Phase 1 clinical trials constitute the initial stage of human testing in drug development, primarily focused on evaluating the safety and tolerability of investigational therapeutic compounds. These studies examine pharmacokinetics—the processes of drug absorption, distribution, metabolism, and elimination—alongside pharmacodynamics, which measures the biological effects and mechanisms of action. Phase 1 trials typically enroll 20-100 participants, consisting of either healthy volunteers or patients with the target condition, depending on the drug’s characteristics and safety profile.
The primary objectives of Phase 1 trials include establishing the maximum tolerated dose, identifying dose-limiting toxicities, and determining the recommended dose for subsequent studies. Researchers employ dose-escalation protocols, gradually increasing drug concentrations across participant cohorts to map the relationship between dosage and adverse effects. These trials also provide initial data on biomarkers, drug interactions, and optimal administration schedules.
Phase 1 results serve as the regulatory foundation for advancing to Phase 2 trials, where therapeutic efficacy becomes the primary endpoint. The Food and Drug Administration and other regulatory agencies require comprehensive Phase 1 safety data before approving progression to larger-scale studies. Approximately 70% of drugs that complete Phase 1 trials advance to Phase 2, though only a fraction ultimately receive market approval.
The data generated during Phase 1 testing directly influences study design, patient selection criteria, and risk-benefit assessments for all subsequent clinical phases.
Key Takeaways
- Phase 1 clinical trials are the first step in testing new treatments for safety and dosage in humans.
- These trials are crucial for advancing medical knowledge and developing effective therapies.
- The process involves careful monitoring of participants to assess safety and side effects.
- Ethical considerations and challenges, such as informed consent and risk management, are central to Phase 1 trials.
- Innovations in Phase 1 trials are shaping the future of medicine by improving patient care and accelerating drug development.
Importance of Phase 1 Clinical Trials in Advancing Medicine
The importance of Phase 1 clinical trials cannot be overstated, as they serve as the gateway for new therapies to enter the clinical landscape. These trials are instrumental in identifying safe dosage levels and understanding how different populations may respond to a new drug. For instance, variations in metabolism due to genetic differences can lead to significant disparities in drug efficacy and safety among individuals.
By conducting Phase 1 trials, researchers can gather data that helps tailor treatments to specific patient populations, ultimately enhancing therapeutic outcomes. Moreover, Phase 1 trials play a vital role in fostering innovation within the pharmaceutical industry. As researchers explore novel compounds and therapeutic approaches—such as biologics, gene therapies, and immunotherapies—Phase 1 trials provide the necessary framework to evaluate these cutting-edge treatments.
The insights gained from these early studies can lead to breakthroughs that not only advance medical science but also offer hope to patients with previously untreatable conditions. For example, recent advancements in immunotherapy for cancer have emerged from findings obtained during Phase 1 trials, demonstrating how these initial studies can catalyze significant progress in treatment options.
Understanding the Process of Phase 1 Clinical Trials
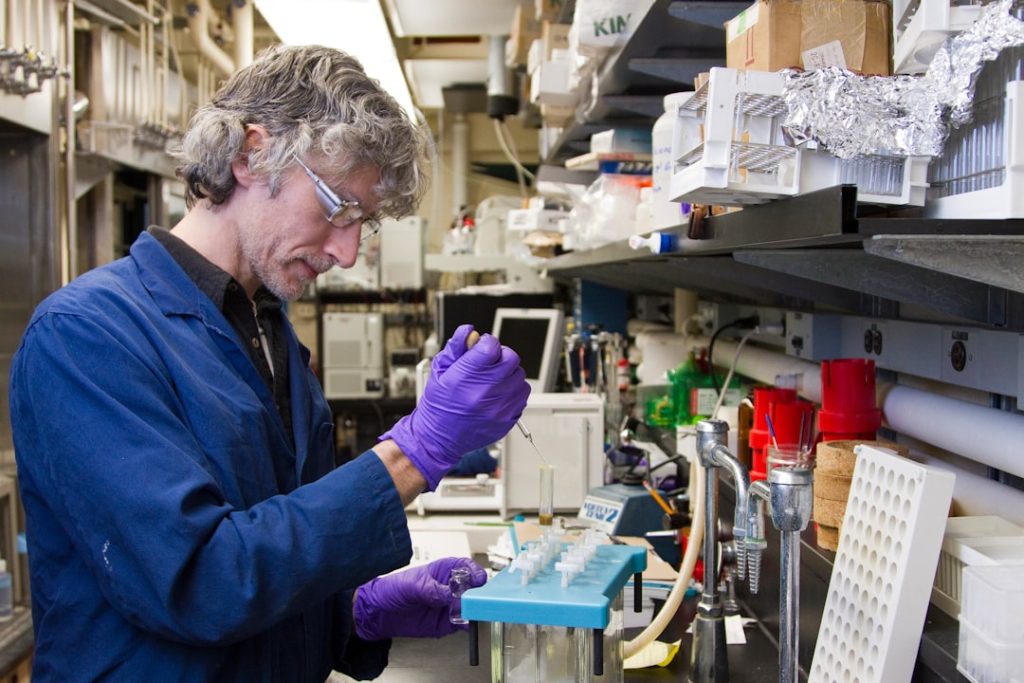
The process of conducting Phase 1 clinical trials is meticulously structured and governed by strict regulatory guidelines to ensure participant safety and data integrity. Initially, researchers must develop a comprehensive protocol that outlines the trial’s objectives, design, methodology, and statistical analysis plan. This protocol undergoes rigorous review by institutional review boards (IRBs) to ensure ethical standards are met and that participants are adequately informed about potential risks.
