Clinical trials serve as the cornerstone of modern medical research, providing a structured framework for evaluating the safety and efficacy of new treatments, drugs, and medical devices. These trials are essential for translating scientific discoveries into practical applications that can improve patient care and health outcomes. By rigorously testing hypotheses in controlled environments, clinical trials help to ensure that new interventions are not only effective but also safe for human use.
The process involves multiple phases, each designed to answer specific research questions, ranging from initial safety assessments to large-scale efficacy studies. The significance of clinical trials extends beyond the immediate results they yield. They contribute to the broader body of medical knowledge, informing clinical guidelines and shaping healthcare policies.
For instance, the results from pivotal trials can lead to the approval of new medications by regulatory bodies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA). This regulatory approval is crucial for making new therapies available to patients who may benefit from them.
Moreover, clinical trials often pave the way for innovative treatment approaches, such as personalized medicine, which tailors therapies based on individual patient characteristics.
Key Takeaways
- Clinical trials are essential for developing new medical treatments and improving patient care.
- Case Report Forms (CRFs) play a critical role in accurately collecting and managing clinical trial data.
- CRFs enhance data quality and streamline analysis, contributing to more reliable trial outcomes.
- Despite their benefits, CRFs face challenges such as complexity, data entry errors, and compliance issues.
- Ethical considerations and best practices are vital to ensure CRFs support transparent and responsible clinical research.
Understanding the Role of CRFs in Clinical Trials
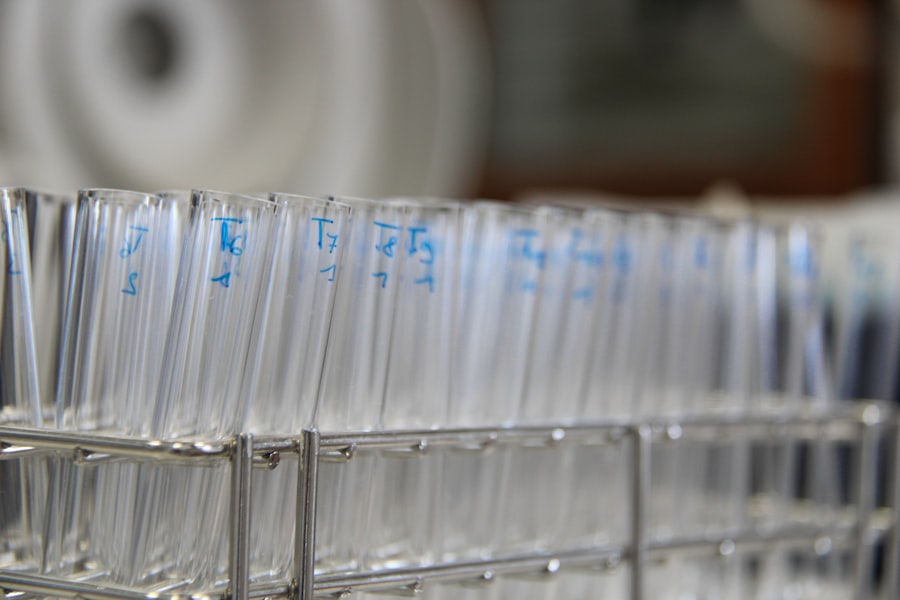
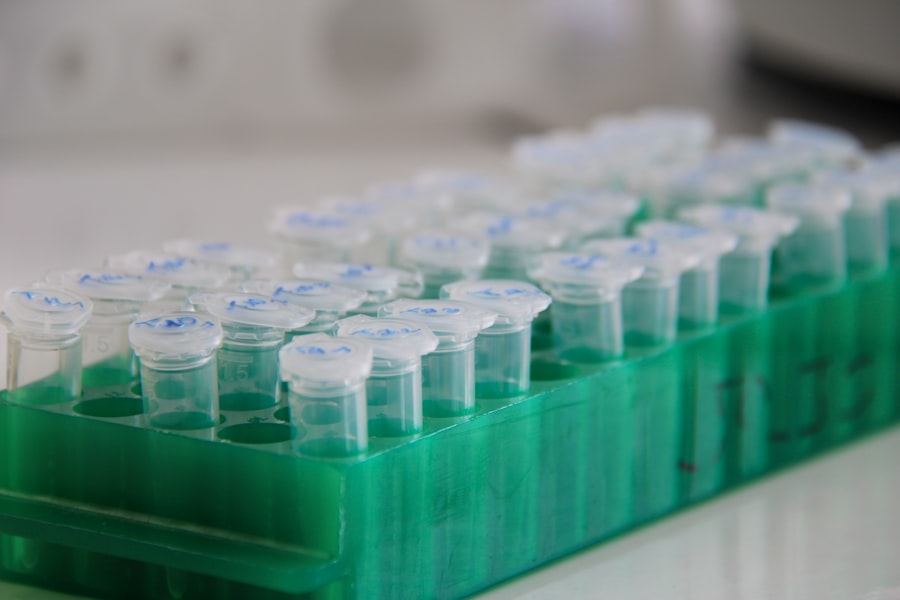
Case Report Forms (CRFs) are vital tools in the realm of clinical trials, serving as standardized documents used to collect data from each participant in a study. These forms are meticulously designed to capture a wide array of information, including demographic details, medical history, treatment regimens, and outcomes. The design of CRFs is critical; they must be user-friendly to ensure that data collectors can complete them accurately and efficiently while also being comprehensive enough to gather all necessary information for analysis.
The role of CRFs extends beyond mere data collection; they are integral to maintaining the integrity and reliability of the trial’s findings. By standardizing how data is recorded, CRFs help minimize variability and bias that could arise from different interpretations or methods of data entry. This standardization is particularly important in multicenter trials where data is collected across various locations and by different personnel.
