Targeted therapies represent a significant advancement in disease treatment, particularly for cancer. These treatments differ from conventional chemotherapy by selectively targeting cancer cells rather than affecting all rapidly dividing cells throughout the body. This selectivity is achieved by identifying specific molecular markers or genetic mutations that are present in tumor cells but absent or less prevalent in healthy tissue.
The mechanism of targeted therapies involves binding to or interfering with specific proteins, enzymes, or cellular pathways that cancer cells depend on for growth, survival, or metastasis. This approach typically results in reduced toxicity to normal cells and fewer adverse effects compared to traditional cytotoxic chemotherapy. Advances in molecular biology and genomic sequencing have accelerated the development of targeted therapies by enabling researchers to map the genetic alterations that drive cancer progression.
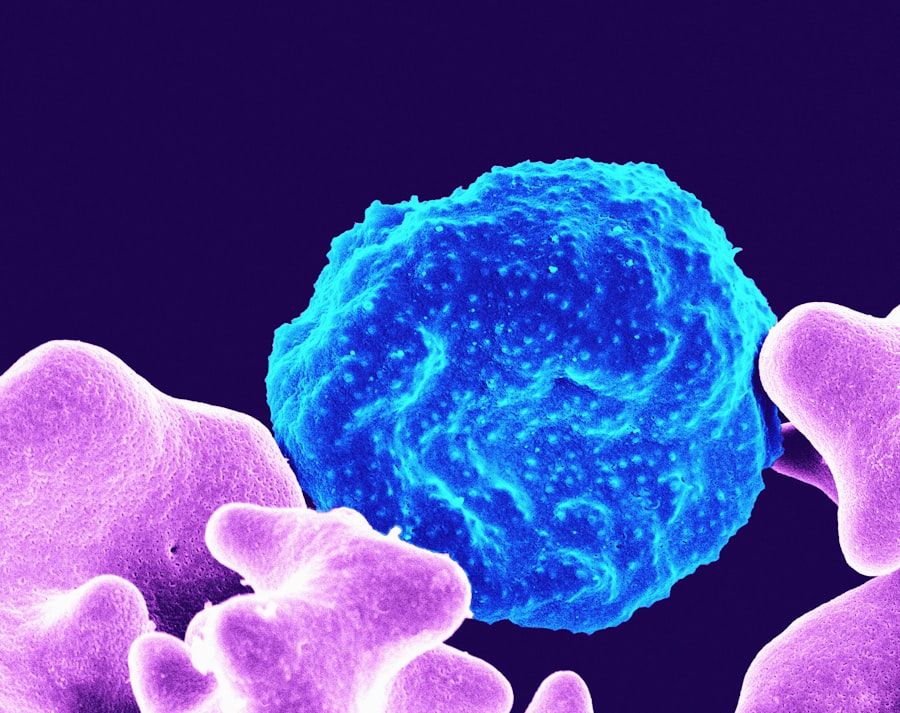
These technologies have revealed that cancers contain multiple genetic mutations and molecular abnormalities that can serve as therapeutic targets. Current targeted therapy approaches include monoclonal antibodies that bind to specific cell surface receptors, small molecule inhibitors that block intracellular signaling pathways, and immunotherapies that enhance the immune system’s ability to recognize and eliminate cancer cells. These treatments can be used alone or in combination with other therapeutic modalities.
The clinical application of targeted therapies often requires companion diagnostic testing to identify patients whose tumors express the specific molecular targets. This approach enables precision medicine strategies where treatment selection is based on the individual molecular characteristics of each patient’s tumor rather than solely on tumor location or histological type.
Key Takeaways
- Targeted therapies have revolutionized cancer treatment by specifically attacking cancer cells while sparing healthy tissue.
- These therapies work through various mechanisms, including inhibiting specific molecules involved in tumor growth and progression.
- Significant advancements have been made in developing targeted treatments for cancers such as lung, breast, and melanoma.
- Clinical trials demonstrate improved efficacy and survival rates, though challenges like resistance and side effects remain.
- Future directions focus on overcoming limitations, personalizing treatments, and integrating novel targets to enhance clinical outcomes.
Evolution of Targeted Therapies in Cancer Treatment
The journey of targeted therapies began in the late 20th century when researchers first recognized that certain cancers were driven by specific genetic mutations. The approval of imatinib (Gleevec) in 2001 marked a significant milestone in this evolution. Imatinib was designed to inhibit the BCR-ABL fusion protein, which is responsible for chronic myeloid leukemia (CML).
