Small cell lung cancer (SCLC) is a highly aggressive form of lung cancer that accounts for approximately 15% of all lung cancer diagnoses. Characterized by its rapid growth and early metastasis, SCLC is often diagnosed at an advanced stage, which significantly complicates treatment options and prognosis. The cancer originates in the neuroendocrine cells of the lungs, leading to the production of hormones and other substances that can cause paraneoplastic syndromes, which are systemic effects not directly related to tumor mass.
The two primary subtypes of SCLC are limited-stage disease (LS-SCLC) and extensive-stage disease (ES-SCLC), with the former being confined to one lung and nearby lymph nodes, while the latter has spread beyond these confines. The clinical presentation of SCLC often includes symptoms such as persistent cough, chest pain, weight loss, and shortness of breath. Due to its aggressive nature, SCLC is typically associated with a poor prognosis, with a five-year survival rate of only about 6%.
The standard treatment regimen for SCLC has historically involved a combination of chemotherapy and radiation therapy. However, the rapid development of resistance to these treatments poses a significant challenge, necessitating ongoing research into more effective therapeutic strategies. Understanding the biology of SCLC and the mechanisms underlying its aggressiveness is crucial for developing innovative treatment approaches.
Key Takeaways
- Small cell lung cancer (SCLC) remains a challenging disease with ongoing clinical trials exploring new treatment options.
- Targeted therapies and immunotherapy have shown promising advancements in improving SCLC patient outcomes.
- Personalized medicine is increasingly important in tailoring clinical trials and treatments to individual SCLC patients.
- Combination therapies are being investigated for their potential to enhance efficacy in SCLC treatment.
- Emerging biomarkers are critical for guiding clinical trial design and future research directions in SCLC.
Overview of Clinical Trials in Small Cell Lung Cancer
Clinical trials play a pivotal role in advancing the understanding and treatment of small cell lung cancer. These trials are essential for evaluating new therapies, assessing their efficacy and safety, and determining optimal treatment regimens. The landscape of clinical trials in SCLC has evolved significantly over the years, with a focus on both traditional chemotherapy regimens and novel therapeutic agents.
Historically, clinical trials have primarily centered on cytotoxic chemotherapy agents such as cisplatin and etoposide, which have formed the backbone of treatment for decades. Recent years have seen a shift towards exploring targeted therapies and immunotherapies in clinical trials for SCLThis shift is driven by a growing understanding of the molecular underpinnings of SCLC and the identification of specific genetic alterations that may be targeted by new drugs. For instance, trials investigating the efficacy of agents targeting the Notch signaling pathway or those inhibiting the poly(ADP-ribose) polymerase (PARP) enzyme have emerged as promising avenues for research.
