Clinical phase trials constitute a fundamental component in the development of medical interventions, including pharmaceuticals, vaccines, and therapeutic procedures. These systematically designed studies evaluate the safety and efficacy of treatments in human participants following completion of preclinical research conducted in laboratory and animal models. Clinical trials serve as the essential mechanism for determining whether experimental treatments can be safely and effectively administered to patients, bridging the gap between scientific research and clinical application.
Clinical trials are organized into sequential phases, each with specific objectives and methodological approaches. These phases systematically assess treatment effects, monitor adverse events, and collect data necessary for regulatory evaluation. The structured design of clinical trials protects participant safety while ensuring that new therapies meet established standards for approval by regulatory agencies, including the U.S.
Food and Drug Administration (FDA) and the European Medicines Agency (EMA). Clinical phase trials therefore represent an indispensable element in medical research and the development of therapeutic interventions that enhance patient care and treatment outcomes.
Key Takeaways
- Clinical phase trials are essential for testing the safety and effectiveness of new medical treatments.
- Each phase of clinical trials has specific objectives, from assessing safety to evaluating efficacy and side effects.
- Participants play a crucial role in advancing medical knowledge and treatment options.
- Ethical considerations and challenges, such as informed consent and risk management, are vital in conducting trials.
- Innovations and future developments in clinical trials promise to enhance healthcare outcomes and treatment accessibility.
The Importance of Clinical Phase Trials in Advancing Medicine
Clinical phase trials are indispensable in the landscape of modern medicine, serving as the primary mechanism through which new treatments are validated before they reach the market. The importance of these trials cannot be overstated; they provide the empirical evidence needed to support claims about a treatment’s safety and effectiveness. Without clinical trials, healthcare providers would lack the necessary data to make informed decisions about patient care, potentially leading to the use of ineffective or harmful treatments.
Moreover, clinical phase trials contribute significantly to the body of medical knowledge. They not only assess the efficacy of new interventions but also enhance understanding of disease mechanisms and patient responses. For instance, the development of targeted therapies for cancer has been propelled by clinical trials that explore genetic markers and their relationship to treatment outcomes.
These studies have led to personalized medicine approaches, where treatments are tailored to individual patient profiles based on genetic information. This shift towards precision medicine underscores the vital role that clinical phase trials play in evolving healthcare practices and improving therapeutic strategies.
The Different Phases of Clinical Trials and Their Objectives
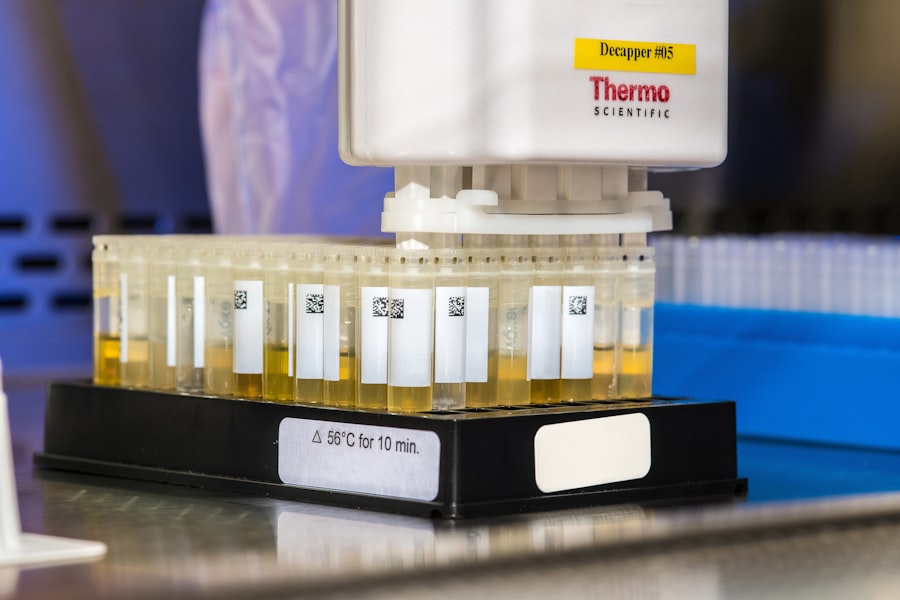
Clinical trials are typically divided into four distinct phases, each with specific goals and methodologies. Phase I trials are primarily concerned with safety; they involve a small number of healthy volunteers or patients and aim to determine the maximum tolerated dose of a new treatment while monitoring for adverse effects. This phase is crucial for identifying any potential toxicity before larger-scale testing occurs.
