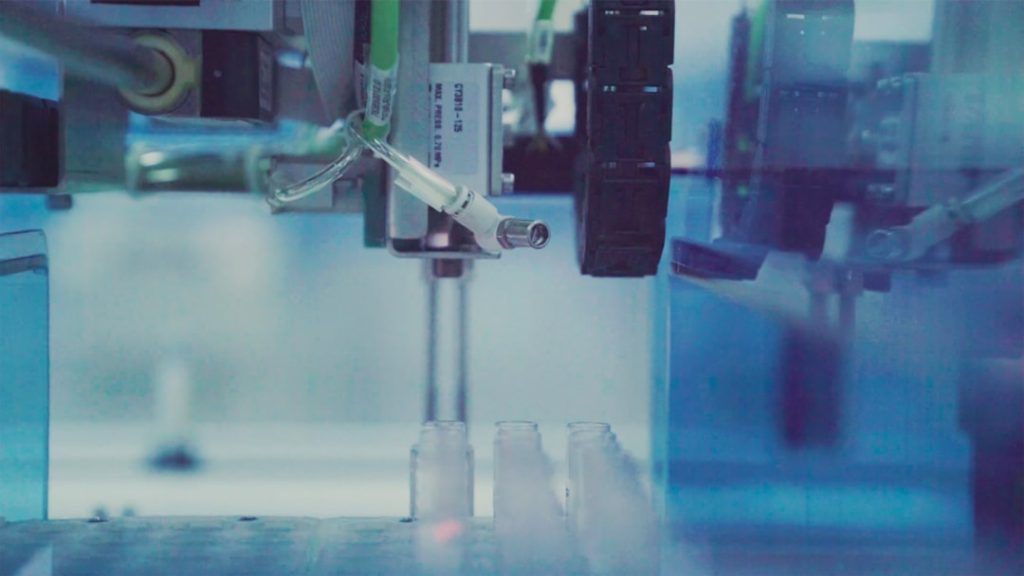
Preclinical research serves as the foundational bedrock upon which clinical trials are built. This phase of research is critical for understanding the biological mechanisms of diseases and the potential therapeutic effects of new drugs or interventions. It typically involves laboratory studies and animal testing, which provide essential data on pharmacodynamics, pharmacokinetics, and toxicology.
By investigating how a drug interacts with biological systems before it is tested in humans, researchers can identify promising candidates that warrant further exploration in clinical settings. For instance, the development of monoclonal antibodies for cancer treatment began with extensive preclinical studies that elucidated their mechanisms of action and safety profiles, ultimately leading to successful clinical applications. Moreover, preclinical research allows for the refinement of hypotheses and the optimization of treatment protocols.
Researchers can explore various dosing regimens, delivery methods, and combinations with other therapies to determine the most effective strategies for human application. This iterative process not only enhances the likelihood of success in clinical trials but also minimizes the risk of failure by identifying potential issues early on. For example, the preclinical evaluation of CAR-T cell therapy involved rigorous testing in animal models to assess its efficacy against specific types of cancer, paving the way for its eventual approval and use in patients with refractory malignancies.
Key Takeaways
- Preclinical research is crucial for establishing the safety and efficacy of new treatments before human trials.
- Successfully translating preclinical findings to clinical trials requires careful validation and adaptation.
- Ethical considerations and informed consent are fundamental to protecting patient rights in clinical research.
- Regulatory agencies play a key role in overseeing the development and approval of new medical treatments.
- Integrating preclinical and clinical research advances the future of treatment development through improved collaboration and innovation.
Translating Preclinical Findings to Clinical Trials
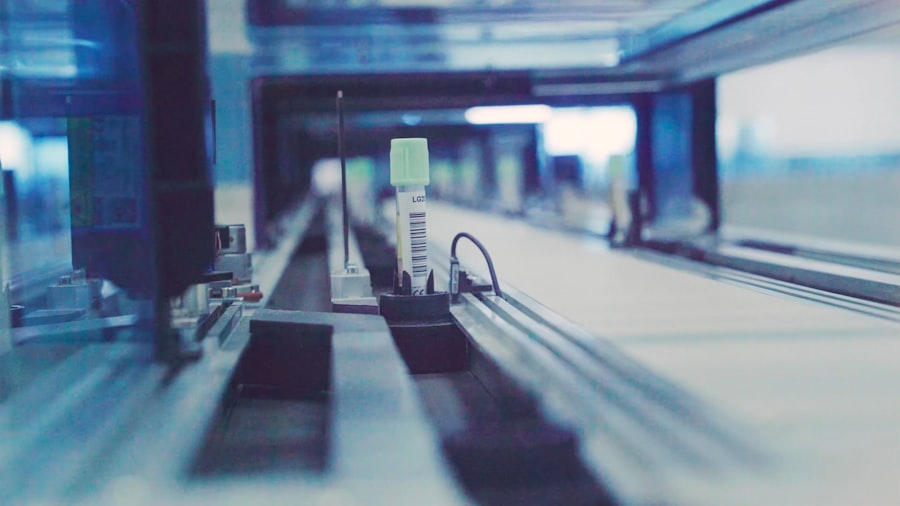
The transition from preclinical findings to clinical trials is a complex process that requires careful consideration and planning. One of the primary goals during this phase is to ensure that the insights gained from laboratory and animal studies are effectively translated into human applications. This involves not only confirming the safety and efficacy of a treatment but also understanding how it behaves in the human body, which can differ significantly from animal models.