Additionally, the incorporation of biomarkers into clinical trial design has become increasingly important, allowing for more personalized approaches to treatment based on individual patient characteristics.
Advancements in Targeted Therapies for Small Cell Lung Cancer
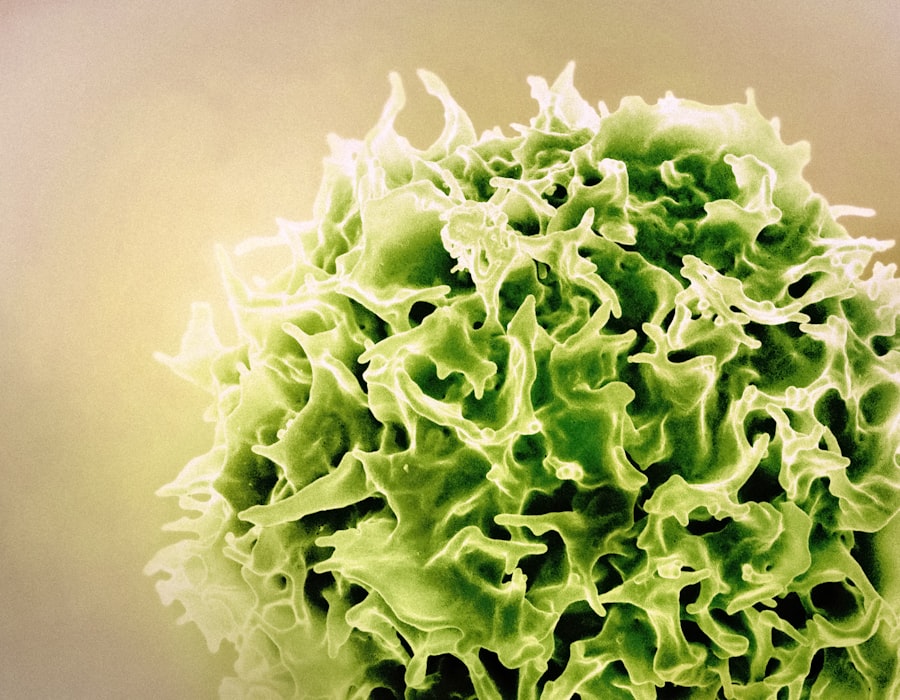
Targeted therapies represent a significant advancement in the treatment landscape for small cell lung cancer, offering the potential for more effective and less toxic treatment options compared to traditional chemotherapy. These therapies are designed to specifically target molecular abnormalities present in cancer cells, thereby inhibiting their growth and survival. One notable example is the development of inhibitors targeting the receptor tyrosine kinases (RTKs), which are often dysregulated in SCLC.
One promising targeted therapy currently under investigation is the use of inhibitors against the fibroblast growth factor receptor (FGFR). Preclinical studies have demonstrated that FGFR signaling plays a critical role in SCLC cell proliferation and survival. By inhibiting this pathway, researchers aim to disrupt the growth signals that drive tumor progression.
Additionally, agents targeting the insulin-like growth factor receptor (IGF-1R) have shown potential in early-phase clinical trials, suggesting that targeting these pathways may improve outcomes for patients with SCLC. Another area of focus in targeted therapy research is the use of small molecules that inhibit specific genetic mutations associated with SCLFor instance, alterations in the TP53 gene are common in SCLC and contribute to its aggressive behavior. Researchers are exploring ways to develop therapies that can restore normal function to mutated TP53 or exploit its loss to enhance sensitivity to existing treatments.
These advancements highlight the importance of understanding the genetic landscape of SCLC to inform targeted therapeutic strategies.
Immunotherapy and its Impact on Small Cell Lung Cancer
| Metric | Value | Details |
|---|---|---|
| Overall Response Rate (ORR) | 20-30% | Percentage of patients showing tumor size reduction with immunotherapy |
| Median Overall Survival (mOS) | 9-12 months | Survival time after treatment initiation with immunotherapy |
| Progression-Free Survival (PFS) | 4-6 months | Time during and after treatment that a patient lives without disease progression |
| Common Immunotherapy Agents | Atezolizumab, Durvalumab, Nivolumab, Pembrolizumab | Checkpoint inhibitors targeting PD-L1 or PD-1 pathways |
| Adverse Event Rate | 15-25% | Percentage of patients experiencing immune-related side effects |
