Phase 2 clinical trials constitute an intermediate stage in drug development, positioned between Phase 1 safety studies and Phase 3 large-scale efficacy trials. These studies typically enroll 100 to 300 participants who have the medical condition the investigational drug is designed to treat. The primary goal is to evaluate the drug’s therapeutic effectiveness while maintaining ongoing safety monitoring.
Phase 2 results determine whether a treatment demonstrates sufficient efficacy to justify progression to larger-scale testing. Phase 2 studies commonly utilize randomized, controlled trial methodology, comparing participants receiving the experimental treatment against those receiving either a placebo or established standard treatment. This approach reduces potential bias and provides more reliable efficacy data.
Phase 2 trials are frequently divided into two substages: Phase 2a studies focus on determining optimal dosing through dose-ranging investigations, while Phase 2b studies emphasize efficacy confirmation and continued safety evaluation. The data generated from Phase 2 trials directly influences regulatory and sponsor decisions regarding advancement to Phase 3 trials, which involve substantially larger participant populations and increased regulatory oversight.
Key Takeaways
- Phase 2 clinical research focuses on evaluating the safety and efficacy of promising treatments in a targeted patient group.
- Identifying suitable treatments involves rigorous preclinical data and initial human testing outcomes.
- Recruiting appropriate participants is crucial for obtaining reliable and generalizable trial results.
- Conducting trials requires strict adherence to protocols to ensure data integrity and participant safety.
- Analyzing and reporting findings transparently guides future research directions and regulatory decisions.
Identifying Promising Treatments
The identification of promising treatments for Phase 2 trials often stems from the insights gained during Phase 1 studies, where initial safety and pharmacokinetics are evaluated. Researchers analyze data from these early trials to determine which compounds exhibit favorable characteristics, such as acceptable toxicity levels and preliminary signs of efficacy. This process may involve various methodologies, including biomarker analysis, genetic profiling, and patient stratification based on specific disease characteristics.
For instance, in oncology, targeted therapies may be selected based on the presence of specific mutations in tumor DNA that indicate a higher likelihood of response. Moreover, the selection of promising treatments is not solely based on clinical data; it also incorporates insights from preclinical studies and real-world evidence. Researchers may look at animal models or previous studies involving similar compounds to gauge potential effectiveness.
The integration of patient feedback and experiences can also play a crucial role in identifying treatments that resonate with patient needs and preferences. For example, if a particular treatment shows promise in alleviating symptoms that significantly impact quality of life, it may be prioritized for further investigation in Phase 2 trials.
Assessing Safety and Efficacy

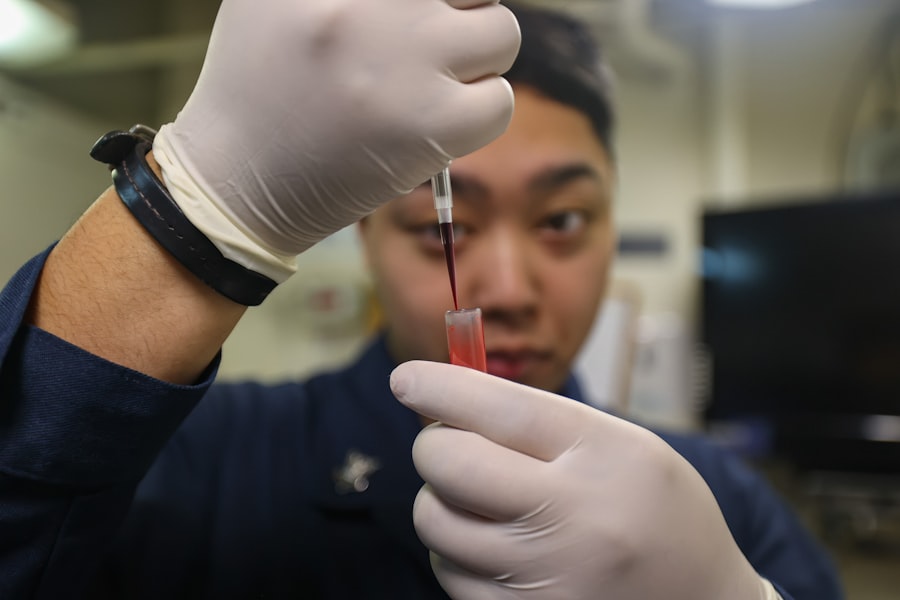
In Phase 2 clinical trials, assessing both safety and efficacy is paramount. While safety assessments continue from Phase 1, they become more nuanced as researchers gather data from a larger cohort of participants. Adverse events are meticulously documented, and researchers employ various tools to monitor participants’ health throughout the trial.
This includes regular laboratory tests, physical examinations, and patient-reported outcomes. The goal is to identify any potential side effects that may not have been apparent in earlier phases due to the smaller sample size. Efficacy assessment in Phase 2 is equally critical and often involves predefined endpoints that reflect the treatment’s impact on the disease.
These endpoints can be clinical outcomes, such as tumor shrinkage in cancer patients or improvement in symptoms for chronic conditions like rheumatoid arthritis. Researchers may also utilize surrogate endpoints—biomarkers or other indicators that can predict clinical benefit—when direct measures are not feasible within the trial’s timeframe. For instance, in cardiovascular research, reductions in cholesterol levels may serve as a surrogate endpoint for long-term heart health outcomes.