For instance, while a drug may show promise in mice, its pharmacokinetics and metabolism could vary dramatically in humans, necessitating adjustments to dosing and administration routes. To facilitate this translation, researchers often employ a variety of methodologies, including biomarker identification and patient stratification. Biomarkers can provide valuable insights into how a drug works and who might benefit most from it.
For example, the identification of specific genetic mutations in tumors has allowed for targeted therapies that are tailored to individual patients, significantly improving outcomes. Additionally, adaptive trial designs are increasingly being utilized to allow for modifications based on interim results, thereby enhancing the efficiency of clinical trials and ensuring that only the most promising treatments proceed to later stages.
Challenges in Transitioning from Preclinical to Clinical
Despite the critical role of preclinical research in informing clinical trials, several challenges persist in the transition from bench to bedside. One significant hurdle is the inherent variability between animal models and human physiology. While animal studies provide valuable insights, they cannot fully replicate the complexity of human diseases or the multifaceted interactions within human biology.
This discrepancy can lead to unexpected outcomes in clinical trials, where a treatment that appeared effective in preclinical studies fails to demonstrate similar efficacy in humans. Another challenge lies in the regulatory landscape governing clinical trials. Regulatory agencies require extensive documentation and evidence of safety and efficacy before allowing a treatment to enter human testing.
This process can be time-consuming and resource-intensive, often leading to delays in bringing new therapies to market. Furthermore, researchers must navigate ethical considerations related to patient safety and informed consent, which can complicate trial design and implementation. The need for rigorous oversight is essential to protect participants but can also create barriers that slow down the pace of innovation.
Ethical Considerations in Clinical Research
| Ethical Consideration | Description | Key Metrics | Importance |
|---|---|---|---|
| Informed Consent | Ensuring participants understand the study and voluntarily agree to participate. | Percentage of participants providing documented consent, comprehension assessment scores | High |
| Risk-Benefit Analysis | Evaluating potential risks against anticipated benefits to participants. | Number of adverse events, severity of side effects, benefit-to-risk ratio | High |
| Confidentiality | Protecting participant data and privacy throughout the study. | Number of data breaches, compliance with data protection regulations | High |
| Equitable Selection | Ensuring fair participant recruitment without discrimination or exploitation. | Diversity metrics (age, gender, ethnicity), recruitment bias indicators | Medium |
| Independent Review | Study protocols reviewed by ethics committees or institutional review boards (IRBs). | Number of protocol approvals, time to approval, number of protocol modifications requested | High |
| Transparency | Open communication of study goals, funding sources, and results. | Publication rate, disclosure of conflicts of interest, trial registration status | Medium |
| Participant Welfare | Monitoring and ensuring the health and safety of participants during the trial. | Frequency of health monitoring, participant dropout rates due to adverse effects | High |
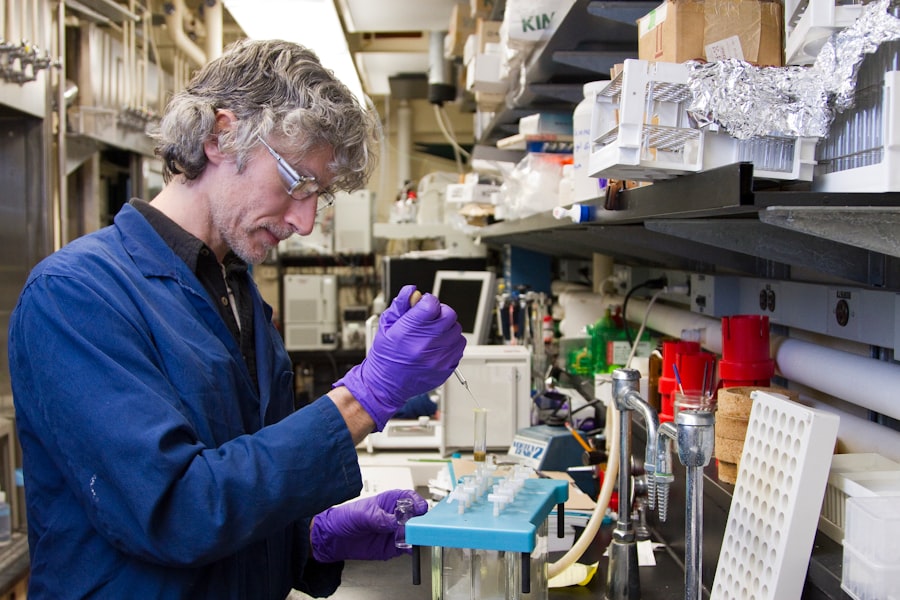
Ethical considerations are paramount in clinical research, particularly when transitioning from preclinical studies to human trials. The principle of “do no harm” is central to medical ethics, guiding researchers to prioritize patient safety above all else. Informed consent is a critical component of this ethical framework, ensuring that participants are fully aware of the potential risks and benefits associated with their involvement in a trial.
