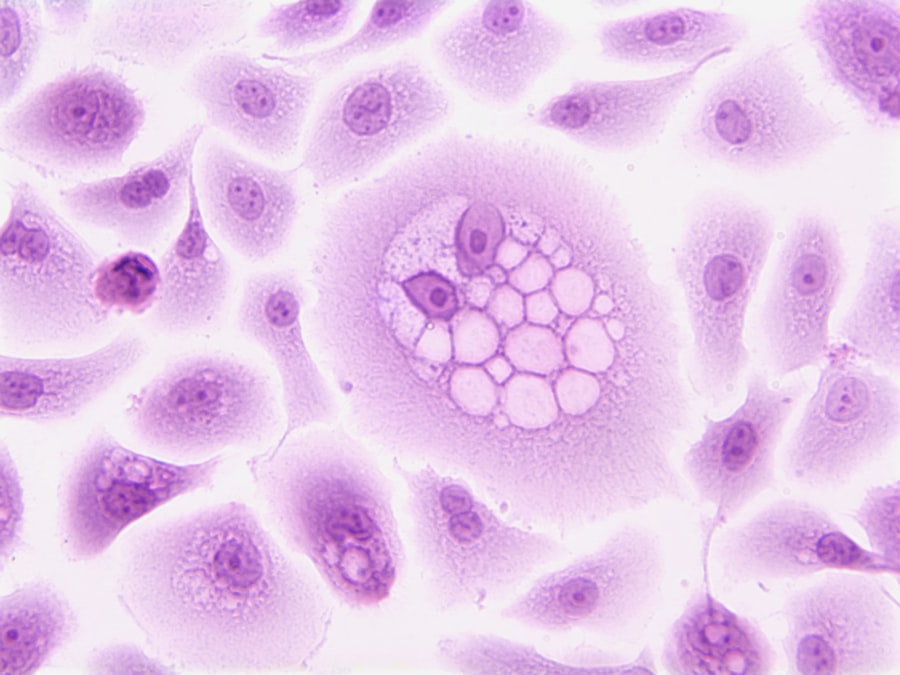
Cellular pathology is a medical science discipline that examines cells in disease states. The field involves analyzing cellular structures, functions, and modifications that result from pathological processes. Through this cellular-level investigation, researchers and clinicians gain essential knowledge for disease diagnosis, treatment development, and prevention strategies.
Cellular pathology draws from histology, biochemistry, and molecular biology to provide comprehensive evaluation of disease-related cellular changes. In clinical applications, cellular pathology serves as a fundamental diagnostic tool. Medical pathologists employ these techniques to identify cancers, infectious diseases, and autoimmune conditions.
Through microscopic examination of tissue specimens, pathologists detect abnormal cellular structures and functional changes that indicate specific diseases. These diagnostic findings directly inform treatment decisions and contribute to improved patient care outcomes.
Key Takeaways
- Cellular pathology is essential for understanding disease mechanisms at the cellular level.
- Genetic and environmental factors both significantly influence cellular health and dysfunction.
- Disruptions in cellular communication and signaling contribute to disease progression, including cancer.
- Advances in research are leading to novel therapeutic strategies targeting cellular pathologies.
- Ongoing studies promise to enhance diagnosis, treatment, and prevention of diseases through cellular pathology insights.
Understanding Cellular Dysfunction and Disease
Cellular dysfunction is a fundamental aspect of many diseases, characterized by the failure of cells to perform their normal functions. This dysfunction can arise from various factors, including genetic mutations, environmental stressors, and metabolic imbalances. For instance, in neurodegenerative diseases such as Alzheimer’s, cellular dysfunction manifests as the accumulation of misfolded proteins that disrupt normal cellular processes.
These disruptions lead to neuronal death and cognitive decline, illustrating how cellular health is intricately linked to overall well-being. Moreover, cellular dysfunction can also result from inflammatory responses triggered by infections or injuries. In conditions like rheumatoid arthritis, immune cells become hyperactive and attack healthy tissues, leading to chronic inflammation and joint damage.
Understanding the mechanisms behind cellular dysfunction is crucial for developing targeted therapies that can restore normal cell function or mitigate the effects of disease. By investigating the pathways involved in cellular dysfunction, researchers can identify potential biomarkers for early diagnosis and therapeutic targets for intervention.