The combination of safety and efficacy data collected during this phase lays the groundwork for informed decision-making regarding the drug’s future development.
Recruiting Participants for Phase 2 Trials
Recruiting participants for Phase 2 clinical trials poses unique challenges that require strategic planning and execution. Given that these trials involve individuals with specific medical conditions, identifying eligible candidates can be complex. Researchers often collaborate with healthcare providers, patient advocacy groups, and community organizations to raise awareness about the trial and its potential benefits.
Effective communication about the trial’s purpose, procedures, and potential risks is essential to build trust and encourage participation. Moreover, recruitment strategies may vary depending on the nature of the disease being studied. For instance, in rare diseases where patient populations are limited, researchers might employ targeted outreach efforts to connect with patients through specialized clinics or online platforms dedicated to those conditions.
In contrast, for more common diseases like diabetes or hypertension, broader recruitment strategies may be employed through advertisements in healthcare facilities or social media campaigns. Additionally, researchers must consider factors such as participant demographics, geographic location, and socioeconomic status to ensure a diverse representation that reflects the broader population affected by the disease.
Conducting Phase 2 Clinical Trials
| Metric | Description | Typical Range/Value | Importance |
|---|---|---|---|
| Number of Participants | Number of patients enrolled in the study | 100 – 300 | Ensures adequate power to detect treatment effects |
| Primary Endpoint | Main outcome measure to assess efficacy | Varies by study (e.g., tumor size reduction, symptom improvement) | Determines if the drug shows preliminary efficacy |
| Duration of Study | Length of time participants are followed | Several months to 2 years | Allows assessment of short-term efficacy and safety |
| Adverse Event Rate | Percentage of participants experiencing side effects | Varies; typically monitored closely | Evaluates safety profile of the intervention |
| Response Rate | Proportion of participants showing desired clinical response | Depends on condition and treatment | Indicates potential effectiveness of the drug |
| Randomization | Whether participants are randomly assigned to groups | Yes/No | Reduces bias and improves validity |
| Blinding | Whether participants and/or investigators are blinded | Single, Double, or None | Minimizes placebo effect and assessment bias |
| Dropout Rate | Percentage of participants who discontinue the study | Typically 5% – 20% | Impacts data integrity and study conclusions |
The execution of Phase 2 clinical trials requires meticulous planning and adherence to regulatory guidelines to ensure scientific integrity and participant safety. Once participants are recruited and informed consent is obtained, researchers initiate the trial by randomizing participants into treatment groups. This randomization process is crucial for minimizing bias and ensuring that any observed effects can be attributed to the treatment rather than confounding variables.
During the trial, researchers implement rigorous monitoring protocols to track participants’ health and adherence to the study regimen. Regular follow-up visits are scheduled to assess both safety and efficacy endpoints. Data collection methods may include clinical assessments, laboratory tests, imaging studies, and patient-reported outcomes through questionnaires or diaries.
The use of electronic data capture systems has become increasingly common in recent years, allowing for real-time data entry and monitoring while enhancing data accuracy and reducing administrative burdens.
Analyzing Data and Results
Once data collection is complete, researchers embark on a comprehensive analysis to evaluate the outcomes of the Phase 2 trial. Statistical methods are employed to determine whether the treatment demonstrates significant efficacy compared to the control group while also assessing safety profiles across different participant demographics. This analysis often involves complex statistical models that account for variables such as age, sex, comorbidities, and baseline disease severity.
The interpretation of results is critical; researchers must consider not only statistical significance but also clinical relevance. A treatment may show statistically significant improvements in certain endpoints but may not translate into meaningful benefits for patients’ quality of life or overall health outcomes. Furthermore, subgroup analyses can provide insights into how different populations respond to the treatment, guiding future research directions and potential personalized medicine approaches.
Reporting Findings and Publication
The dissemination of findings from Phase 2 clinical trials is an essential step in advancing medical knowledge and informing future research efforts. Researchers typically prepare detailed reports outlining their methodology, results, and interpretations for submission to peer-reviewed journals. This process involves rigorous scrutiny by experts in the field who evaluate the study’s design, data integrity, and conclusions drawn from the findings.
In addition to traditional journal publications, researchers may present their findings at scientific conferences or symposia where they can engage with other professionals in their field. These presentations provide opportunities for discussion and feedback that can refine future research directions or highlight areas needing further exploration. Moreover, sharing results with participants and stakeholders is crucial for transparency and fostering trust within the community.
Future Implications and Next Steps
The outcomes of Phase 2 clinical trials have significant implications for subsequent phases of drug development. If a treatment demonstrates promising efficacy and an acceptable safety profile, it may progress to Phase 3 trials where larger populations are studied under more diverse conditions. This transition is often accompanied by additional regulatory scrutiny as developers prepare for potential market approval.
Conversely, if results indicate limited efficacy or unacceptable safety concerns, researchers may need to reevaluate their approach or discontinue development altogether. The insights gained during Phase 2 can also inform modifications to dosing regimens or treatment protocols that enhance patient outcomes in future studies. Ultimately, the knowledge acquired during this phase not only shapes the trajectory of individual treatments but also contributes to broader advancements in medical science and therapeutic strategies across various fields.



