year.
Palliative care also plays a vital role in managing symptoms and improving quality of life for patients facing advanced disease.
Importance of Clinical Trials in Advancing Small Cell Lung Cancer Treatment
Clinical trials are essential for advancing the understanding and treatment of small cell lung cancer. These studies provide a structured framework for evaluating new therapies and treatment combinations that may offer improved outcomes compared to existing standards of care. By participating in clinical trials, patients gain access to cutting-edge treatments that are not yet widely available, while also contributing to the broader scientific knowledge that can benefit future patients.
The rigorous design of clinical trials ensures that new interventions are tested for safety and efficacy before they are approved for general use. Moreover, clinical trials can help identify biomarkers that predict response to specific therapies, allowing for more personalized treatment approaches. For instance, researchers are increasingly exploring the role of genetic profiling in SCLC to identify patients who may benefit from targeted therapies or immunotherapies.
The integration of biomarker-driven strategies into clinical trial designs holds promise for improving patient outcomes by tailoring treatments to individual tumor characteristics. As such, clinical trials not only serve as a platform for innovation but also foster collaboration among researchers, clinicians, and patients in the fight against this challenging disease.
Recent Breakthroughs in Small Cell Lung Cancer Clinical Trials
| Trial Name | Drug/Intervention | Phase | Primary Endpoint | Results | Publication Year |
|---|---|---|---|---|---|
| IMpower133 | Atezolizumab + Chemotherapy | III | Overall Survival (OS) | Median OS improved to 12.3 months vs 10.3 months (HR 0.70) | 2018 |
| CASPIAN | Daratumumab + Chemotherapy | III | Overall Survival (OS) | Median OS 13.9 months vs 10.5 months (HR 0.73) | 2019 |
| CheckMate 032 | Nivolumab ± Ipilimumab | I/II | Objective Response Rate (ORR) | ORR 11% with Nivolumab, 22% with combination | 2017 |
| KEYNOTE-604 | Pembrolizumab + Chemotherapy | III | Progression-Free Survival (PFS) | PFS improved to 4.5 months vs 4.3 months (HR 0.75) | 2020 |
| EA5161 | Nivolumab + Chemotherapy | II | Overall Survival (OS) | Median OS 11.3 months vs 8.5 months (HR 0.67) | 2021 |
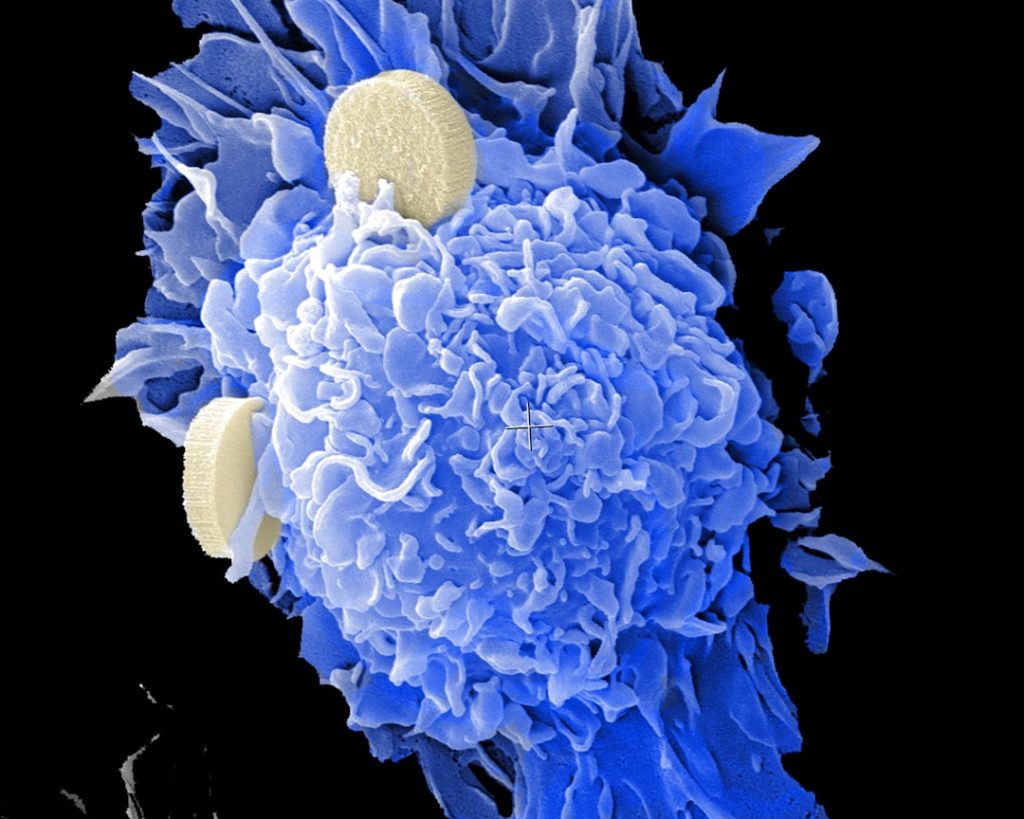
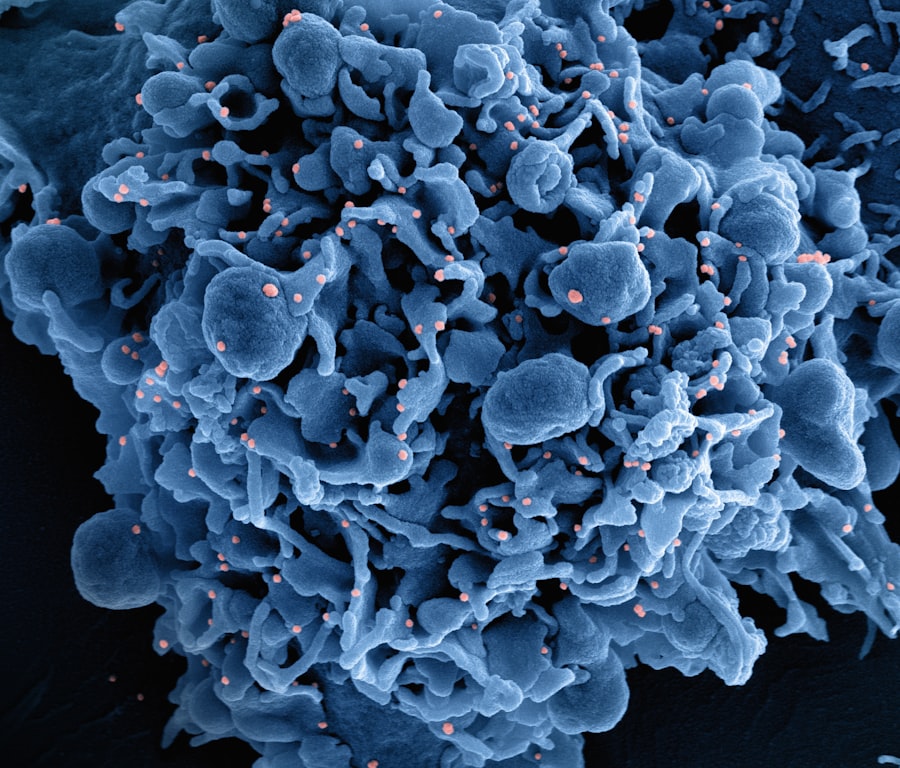
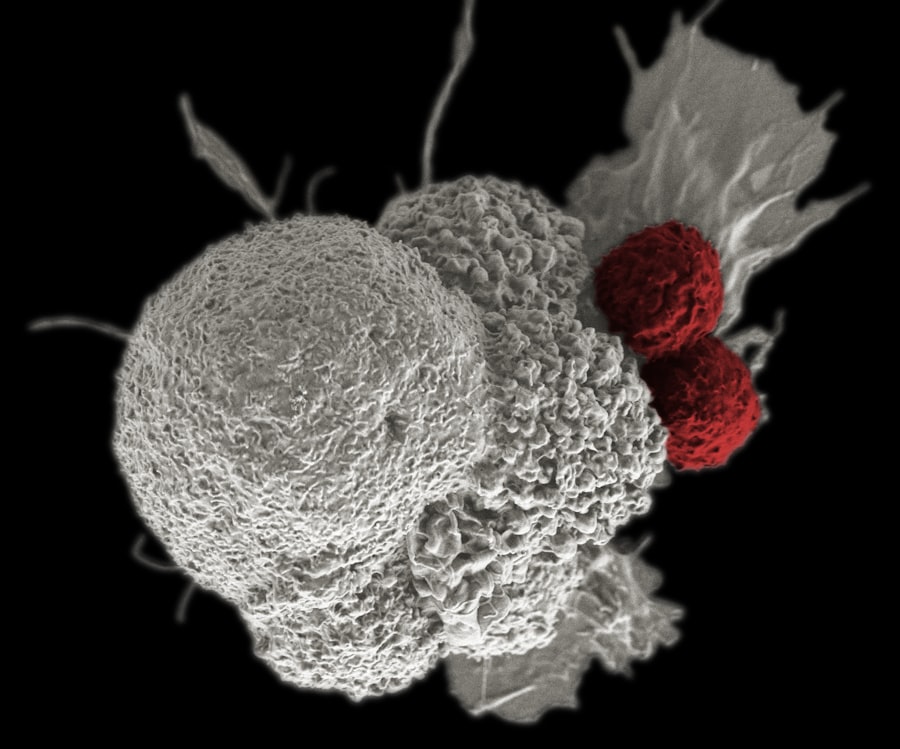
Recent years have witnessed significant breakthroughs in clinical trials focused on small cell lung cancer, particularly in the realm of immunotherapy and targeted therapies. One notable advancement is the introduction of immune checkpoint inhibitors, such as pembrolizumab and nivolumab, which have shown promise in treating SCLC by enhancing the body’s immune response against cancer cells. These agents work by blocking proteins that inhibit immune activation, thereby allowing T-cells to recognize and attack tumor cells more effectively.