Its success demonstrated that targeting specific molecular abnormalities could lead to remarkable clinical responses and improved survival rates. This breakthrough paved the way for further research into other targeted agents and solidified the concept that cancer treatment could be tailored to the molecular characteristics of individual tumors. As the field progressed, the focus expanded beyond hematological malignancies to solid tumors, leading to the development of therapies targeting various oncogenes and tumor suppressor genes.
For instance, trastuzumab (Herceptin) was introduced for HER2-positive breast cancer, while gefitinib (Iressa) and erlotinib (Tarceva) were developed for non-small cell lung cancer (NSCLC) with EGFR mutations. These advancements underscored the importance of biomarker testing in guiding treatment decisions and highlighted the growing recognition that cancer is not a single disease but a collection of heterogeneous disorders requiring tailored therapeutic approaches.
Mechanisms of Action of Targeted Therapies
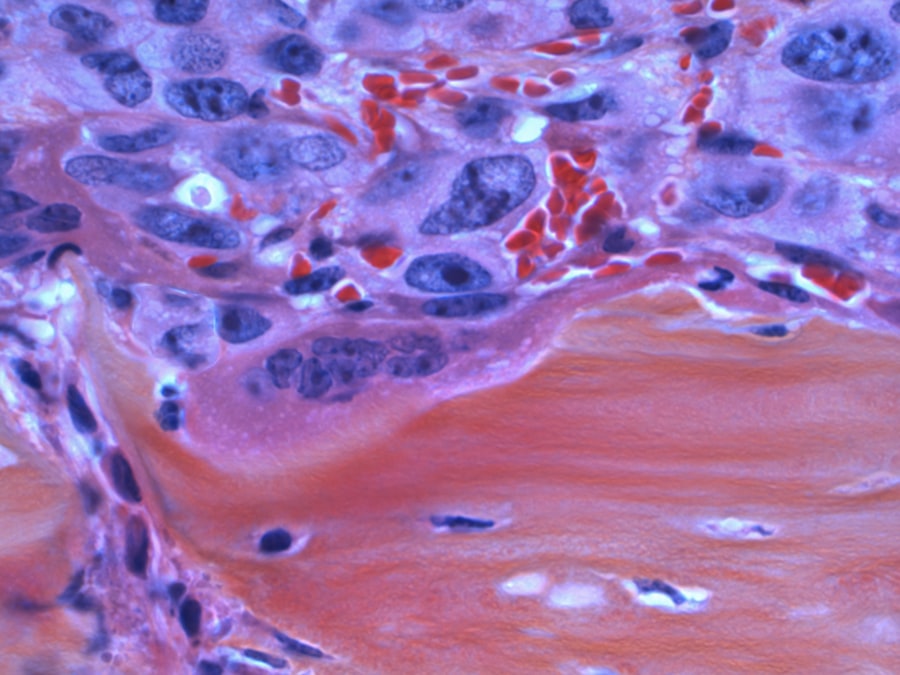
Targeted therapies operate through various mechanisms that disrupt the signaling pathways essential for cancer cell proliferation and survival. One common approach involves inhibiting specific proteins that drive tumor growth. For example, small molecule tyrosine kinase inhibitors (TKIs) like imatinib block the activity of tyrosine kinases involved in cell signaling pathways that promote cancer cell division.
By preventing these signals from being transmitted, TKIs effectively halt tumor progression. Another mechanism involves monoclonal antibodies that bind to specific antigens on the surface of cancer cells. Trastuzumab, for instance, binds to the HER2 receptor, inhibiting its signaling and marking the cancer cell for destruction by the immune system.
This dual action not only impedes tumor growth but also enhances immune-mediated cytotoxicity. Additionally, some targeted therapies are designed to induce apoptosis, or programmed cell death, in cancer cells by activating specific pathways that lead to cell death while leaving normal cells unharmed.
Advancements in Targeted Therapies for Specific Cancer Types
The landscape of targeted therapies has evolved significantly, with numerous advancements tailored to specific cancer types. In breast cancer, for example, the introduction of CDK4/6 inhibitors such as palbociclib has transformed treatment paradigms for hormone receptor-positive breast cancer. These agents work by inhibiting cyclin-dependent kinases involved in cell cycle regulation, thereby preventing cancer cells from proliferating.