Researchers must communicate complex information clearly and transparently, allowing individuals to make informed decisions about their participation. Additionally, ethical considerations extend beyond informed consent to encompass issues such as equity in patient recruitment and the fair distribution of benefits and burdens associated with research participation. Vulnerable populations must be protected from exploitation, and efforts should be made to ensure that diverse groups are represented in clinical trials.
This inclusivity not only enhances the generalizability of findings but also addresses historical disparities in healthcare access and treatment outcomes. For example, initiatives aimed at increasing minority participation in clinical trials have been implemented to ensure that new therapies are effective across diverse populations.
The Role of Regulatory Agencies in Advancing New Treatments
Regulatory agencies play a crucial role in overseeing the development and approval of new treatments, ensuring that they meet rigorous standards for safety and efficacy before reaching patients. In the United States, the Food and Drug Administration (FDA) is responsible for evaluating clinical trial data and making determinations about whether a treatment can be marketed. This process involves a thorough review of preclinical data, clinical trial results, manufacturing practices, and labeling information.
The regulatory framework is designed not only to protect patients but also to foster innovation within the pharmaceutical industry. Agencies often provide guidance on trial design and regulatory pathways that can expedite the development process for promising therapies. For instance, programs such as Fast Track designation or Breakthrough Therapy designation allow for more frequent interactions with regulatory officials and can significantly shorten the time it takes for a treatment to reach the market.
These initiatives reflect an understanding of the urgent need for new therapies in areas with high unmet medical needs, such as rare diseases or aggressive cancers.
Patient Recruitment and Informed Consent in Clinical Trials
Effective patient recruitment is a cornerstone of successful clinical trials, yet it remains one of the most challenging aspects of research design. Identifying eligible participants who meet specific inclusion criteria while also ensuring diversity can be difficult. Researchers must employ innovative strategies to reach potential participants, including community outreach programs, partnerships with healthcare providers, and digital marketing campaigns.
Engaging with patient advocacy groups can also enhance recruitment efforts by raising awareness about ongoing trials and their importance. Informed consent is intricately linked to patient recruitment; it is essential that participants understand what their involvement entails. This process goes beyond simply obtaining a signature on a consent form; it requires ongoing communication throughout the trial.
Researchers must ensure that participants are aware of their rights, including the right to withdraw from the study at any time without penalty. Providing information in accessible language and formats is crucial for fostering trust and transparency between researchers and participants.
Monitoring and Reporting Adverse Events in Clinical Trials
Monitoring adverse events during clinical trials is critical for ensuring participant safety and maintaining the integrity of research findings. Adverse events can range from mild side effects to severe complications that may jeopardize patient health or even lead to death. Regulatory agencies require that all adverse events be reported promptly and accurately, allowing for real-time assessment of a treatment’s safety profile.
Data Safety Monitoring Boards (DSMBs) are often established to oversee ongoing trials and evaluate safety data independently. These boards play a vital role in determining whether a trial should continue as planned or if modifications are necessary based on emerging safety concerns. For example, if a significant number of participants experience serious adverse events related to a treatment, a DSMB may recommend halting the trial until further investigation can be conducted.
This oversight mechanism is essential for protecting participants while also ensuring that valuable data is collected responsibly.
The Future of Advancing New Treatments: Integrating Preclinical and Clinical Research
The future of advancing new treatments lies in a more integrated approach between preclinical and clinical research phases. As scientific understanding evolves, there is an increasing recognition that collaboration across disciplines can enhance the efficiency and effectiveness of drug development processes. For instance, leveraging advancements in genomics and personalized medicine allows researchers to tailor treatments based on individual patient profiles rather than relying solely on traditional one-size-fits-all approaches.
Moreover, innovative technologies such as artificial intelligence (AI) and machine learning are beginning to play a significant role in both preclinical and clinical research. These tools can analyze vast datasets to identify potential drug candidates more rapidly or predict patient responses based on genetic information. By integrating these technologies into research workflows, scientists can streamline processes from discovery through clinical application, ultimately accelerating the delivery of new therapies to patients who need them most.
In conclusion, as we look toward the future of medical research, fostering collaboration between preclinical scientists and clinical researchers will be essential for overcoming existing challenges and enhancing patient outcomes. By embracing an integrated approach that prioritizes ethical considerations, regulatory compliance, and innovative methodologies, we can pave the way for groundbreaking advancements in healthcare that improve lives around the world.