| First-line Treatment Impact | Improved survival by ~2-3 months | Immunotherapy combined with chemotherapy vs chemotherapy alone |
| Second-line Treatment Response | 10-15% | Response rate in patients treated with immunotherapy after relapse |
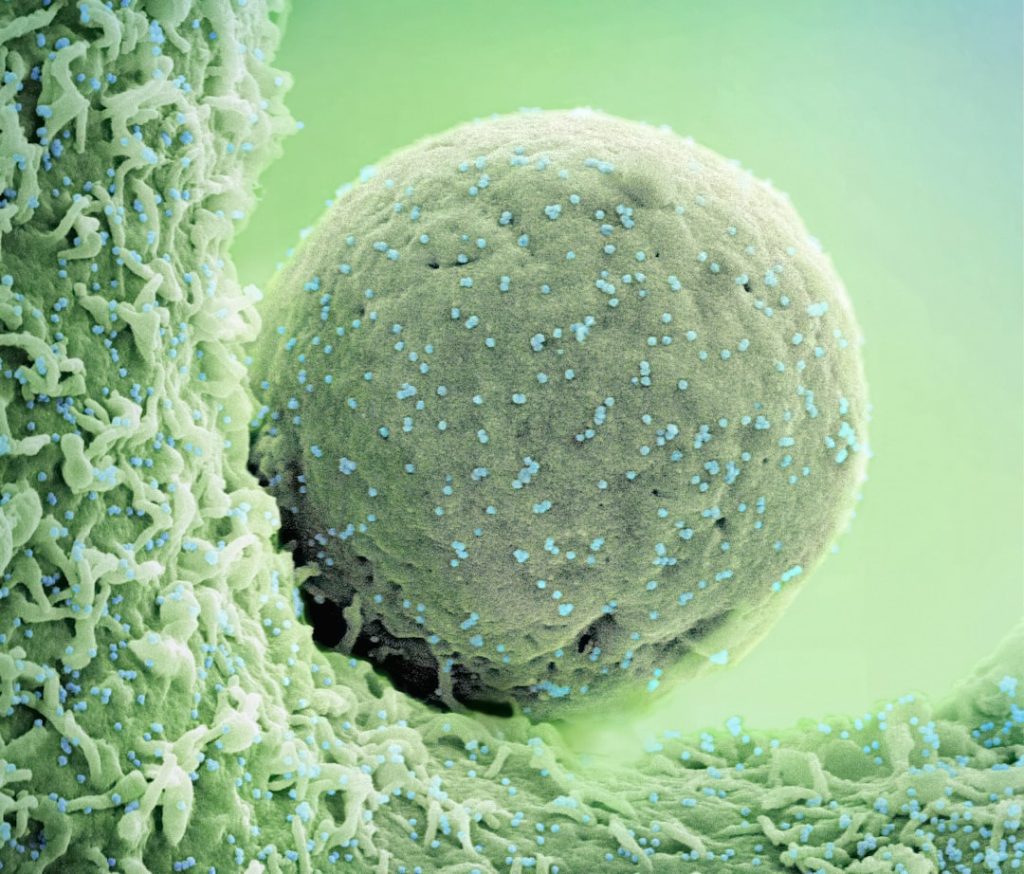
Immunotherapy has emerged as a groundbreaking approach in oncology, offering new hope for patients with various malignancies, including small cell lung cancer. This therapeutic strategy harnesses the body’s immune system to recognize and attack cancer cells more effectively. In SCLC, where traditional treatments have often fallen short, immunotherapy has shown promise in improving outcomes for patients.
One of the most significant advancements in immunotherapy for SCLC has been the development of immune checkpoint inhibitors, such as pembrolizumab and nivolumab. These agents work by blocking proteins that inhibit immune responses, thereby enhancing T-cell activity against tumor cells. Clinical trials have demonstrated that these checkpoint inhibitors can lead to durable responses in a subset of patients with SCLC, particularly those with extensive-stage disease who have progressed after first-line chemotherapy.
Moreover, combination strategies involving immunotherapy and chemotherapy are being actively explored in clinical trials. The rationale behind this approach is that chemotherapy can induce immunogenic cell death, potentially enhancing the effectiveness of subsequent immunotherapy. Early results from studies combining immune checkpoint inhibitors with standard chemotherapy regimens have shown improved response rates and overall survival compared to chemotherapy alone.
This combination approach represents a paradigm shift in how SCLC is treated and underscores the importance of integrating immunotherapy into standard care protocols.
Personalized Medicine and its Role in Small Cell Lung Cancer Clinical Trials
Personalized medicine aims to tailor treatment strategies based on individual patient characteristics, including genetic makeup, tumor biology, and response to previous therapies. In small cell lung cancer, where heterogeneity among tumors can significantly impact treatment outcomes, personalized approaches are particularly relevant. Clinical trials focusing on personalized medicine are increasingly incorporating biomarker-driven strategies to identify patients who are most likely to benefit from specific therapies.
One example of personalized medicine in SCLC is the use of genomic profiling to identify actionable mutations or alterations within tumors. By analyzing tumor samples for specific genetic changes, researchers can stratify patients into subgroups that may respond differently to targeted therapies or immunotherapies. For instance, patients with tumors harboring mutations in genes such as RB1 or TP53 may exhibit distinct responses to certain treatments compared to those without these alterations.