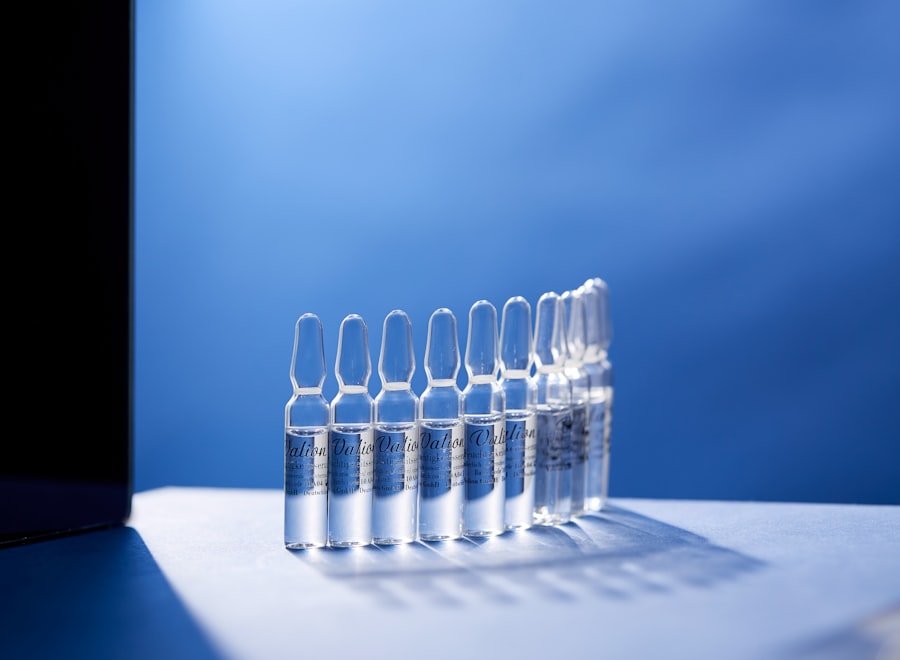
For example, in the development of a new chemotherapy agent, Phase I trials would focus on establishing safe dosage levels while observing how the drug is metabolized in the body. Phase II trials expand on the findings of Phase I by assessing both safety and efficacy in a larger group of participants who have the condition that the treatment aims to address. These trials often involve hundreds of patients and are designed to provide preliminary data on how well the treatment works.
For instance, a Phase II trial for a new diabetes medication might evaluate its ability to lower blood sugar levels compared to a placebo. The results from this phase help researchers determine whether to proceed to Phase III trials, which are larger-scale studies designed to confirm efficacy and monitor adverse reactions in diverse populations. Phase III trials are pivotal as they involve thousands of participants across multiple sites and are often randomized and controlled.
These trials provide comprehensive data on the treatment’s effectiveness compared to standard therapies or placebos. The results from Phase III trials are critical for regulatory approval; they must demonstrate that the new treatment offers significant benefits over existing options. Finally, Phase IV trials occur post-marketing and focus on long-term effects and rare side effects in a broader population once the treatment is available to the public.
The Role of Participants in Clinical Phase Trials
Participants in clinical phase trials play an essential role in advancing medical research. Their involvement is not merely as subjects but as active contributors to the scientific process. By volunteering for these studies, participants provide invaluable data that can lead to breakthroughs in treatment options for various diseases.
Each participant’s experience contributes to a larger understanding of how a treatment works across different demographics, including age, gender, ethnicity, and comorbidities. The recruitment process for clinical trials is often rigorous, as researchers seek individuals who meet specific inclusion criteria while also ensuring diversity among participants. This diversity is crucial for understanding how different populations respond to treatments.
For example, a trial for a cardiovascular drug may include participants from various ethnic backgrounds to assess how genetic factors influence drug metabolism and efficacy. Additionally, informed consent is a fundamental aspect of participation; individuals must be fully aware of potential risks and benefits before enrolling in a trial. This ethical consideration ensures that participants make informed decisions about their involvement.