A well-structured CRF ensures that all sites adhere to the same protocols, thereby enhancing the overall quality of the data collected.
The Impact of CRFs on Data Collection and Analysis
The design and implementation of CRFs have a profound impact on both data collection and subsequent analysis in clinical trials. A thoughtfully constructed CRF can streamline the data entry process, reducing the likelihood of errors and omissions that could compromise the validity of the study’s results. For example, incorporating checkboxes or dropdown menus can facilitate quicker data entry compared to open-ended questions, which may lead to inconsistencies in responses.
This efficiency is particularly crucial in large-scale trials where thousands of participants may be involved. Moreover, CRFs play a pivotal role in ensuring that data is collected in a manner that aligns with the study’s objectives. By clearly defining endpoints and outcomes, CRFs guide researchers in gathering relevant information that directly addresses the research questions posed by the trial.
This alignment is essential for robust statistical analysis, as it allows researchers to apply appropriate methodologies to interpret the data accurately. Inadequate or poorly designed CRFs can lead to incomplete datasets, which may ultimately skew results and hinder the ability to draw meaningful conclusions.
The Advantages of Using CRFs in Clinical Trials
| Advantage | Description | Impact on Clinical Trials | Example Metric |
|---|---|---|---|
| Improved Data Accuracy | CRFs standardize data collection, reducing errors and inconsistencies. | Higher data quality leads to more reliable trial outcomes. | Reduction in data entry errors by up to 30% |
| Enhanced Data Completeness | Mandatory fields and validation checks ensure all necessary data is captured. | Minimizes missing data, improving statistical power. | Decrease in missing data points by 25% |
| Streamlined Data Management | Facilitates easier data aggregation and monitoring. | Speeds up data cleaning and analysis phases. | Reduction in data processing time by 20% |
| Regulatory Compliance | CRFs help ensure data collection meets regulatory standards. | Supports audit readiness and approval processes. | 100% compliance with regulatory data standards |
| Facilitates Remote Monitoring | Electronic CRFs enable real-time data access for monitors. | Improves oversight and timely issue resolution. | Monitoring visit efficiency increased by 15% |
The advantages of utilizing CRFs in clinical trials are manifold. One of the primary benefits is the enhancement of data quality. By standardizing data collection processes, CRFs help ensure that information is gathered consistently across all participants and sites.