Clinical trials have demonstrated that combining these immunotherapies with traditional chemotherapy can lead to improved response rates and overall survival in patients with extensive stage SCLC. Another area of progress involves targeted therapies aimed at specific genetic alterations found in SCLC tumors. For example, research has identified mutations in genes such as NOTCH1 and MYC that may drive tumor growth in some patients.
Targeted agents designed to inhibit these pathways are currently being evaluated in clinical trials. Additionally, novel combinations of existing therapies are being explored to enhance treatment efficacy. For instance, studies investigating the combination of chemotherapy with anti-angiogenic agents or other novel compounds have shown encouraging results in early-phase trials.
These breakthroughs represent a shift towards more innovative and effective treatment paradigms for small cell lung cancer.
Promising New Therapies and Treatment Approaches
The landscape of small cell lung cancer treatment is evolving rapidly with the emergence of promising new therapies and treatment approaches. One such approach is the use of antibody-drug conjugates (ADCs), which combine monoclonal antibodies with cytotoxic drugs to deliver targeted therapy directly to cancer cells while minimizing damage to healthy tissue. For instance, an ADC targeting DLL3—a protein commonly overexpressed in SCLC—has shown encouraging results in early clinical trials.
By selectively delivering potent chemotherapy agents to DLL3-positive tumor cells, these therapies aim to improve response rates while reducing systemic toxicity. Additionally, combination therapies that integrate immunotherapy with traditional chemotherapy or radiation are gaining traction as a means to enhance treatment efficacy. The rationale behind this strategy lies in the potential synergistic effects of these modalities; chemotherapy can induce immunogenic cell death and enhance tumor antigen presentation, thereby priming the immune system for subsequent immunotherapy.
Ongoing clinical trials are investigating various combinations to determine optimal dosing schedules and treatment sequences that maximize patient benefit while minimizing adverse effects.
Challenges and Limitations in Small Cell Lung Cancer Clinical Trials
Despite the advancements made in small cell lung cancer research, several challenges and limitations persist within clinical trials. One significant hurdle is the heterogeneity of SCLC tumors, which can exhibit diverse genetic profiles and varying responses to treatment. This variability complicates trial design and may lead to inconclusive results if patient populations are not adequately stratified based on molecular characteristics.
Furthermore, the rapid progression of SCLC often results in a limited window for patient enrollment in clinical trials, as many patients may not meet eligibility criteria due to advanced disease at diagnosis. Another challenge lies in patient recruitment and retention within clinical trials. Many patients may be hesitant to participate due to concerns about potential side effects or uncertainty regarding new treatments’ effectiveness compared to standard care.
Additionally, logistical barriers such as travel requirements for trial sites can further limit participation among certain populations. Addressing these challenges requires innovative strategies to enhance patient education about clinical trials and improve access to research opportunities across diverse demographics.
Patient Perspectives and Involvement in Clinical Trials
The involvement of patients in clinical trials is crucial not only for advancing research but also for ensuring that studies address their needs and preferences. Patient perspectives can provide valuable insights into treatment tolerability, quality of life considerations, and overall satisfaction with care. Engaging patients throughout the research process—from trial design to implementation—can help ensure that studies are relevant and meaningful to those affected by small cell lung cancer.
Moreover, patient advocacy groups play an essential role in raising awareness about clinical trials and promoting participation among individuals diagnosed with SCLThese organizations often provide resources and support for patients navigating their treatment options while also advocating for increased funding and research initiatives focused on this aggressive cancer type. By fostering collaboration between researchers, clinicians, and patient communities, it becomes possible to create a more patient-centered approach to clinical trial design that prioritizes outcomes that matter most to those living with small cell lung cancer.
Future Directions in Small Cell Lung Cancer Research and Clinical Trials
Looking ahead, future directions in small cell lung cancer research will likely focus on several key areas aimed at improving patient outcomes and expanding treatment options. One promising avenue involves further exploration of personalized medicine approaches that leverage genomic profiling to identify specific mutations or alterations within individual tumors. By tailoring treatments based on these molecular characteristics, researchers hope to enhance therapeutic efficacy while minimizing unnecessary toxicity.
Additionally, ongoing investigations into novel immunotherapeutic strategies—such as CAR T-cell therapy—hold great promise for transforming the treatment landscape for SCLThese approaches aim to harness the power of the immune system more effectively by engineering T-cells to specifically target cancer cells based on unique tumor antigens. As our understanding of SCLC biology continues to evolve, it is anticipated that innovative combination therapies will emerge that integrate multiple modalities—such as immunotherapy, targeted therapy, and traditional chemotherapy—to create more effective treatment regimens. In conclusion, while small cell lung cancer remains a formidable challenge due to its aggressive nature and limited treatment options, ongoing research efforts hold promise for improving outcomes through innovative therapies and personalized approaches.
The collaborative efforts between researchers, clinicians, patients, and advocacy groups will be essential in driving progress forward in this critical area of oncology.