Clinical trials are a cornerstone of modern medicine, serving as the bridge between laboratory research and the delivery of new therapies to patients. These meticulously designed studies are essential for determining the safety and efficacy of new drugs, medical devices, and treatment protocols. By adhering to rigorous scientific standards, clinical trials provide the evidence needed to support regulatory approval and clinical practice.
The process is not only vital for advancing medical knowledge but also for ensuring that patients receive treatments that are both effective and safe. The journey of a new treatment begins long before it reaches the clinical trial stage. It starts with basic research, where scientists explore biological mechanisms and potential therapeutic targets.
Once a promising candidate emerges, it undergoes a series of preclinical tests to evaluate its safety and biological activity. Only after these preliminary assessments can a treatment enter the clinical trial phase, which is divided into several distinct stages, each with specific objectives and methodologies. Understanding this progression is crucial for grasping how new therapies are developed and brought to market.
Key Takeaways
- Clinical trials progress through phases I to III, focusing on safety, efficacy, and large-scale testing.
- Preclinical research is essential for initial drug development before human trials.
- Regulatory approval depends on successful trial outcomes and thorough data review.
- Post-market surveillance (Phase IV) monitors long-term effects after drug approval.
- Future clinical trials aim to incorporate advanced technologies and personalized medicine.
Preclinical Research and Development
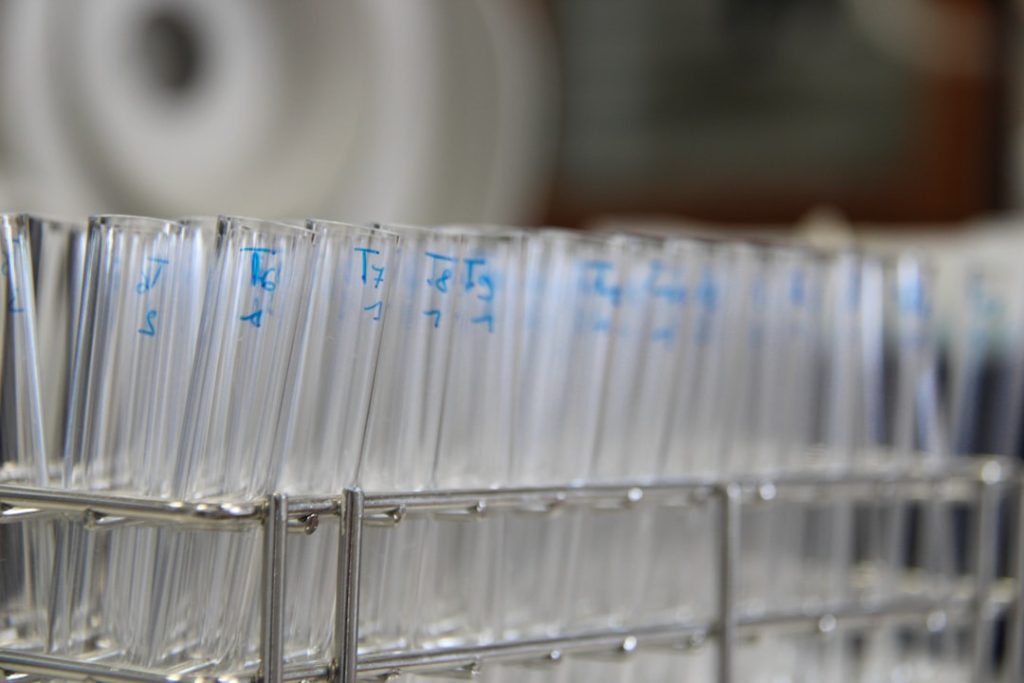
Preclinical research is a critical phase in the development of new medical interventions, serving as the foundation upon which clinical trials are built. This stage typically involves laboratory experiments and animal studies designed to assess the pharmacological properties of a drug candidate. Researchers evaluate how the drug interacts with biological systems, its absorption, distribution, metabolism, and excretion (ADME), as well as its potential toxicity.
These studies are essential for identifying any adverse effects that could arise from human use and for determining appropriate dosing regimens. In addition to safety assessments, preclinical research also focuses on establishing the therapeutic potential of a drug. This involves testing its efficacy in various disease models, which can include cell cultures or animal models that mimic human diseases.
For instance, a new cancer drug might be tested in mice implanted with human tumor cells to observe its effects on tumor growth. The data generated during this phase is crucial for informing the design of subsequent clinical trials, as it helps researchers identify the most promising candidates for human testing and refine their hypotheses about how the drug will perform in patients.
Phase I Clinical Trials: Safety and Dosage

Phase I clinical trials mark the first time a new drug is administered to humans, typically involving a small group of healthy volunteers or patients. The primary objective of this phase is to assess the safety profile of the drug, including any potential side effects and the appropriate dosage range. Researchers closely monitor participants for adverse reactions, which can provide critical insights into how the drug behaves in the human body.
This phase often employs a dose-escalation design, where participants receive gradually increasing doses until side effects become unacceptable or therapeutic effects are observed. In addition to safety assessments, Phase I trials also gather preliminary pharmacokinetic data, which helps researchers understand how the drug is absorbed, distributed, metabolized, and excreted in humans. For example, if a new antihypertensive medication is being tested, researchers will measure how quickly it lowers blood pressure and how long its effects last.
This information is vital for determining optimal dosing schedules for future trials. While Phase I trials typically involve a small number of participants—often fewer than 100—their findings lay the groundwork for subsequent phases by establishing a safe starting point for larger studies.