Challenges and Ethical Considerations in Clinical Phase Trials
| Clinical Phase | Purpose | Number of Participants | Duration | Success Rate (%) | Key Metrics |
|---|---|---|---|---|---|
| Phase 1 | Safety and dosage | 20-100 healthy volunteers | Several months | 70% | Adverse effects, pharmacokinetics |
| Phase 2 | Efficacy and side effects | 100-300 patients | Several months to 2 years | 33% | Therapeutic efficacy, optimal dose |
| Phase 3 | Confirm effectiveness, monitor side effects | 1,000-3,000 patients | 1-4 years | 25-30% | Comparison to standard treatment, safety |
| Phase 4 | Post-marketing surveillance | Various | Ongoing | N/A | Long-term effects, rare side effects |
Despite their importance, clinical phase trials face numerous challenges and ethical considerations that must be navigated carefully. One significant challenge is recruitment; finding enough eligible participants can be difficult, particularly for rare diseases or conditions with strict inclusion criteria. Additionally, there may be hesitancy among potential participants due to concerns about safety or mistrust in medical research, particularly among marginalized communities that have historically been subjected to unethical practices.
Ethical considerations also extend to issues such as informed consent, data privacy, and the management of adverse events. Researchers must ensure that participants fully understand what participation entails, including potential risks and benefits. This process requires clear communication and transparency about the study’s purpose and procedures.
Furthermore, maintaining participant confidentiality is paramount; researchers must implement robust data protection measures to safeguard personal information. Another ethical dilemma arises when considering placebo-controlled trials, particularly when effective treatments already exist. In such cases, researchers must weigh the scientific necessity of using a placebo against the moral obligation to provide participants with the best available care.
This balance is critical in maintaining public trust in clinical research while ensuring that scientific integrity is upheld.
Advancements and Innovations in Clinical Phase Trials
The landscape of clinical phase trials is continually evolving, driven by advancements in technology and innovative methodologies that enhance efficiency and effectiveness. One notable trend is the increasing use of digital health technologies, such as mobile health applications and wearable devices, which facilitate real-time data collection and monitoring of participants’ health status outside traditional clinical settings. These innovations allow researchers to gather more comprehensive data on treatment effects while improving participant engagement and adherence.
Additionally, adaptive trial designs have gained traction in recent years. Unlike traditional fixed designs, adaptive trials allow modifications to be made during the study based on interim results. This flexibility can lead to more efficient use of resources and faster identification of effective treatments.
For instance, if early results indicate that a particular dosage is significantly more effective than others being tested, researchers can adjust the trial accordingly rather than waiting until its conclusion. Moreover, advancements in genomics and personalized medicine have transformed how clinical trials are conducted. Biomarker-driven studies enable researchers to identify specific patient populations that are more likely to benefit from certain treatments based on genetic profiles.
This approach not only enhances the likelihood of success but also minimizes exposure to ineffective therapies for those unlikely to respond.
The Future of Clinical Phase Trials and Their Impact on Healthcare
Looking ahead, the future of clinical phase trials appears promising as ongoing innovations continue to reshape their design and implementation. The integration of artificial intelligence (AI) into trial design holds significant potential for optimizing participant selection, predicting outcomes, and analyzing vast datasets more efficiently than traditional methods allow. AI algorithms can identify patterns within complex data sets that may not be immediately apparent to human researchers, leading to more informed decision-making throughout the trial process.
Furthermore, decentralized clinical trials are emerging as a viable alternative to traditional site-based studies. By leveraging telemedicine and remote monitoring technologies, these trials allow participants to engage from their homes while still providing valuable data for researchers. This model not only enhances accessibility for participants but also broadens the demographic reach of studies by including individuals who may have difficulty traveling to clinical sites due to geographical or health-related barriers.
The impact of these advancements on healthcare could be profound. As clinical phase trials become more efficient and inclusive, they will likely accelerate the development of new therapies that address unmet medical needs across diverse populations. This evolution could lead to improved patient outcomes and a more responsive healthcare system capable of adapting quickly to emerging health challenges.
The Ongoing Impact of Clinical Phase Trials on Medicine
Clinical phase trials remain at the forefront of medical research, serving as essential mechanisms for validating new treatments before they reach patients. Their structured approach ensures that safety and efficacy are rigorously evaluated while contributing significantly to our understanding of diseases and therapeutic interventions. As we continue to navigate challenges related to recruitment, ethics, and data management, ongoing innovations promise to enhance the efficiency and inclusivity of these trials.
The future landscape of clinical phase trials will likely be characterized by greater integration of technology, personalized medicine approaches, and adaptive designs that respond dynamically to emerging data. As these advancements unfold, they will not only transform how clinical research is conducted but also significantly impact patient care by facilitating faster access to effective therapies. The ongoing evolution of clinical phase trials underscores their vital role in shaping the future of medicine and improving health outcomes for individuals worldwide.