Once approved, recruitment begins, often targeting healthy volunteers or patients with specific conditions relevant to the investigational drug. Participants undergo thorough screening processes to assess their eligibility based on predefined inclusion and exclusion criteria. This step is crucial for minimizing confounding variables that could skew results.
After enrollment, participants receive the investigational drug at varying doses in a controlled environment, allowing researchers to monitor their responses closely. Data collection during this phase includes regular health assessments, laboratory tests, and adverse event reporting, all aimed at building a comprehensive safety profile for the drug.
Current Breakthroughs and Discoveries in Phase 1 Clinical Trials
Recent years have witnessed remarkable breakthroughs emerging from Phase 1 clinical trials across various therapeutic areas. One notable example is the development of CAR T-cell therapy for certain types of blood cancers. In early Phase 1 trials, researchers observed that genetically modified T-cells could effectively target and eliminate cancer cells in patients with refractory leukemia and lymphoma.
These initial findings not only demonstrated the potential efficacy of this innovative approach but also paved the way for subsequent trials that led to FDA approvals for several CAR T-cell therapies. Another area where Phase 1 trials have made significant contributions is in the realm of rare diseases. For instance, gene therapies targeting genetic disorders such as spinal muscular atrophy (SMA) have emerged from early-phase studies that assessed safety and dosing regimens.
The success of these trials has led to transformative treatments that address the underlying genetic causes of diseases rather than merely alleviating symptoms. Such advancements underscore how Phase 1 trials can catalyze progress in areas where traditional therapies have been limited or nonexistent.
Challenges and Ethical Considerations in Phase 1 Clinical Trials
| Metric | Description | Typical Range/Value |
|---|---|---|
| Number of Participants | Number of healthy volunteers or patients enrolled | 20 – 100 |
| Primary Objective | Assess safety and tolerability of the investigational drug | Safety and dose-limiting toxicities |
| Secondary Objective | Evaluate pharmacokinetics and pharmacodynamics | Drug absorption, distribution, metabolism, excretion |
| Duration | Length of the trial phase | Several months (1-2 years depending on drug) |
| Study Design | Type of clinical trial design used | Open-label, dose-escalation, single ascending dose |
| Adverse Events | Frequency and severity of side effects observed | Monitored and recorded; usually mild to moderate |
| Maximum Tolerated Dose (MTD) | Highest dose with acceptable toxicity | Determined during dose escalation |
| Placebo Control | Use of placebo group for comparison | Sometimes used, but not always |
Despite their critical role in drug development, Phase 1 clinical trials are not without challenges and ethical dilemmas. One significant concern is the recruitment of participants, particularly when healthy volunteers are involved. The ethical implications of exposing individuals to potential risks for the sake of advancing medical knowledge raise questions about informed consent and participant autonomy.
Researchers must ensure that volunteers fully understand the nature of the trial, including potential side effects and long-term implications. Additionally, there is an ongoing debate regarding the use of placebo controls in Phase 1 trials. While placebos can provide valuable comparative data on drug efficacy, they may also pose ethical challenges when participants are deprived of potentially beneficial treatments.