Phase II Clinical Trials: Efficacy and Side Effects
Once a drug has demonstrated an acceptable safety profile in Phase I trials, it progresses to Phase II trials, which focus on evaluating its efficacy and further assessing its safety in a larger group of participants. This phase typically involves several hundred patients who have the condition that the drug aims to treat. The primary goal is to determine whether the drug produces a beneficial effect on the disease or condition being targeted.
Researchers often use randomized controlled trial designs to compare outcomes between those receiving the experimental treatment and those receiving a placebo or standard therapy. In addition to efficacy, Phase II trials continue to monitor side effects and adverse reactions, providing more comprehensive data on the drug’s safety profile. For instance, if a new antidepressant is being tested, researchers will not only assess improvements in mood but also track any side effects such as weight gain or sexual dysfunction.
This dual focus on efficacy and safety helps refine dosing strategies and informs decisions about whether to advance to Phase III trials. The results from Phase II trials are critical for determining whether a drug has sufficient therapeutic potential to warrant further investigation in larger populations.
Phase III Clinical Trials: Large-Scale Testing
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety and dosage | 20-100 healthy volunteers | Several months | Safety, side effects, pharmacokinetics | 60-70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Effectiveness, optimal dose, short-term side effects | 30-40% |
| Phase 3 | Confirm effectiveness and monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Comparison to standard treatments, long-term safety | 25-30% |
| Phase 4 | Post-marketing surveillance | Various (thousands) | Ongoing | Long-term effects, rare side effects, real-world use | N/A |
Phase III clinical trials represent a pivotal moment in the drug development process, as they involve large-scale testing of the treatment in diverse patient populations across multiple sites. These trials typically enroll thousands of participants and are designed to provide definitive evidence regarding the drug’s efficacy and safety compared to existing treatments or placebos. The results from Phase III trials are crucial for regulatory approval, as they offer comprehensive data that can influence clinical practice guidelines.
The design of Phase III trials often includes randomization and blinding to minimize bias and ensure that results are reliable. For example, if a new cancer therapy is being tested against standard chemotherapy, participants may be randomly assigned to receive either treatment without knowing which one they are receiving. This rigorous methodology helps ensure that any observed differences in outcomes can be attributed to the treatment itself rather than external factors.
Additionally, Phase III trials may also explore different patient demographics or disease stages to assess how well the drug performs across various populations.
Regulatory Approval and Market Access

Following successful completion of Phase III trials, the next step is seeking regulatory approval from agencies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA). This process involves submitting a New Drug Application (NDA) or Marketing Authorization Application (MAA), which includes all data from preclinical studies and clinical trials, along with information about manufacturing processes and proposed labeling.
Regulatory agencies meticulously review this information to ensure that the drug meets established standards for safety, efficacy, and quality. Once approved, gaining market access involves navigating additional hurdles such as pricing negotiations and reimbursement decisions by healthcare payers. In many countries, regulatory approval does not automatically guarantee that a drug will be covered by insurance plans or included in national health systems.
Pharmaceutical companies often engage in discussions with payers to establish pricing models that reflect the drug’s value while ensuring patient access. This complex interplay between regulatory approval and market access underscores the importance of not only demonstrating clinical efficacy but also addressing economic considerations in healthcare.
Post-Market Surveillance and Phase IV Trials
After a drug receives regulatory approval and enters the market, post-market surveillance becomes essential for monitoring its long-term safety and effectiveness in real-world settings. This ongoing assessment helps identify any rare or unexpected adverse events that may not have been evident during clinical trials due to limited sample sizes or short follow-up periods. Regulatory agencies often require manufacturers to conduct Phase IV trials or post-marketing studies to gather additional data on long-term outcomes and safety profiles.
Phase IV trials can take various forms, including observational studies that track patient outcomes over time or randomized controlled trials designed to answer specific questions about the drug’s use in broader populations. For instance, if a new diabetes medication is approved, a Phase IV study might investigate its long-term effects on cardiovascular health among diverse patient groups. These studies not only contribute valuable information about the drug’s performance but also help inform clinical guidelines and best practices for its use.
Future Directions in Clinical Trial Progress
The landscape of clinical trials is evolving rapidly due to advancements in technology, data analytics, and patient engagement strategies. One significant trend is the increasing use of digital health technologies such as wearable devices and mobile health applications that enable real-time monitoring of patient health data during trials. These innovations can enhance data collection efficiency and provide more comprehensive insights into treatment effects outside traditional clinical settings.
Moreover, there is a growing emphasis on patient-centered approaches in trial design, which prioritize patient preferences and experiences throughout the research process. Engaging patients as active partners can lead to more relevant study endpoints and improved recruitment strategies. Additionally, adaptive trial designs are gaining traction, allowing researchers to modify trial parameters based on interim results without compromising scientific integrity.
This flexibility can accelerate drug development timelines while ensuring that patient safety remains paramount. As we look ahead, the integration of artificial intelligence (AI) and machine learning into clinical trial processes holds great promise for optimizing study designs and identifying suitable patient populations more efficiently. By harnessing vast amounts of data from electronic health records and genomic databases, researchers can better predict which patients are likely to benefit from specific treatments.
This shift towards precision medicine not only enhances trial efficiency but also aligns with broader trends in personalized healthcare, ultimately leading to more effective therapies tailored to individual patient needs.