Investigating the Role of Genetics in Cellular Pathology
Genetics plays a pivotal role in cellular pathology, influencing both susceptibility to diseases and the progression of various conditions. Genetic mutations can lead to alterations in cellular functions that predispose individuals to specific diseases. For example, mutations in the BRCA1 and BRCA2 genes significantly increase the risk of breast and ovarian cancers by impairing the body’s ability to repair DNA damage.
This highlights how genetic factors can create a cellular environment conducive to disease development. Furthermore, epigenetic modifications—changes in gene expression that do not involve alterations to the underlying DNA sequence—also contribute to cellular pathology. These modifications can be influenced by environmental factors and lifestyle choices, leading to changes in cellular behavior that may promote disease.
For instance, exposure to certain chemicals can result in epigenetic changes that activate oncogenes or silence tumor suppressor genes, thereby facilitating cancer progression. Understanding the interplay between genetics and cellular pathology is essential for developing personalized medicine approaches that consider an individual’s genetic makeup when designing treatment plans.
Exploring the Impact of Environmental Factors on Cellular Health
Environmental factors significantly influence cellular health and can contribute to the onset of various diseases. These factors include exposure to pollutants, dietary habits, physical activity levels, and lifestyle choices such as smoking and alcohol consumption. For instance, air pollution has been linked to respiratory diseases and cardiovascular conditions due to its detrimental effects on lung cells and vascular function.
Fine particulate matter can induce oxidative stress and inflammation at the cellular level, leading to chronic health issues. Additionally, nutrition plays a critical role in maintaining cellular health. A diet rich in antioxidants can help protect cells from oxidative damage caused by free radicals, while deficiencies in essential nutrients can impair cellular functions.
For example, a lack of vitamin D has been associated with increased susceptibility to autoimmune diseases and certain cancers. By understanding how environmental factors impact cellular health, researchers can develop strategies aimed at mitigating these risks through lifestyle modifications or public health initiatives.
Unraveling the Complexities of Cellular Communication and Signaling
| Term | Definition | Common Techniques | Applications |
|---|---|---|---|
| Histology | Study of the microscopic structure of tissues and cells | Light microscopy, staining (H&E, immunohistochemistry) | Diagnosing diseases, research on tissue structure |
| Cytology | Study of individual cells and their structure | Cell smears, Pap test, flow cytometry | Cancer screening, cell counting, disease diagnosis |
| Cell Biology | Study of cell function, structure, and life cycle | Fluorescence microscopy, cell culture, molecular assays | Understanding cell processes, drug development |
| Pathology | Study of disease-related changes in cells and tissues | Biopsy analysis, histopathology, molecular pathology | Disease diagnosis, prognosis, treatment planning |
| Flow Cytometry | Technique to analyze physical and chemical characteristics of cells | Laser-based cell counting, immunophenotyping | Immunology, cancer diagnosis, cell sorting |
Cellular communication is a fundamental aspect of maintaining homeostasis within the body. Cells communicate through intricate signaling pathways that regulate various physiological processes, including growth, differentiation, and immune responses. Disruptions in these signaling pathways can lead to pathological conditions.
For instance, aberrant signaling in the insulin pathway is a hallmark of diabetes mellitus, where insulin resistance leads to elevated blood glucose levels and subsequent complications. Moreover, intercellular communication is essential for coordinating responses to environmental changes or stressors. Cells utilize various signaling molecules such as hormones, neurotransmitters, and cytokines to relay information.
In cancer biology, tumor cells often hijack these signaling pathways to promote uncontrolled growth and evade apoptosis (programmed cell death). Understanding these complex communication networks is crucial for identifying potential therapeutic targets that can restore normal signaling and inhibit disease progression.