Striking a balance between scientific rigor and ethical responsibility is paramount in designing these studies. Regulatory bodies often require robust justification for placebo use, particularly when effective treatments already exist for the condition being studied.
Impact of Phase 1 Clinical Trials on Patient Care and Treatment
The impact of Phase 1 clinical trials on patient care extends far beyond the immediate outcomes of individual studies; they fundamentally shape treatment paradigms and influence clinical practice guidelines. The data generated from these early-phase trials inform subsequent research phases and ultimately determine which therapies become available to patients. As new drugs demonstrate safety and efficacy through rigorous testing, they can lead to paradigm shifts in how diseases are managed.
For instance, advancements in targeted therapies for cancer have transformed treatment approaches for various malignancies. Insights gained from Phase 1 trials have led to the identification of specific biomarkers that guide treatment decisions, allowing clinicians to tailor therapies based on individual patient profiles. This personalized medicine approach enhances treatment effectiveness while minimizing unnecessary side effects associated with less targeted interventions.
Future Directions and Innovations in Phase 1 Clinical Trials
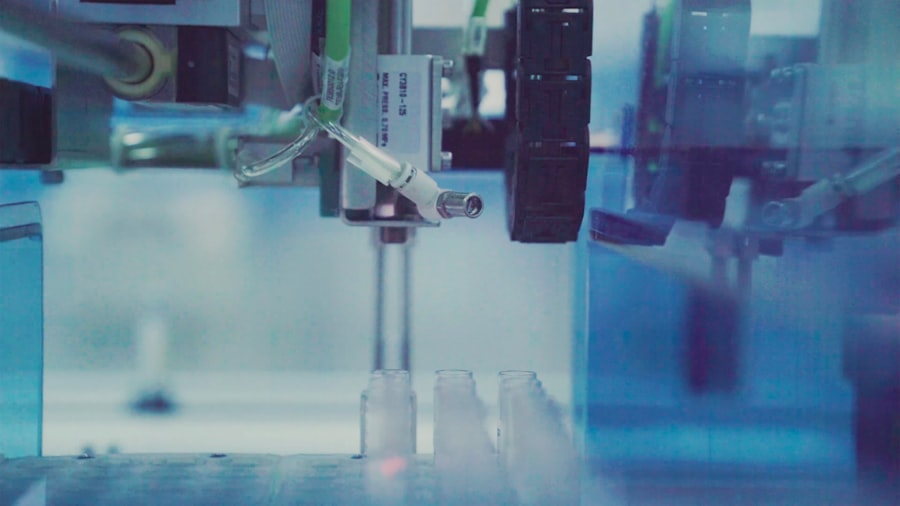
Looking ahead, the landscape of Phase 1 clinical trials is poised for significant transformation driven by technological advancements and innovative methodologies. One promising direction is the integration of real-world evidence (RWE) into trial designs. By leveraging data from electronic health records and patient registries, researchers can gain insights into how new therapies perform outside controlled clinical settings.
This approach not only enhances understanding of drug safety but also facilitates more efficient trial designs that reflect diverse patient populations. Moreover, advancements in artificial intelligence (AI) and machine learning are beginning to play a role in optimizing trial designs and patient recruitment strategies. These technologies can analyze vast datasets to identify suitable candidates for participation based on genetic profiles or historical responses to similar treatments.
By streamlining recruitment processes and enhancing patient stratification, AI-driven approaches hold promise for accelerating the pace of drug development while maintaining rigorous safety standards.
The Role of Phase 1 Clinical Trials in Shaping the Future of Medicine
Phase 1 clinical trials serve as a cornerstone in the continuum of medical research, providing essential insights that drive innovation and improve patient care. As we continue to navigate an era marked by rapid advancements in biotechnology and personalized medicine, the importance of these early-phase studies will only grow. They not only facilitate the introduction of novel therapies but also contribute to our understanding of disease mechanisms and treatment responses.
The ongoing evolution of Phase 1 clinical trials—characterized by enhanced ethical considerations, technological integration, and a focus on patient-centered outcomes—will undoubtedly shape the future landscape of medicine. As researchers strive to balance scientific inquiry with ethical responsibility, Phase 1 trials will remain pivotal in ensuring that new treatments are both safe and effective for diverse patient populations worldwide.