This consistency is crucial for maintaining the integrity of the trial and for producing reliable results that can be generalized to broader populations. Furthermore, high-quality data is essential for regulatory submissions, as it underpins the evidence required for drug approval. Another significant advantage of CRFs is their ability to facilitate regulatory compliance.
Regulatory agencies require that clinical trials adhere to strict guidelines regarding data collection and reporting. Well-designed CRFs can help ensure that all necessary information is captured in accordance with these regulations, thereby reducing the risk of non-compliance issues that could delay or jeopardize a trial’s progress. Additionally, CRFs can aid in tracking adverse events and other safety-related information, which is critical for protecting participant welfare throughout the study.
Challenges and Limitations of CRFs in Clinical Trials
Despite their numerous advantages, CRFs are not without challenges and limitations. One major issue is the potential for complexity in their design. While it is essential for CRFs to be comprehensive, overly complicated forms can lead to confusion among data collectors and participants alike.
This complexity can result in incomplete or inaccurate data entry, ultimately compromising the quality of the study’s findings. Striking a balance between thoroughness and simplicity is a critical consideration when developing CRFs. Another challenge lies in the adaptability of CRFs to evolving research needs.
Clinical trials often undergo modifications based on interim findings or changes in regulatory requirements. Updating CRFs mid-study can be cumbersome and may lead to inconsistencies if not managed carefully. Additionally, training staff on new versions of CRFs can be time-consuming and may disrupt ongoing data collection efforts.
These challenges underscore the importance of careful planning and foresight during the design phase to create flexible yet robust CRFs that can accommodate potential changes.
Best Practices for Implementing CRFs in Clinical Trials
Implementing effective CRFs requires adherence to best practices that enhance their utility and effectiveness in clinical trials. One key practice is involving stakeholders from various disciplines during the design phase. Engaging clinicians, biostatisticians, data managers, and regulatory experts ensures that all perspectives are considered, leading to a more comprehensive and functional CRF.
This collaborative approach can help identify potential pitfalls early on and foster a sense of ownership among team members. Another best practice involves conducting pilot testing of CRFs before full-scale implementation. Pilot testing allows researchers to identify any issues with clarity or usability that may not have been apparent during the design phase.
Feedback from pilot participants can inform necessary adjustments, ensuring that the final version of the CRF is user-friendly and effective at capturing required data. Additionally, ongoing training and support for staff involved in data collection are crucial for maintaining high standards throughout the trial.
The Future of CRFs in Advancing Medicine
As technology continues to evolve, so too does the landscape of clinical trials and the role of CRFs within them. The integration of electronic data capture (EDC) systems has revolutionized how CRFs are utilized, allowing for real-time data entry and monitoring. These systems can enhance data accuracy by minimizing manual entry errors and enabling automated validation checks.
Furthermore, EDC platforms often come equipped with advanced analytics tools that facilitate immediate insights into trial progress and participant safety. Looking ahead, there is potential for further innovation in CRF design through advancements in artificial intelligence (AI) and machine learning (ML). These technologies could enable adaptive CRF designs that evolve based on incoming data trends or participant responses, allowing for more dynamic trial management.
Additionally, AI-driven analytics could enhance data interpretation by identifying patterns or correlations that may not be immediately apparent through traditional analysis methods. Such advancements hold promise for accelerating drug development timelines and improving patient outcomes.
Ethical Considerations in CRFs and Clinical Trials
Ethical considerations are paramount in clinical trials, particularly concerning how data is collected and reported through CRFs. Informed consent is a fundamental ethical principle that must be upheld throughout the research process. Participants should be fully aware of what information will be collected via CRFs and how it will be used.
Transparency regarding data handling practices fosters trust between researchers and participants, which is essential for successful trial enrollment and retention. Moreover, safeguarding participant confidentiality is a critical ethical obligation when designing CRFs. Personal identifiers should be minimized or anonymized wherever possible to protect sensitive information from unauthorized access or disclosure.
Researchers must also adhere to relevant regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or General Data Protection Regulation (GDPR) in Europe when handling personal health information. Ethical considerations must remain at the forefront throughout all stages of clinical trials to ensure that participant rights are respected while advancing medical knowledge through rigorous research practices.