The combination of CDK4/6 inhibitors with endocrine therapy has shown improved progression-free survival rates compared to endocrine therapy alone. In lung cancer, targeted therapies have made substantial strides with the identification of actionable mutations. The emergence of ALK inhibitors like crizotinib and alectinib has provided new options for patients with ALK-positive NSCLThese agents specifically target the ALK fusion protein, leading to significant tumor shrinkage and prolonged survival.
Furthermore, the development of next-generation EGFR inhibitors such as osimertinib has addressed resistance mechanisms associated with earlier generations of EGFR TKIs, offering hope for patients with acquired resistance.
Clinical Trials and Efficacy of Targeted Therapies
| Metric | Value | Year | Source |
|---|---|---|---|
| Impact Factor | 10.199 | 2023 | Journal Citation Reports |
| 5-Year Impact Factor | 11.345 | 2023 | Journal Citation Reports |
| h-index | 120 | 2023 | Scopus |
| Acceptance Rate | 18% | 2023 | Journal Website |
| Average Time to Publication | 45 days | 2023 | Journal Website |
| Publisher | American Association for Cancer Research | – | Journal Website |
| Frequency | Monthly | – | Journal Website |
Clinical trials play a crucial role in evaluating the efficacy and safety of targeted therapies. The success of these trials is often measured by objective response rates, progression-free survival, and overall survival. For instance, pivotal trials involving trastuzumab demonstrated a significant improvement in overall survival for patients with HER2-positive breast cancer compared to those receiving chemotherapy alone.
Such findings have led to its incorporation into standard treatment regimens. Moreover, ongoing clinical trials continue to explore novel combinations of targeted therapies and their potential synergistic effects. For example, combining immune checkpoint inhibitors with targeted agents is an area of active investigation, as it may enhance anti-tumor responses by leveraging both targeted inhibition and immune activation.
The results from these trials will further refine treatment strategies and provide insights into optimizing patient outcomes based on individual tumor characteristics.
Challenges and Limitations of Targeted Therapies
Despite their promise, targeted therapies are not without challenges and limitations. One significant issue is the development of resistance, which can occur through various mechanisms such as secondary mutations in target genes or activation of alternative signaling pathways. For instance, patients treated with EGFR inhibitors may initially respond well but later develop resistance due to mutations like T790M that render these agents ineffective.
This necessitates ongoing research into next-generation inhibitors or combination strategies that can overcome resistance. Additionally, the identification of suitable biomarkers for patient selection remains a critical challenge. Not all patients with a particular cancer type will benefit from a specific targeted therapy due to the heterogeneity within tumors.
The reliance on biomarker testing can also lead to delays in treatment initiation if results are not available promptly. Furthermore, access to targeted therapies can be limited by factors such as cost and availability, particularly in low-resource settings where comprehensive genomic testing may not be feasible.
Future Directions in Targeted Therapies
The future of targeted therapies is poised for exciting developments as research continues to uncover new molecular targets and refine existing treatment strategies. One promising direction is the integration of artificial intelligence and machine learning into drug discovery and patient stratification processes. These technologies can analyze vast datasets to identify novel biomarkers and predict patient responses to specific therapies more accurately.
Additionally, the concept of combination therapy is gaining traction as researchers explore synergistic effects between different classes of agents. Combining targeted therapies with immunotherapies or other modalities may enhance treatment efficacy and mitigate resistance mechanisms. Furthermore, ongoing investigations into personalized medicine aim to tailor treatment plans based on an individual’s unique genetic makeup and tumor profile, ensuring that patients receive the most effective interventions.
Conclusion and Implications for Clinical Practice
The advent of targeted therapies has revolutionized cancer treatment by providing more effective and personalized options for patients. As our understanding of cancer biology deepens and new therapeutic agents are developed, clinicians must remain vigilant in adapting their practices to incorporate these advancements. The integration of biomarker testing into routine clinical practice will be essential for optimizing treatment decisions and improving patient outcomes.
Moreover, ongoing education and collaboration among healthcare professionals will be crucial in navigating the complexities associated with targeted therapies. As challenges such as resistance and access persist, a concerted effort is needed to ensure that all patients benefit from these innovative treatments. Ultimately, the future of oncology lies in harnessing the power of targeted therapies to create more effective, individualized treatment strategies that enhance survival and quality of life for patients battling cancer.