Additionally, ongoing clinical trials are exploring the use of circulating tumor DNA (ctDNA) as a biomarker for monitoring treatment response and detecting minimal residual disease. This non-invasive approach allows for real-time assessment of tumor dynamics and may guide treatment decisions based on emerging resistance mechanisms. As personalized medicine continues to evolve within the context of SCLC clinical trials, it holds promise for improving patient outcomes through more tailored therapeutic interventions.
Combination Therapies and their Potential in Small Cell Lung Cancer Treatment
Combination therapies have gained traction as a promising strategy for enhancing treatment efficacy in small cell lung cancer. Given the aggressive nature of SCLC and its propensity for rapid progression, relying solely on monotherapy may not yield optimal outcomes. By combining different therapeutic modalities—such as chemotherapy, targeted therapy, and immunotherapy—researchers aim to exploit synergistic effects that can lead to improved response rates and prolonged survival.
One notable combination approach currently under investigation involves pairing traditional chemotherapy agents with novel targeted therapies or immunotherapies. For example, studies are exploring the combination of platinum-based chemotherapy with immune checkpoint inhibitors like atezolizumab or durvalumab. Early-phase clinical trials have shown encouraging results, indicating that this combination may enhance overall survival compared to chemotherapy alone.
Furthermore, researchers are also examining combinations that target multiple pathways simultaneously. For instance, combining inhibitors of both FGFR and PD-1/PD-L1 pathways may provide a dual mechanism of action that could overcome resistance mechanisms commonly observed in SCLThis multi-faceted approach not only aims to improve treatment efficacy but also addresses the challenge of tumor heterogeneity by targeting various aspects of cancer biology.
Emerging Biomarkers and their Significance in Small Cell Lung Cancer Clinical Trials
The identification and validation of emerging biomarkers hold significant promise for advancing clinical trials in small cell lung cancer. Biomarkers can provide critical insights into tumor behavior, predict treatment response, and guide therapeutic decision-making. In recent years, researchers have focused on discovering novel biomarkers that can enhance patient stratification and improve outcomes in clinical trials.
One area of interest is the exploration of immune-related biomarkers that may predict response to immunotherapy in SCLC patients. For instance, high levels of PD-L1 expression on tumor cells have been associated with improved responses to immune checkpoint inhibitors. Ongoing clinical trials are investigating whether specific immune signatures can serve as predictive markers for patient selection in immunotherapy-based regimens.
Additionally, circulating biomarkers such as ctDNA are gaining traction as potential indicators of treatment response and disease progression. By analyzing ctDNA levels before and during treatment, researchers aim to identify changes that correlate with clinical outcomes. This real-time monitoring could enable clinicians to make timely adjustments to treatment plans based on emerging resistance or disease recurrence.
Future Directions in Small Cell Lung Cancer Research and Clinical Trials
The future landscape of small cell lung cancer research is poised for significant advancements driven by ongoing clinical trials and innovative therapeutic strategies. As our understanding of the molecular mechanisms underlying SCLC deepens, researchers are increasingly focused on developing novel agents that target specific pathways involved in tumor growth and metastasis. One promising direction involves leveraging advances in genomics and proteomics to identify new therapeutic targets within SCLC tumors.
By utilizing high-throughput sequencing technologies, researchers can uncover previously unrecognized mutations or alterations that may be amenable to targeted therapies. This approach not only enhances our understanding of SCLC biology but also opens avenues for developing personalized treatment strategies tailored to individual patients. Moreover, collaborative efforts between academia and industry are essential for accelerating drug development processes and bringing new therapies into clinical practice more rapidly.
Multi-institutional clinical trials that incorporate diverse patient populations will be crucial for validating findings across different demographics and ensuring equitable access to emerging treatments. As we look ahead, integrating novel therapeutic modalities such as gene therapy or CAR-T cell therapy into clinical trials represents an exciting frontier in SCLC research. These innovative approaches hold potential for transforming treatment paradigms and improving outcomes for patients facing this challenging disease.
The commitment to advancing research efforts will ultimately pave the way for more effective interventions and improved quality of life for individuals diagnosed with small cell lung cancer.