Examining the Role of Cellular Pathology in Cancer Development
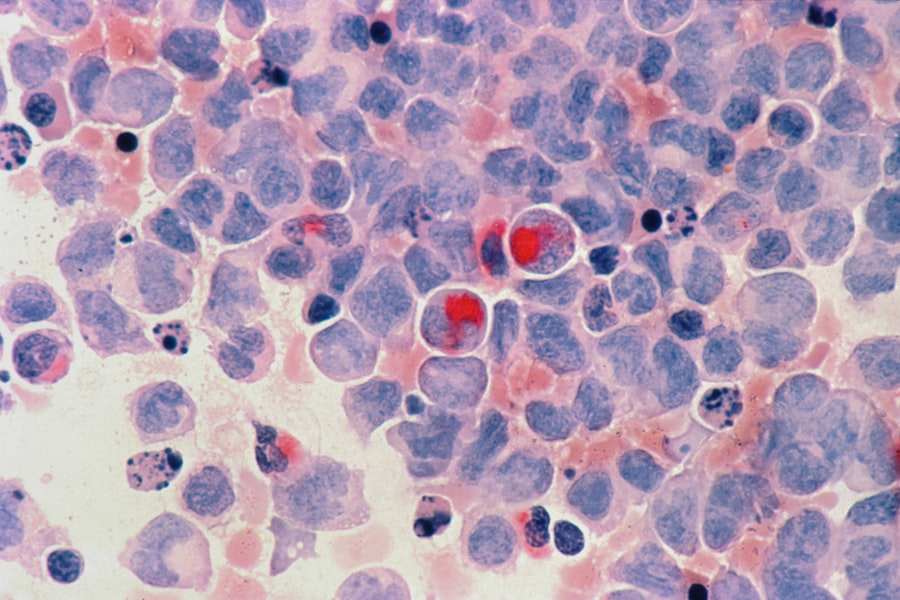
Cancer development is a prime example of how cellular pathology manifests through uncontrolled cell proliferation and evasion of normal regulatory mechanisms. The transformation of normal cells into cancerous ones involves a series of genetic mutations that disrupt key pathways governing cell cycle regulation, apoptosis, and DNA repair mechanisms. For instance, mutations in oncogenes such as RAS or tumor suppressor genes like TP53 are frequently observed in various cancers and play critical roles in tumorigenesis.
The tumor microenvironment also significantly influences cancer progression. Interactions between cancer cells and surrounding stromal cells can promote tumor growth and metastasis through altered signaling pathways and immune evasion strategies. For example, cancer-associated fibroblasts can secrete growth factors that enhance tumor cell proliferation while simultaneously suppressing anti-tumor immune responses.
Understanding these interactions at the cellular level is essential for developing effective cancer therapies that target not only the tumor cells but also their microenvironment.
Investigating Novel Therapeutic Approaches for Cellular Pathologies
The field of cellular pathology is continuously evolving with advancements in therapeutic approaches aimed at addressing various diseases at their root causes. One promising area of research involves gene therapy, which seeks to correct genetic defects by delivering functional genes into affected cells. This approach has shown potential in treating inherited disorders such as cystic fibrosis and certain types of muscular dystrophy by restoring normal cellular function.
Another innovative strategy involves the use of targeted therapies that specifically inhibit aberrant signaling pathways associated with diseases like cancer. For instance, tyrosine kinase inhibitors have revolutionized the treatment of chronic myeloid leukemia (CML) by selectively targeting the BCR-ABL fusion protein responsible for uncontrolled cell proliferation in this condition. Additionally, immunotherapy has emerged as a powerful tool in cancer treatment by harnessing the body’s immune system to recognize and destroy cancer cells more effectively.
Research into regenerative medicine also holds promise for addressing cellular pathologies by promoting tissue repair and regeneration. Stem cell therapy aims to replace damaged or dysfunctional cells with healthy ones derived from pluripotent stem cells or adult stem cells. This approach has potential applications in treating degenerative diseases such as Parkinson’s disease or spinal cord injuries by restoring lost cellular functions.
The Future of Cellular Pathology Research
The future of cellular pathology research is poised for significant advancements as our understanding of cellular mechanisms continues to deepen. With the advent of technologies such as CRISPR-Cas9 gene editing and high-throughput sequencing, researchers are now able to explore genetic variations and their implications for disease at an unprecedented scale. These tools enable scientists to dissect complex biological systems and identify novel therapeutic targets with greater precision.
Moreover, interdisciplinary collaborations between biologists, clinicians, bioinformaticians, and engineers are fostering innovative approaches to tackle challenges in cellular pathology. The integration of artificial intelligence and machine learning into pathology diagnostics holds promise for enhancing accuracy and efficiency in disease detection. As we continue to unravel the complexities of cellular behavior in health and disease, the potential for developing effective interventions will expand, ultimately leading to improved patient care and outcomes across a wide range of conditions.