Frontage clinical trials play a pivotal role in the landscape of medical research, serving as a bridge between laboratory discoveries and real-world applications. These trials are essential for validating the safety and efficacy of new treatments, ensuring that they meet rigorous scientific standards before reaching the market. The significance of these trials cannot be overstated; they provide the necessary data that informs regulatory decisions, shapes clinical guidelines, and ultimately influences patient care.
By systematically evaluating new therapies, Frontage clinical trials contribute to a deeper understanding of diseases and the development of innovative treatment strategies. Moreover, Frontage clinical trials are instrumental in fostering collaboration among various stakeholders in the healthcare ecosystem. Researchers, pharmaceutical companies, regulatory bodies, and healthcare providers all play a role in the clinical trial process.
This collaborative environment not only accelerates the pace of medical advancements but also enhances the quality of research outcomes. The data generated from these trials can lead to breakthroughs in treatment protocols, offering hope to patients with conditions that previously had limited therapeutic options. As such, Frontage clinical trials are not merely a procedural step in drug development; they are a cornerstone of modern medicine that drives progress and innovation.
Key Takeaways
- Frontage clinical trials play a crucial role in advancing medical research and drug development.
- They ensure the safety and efficacy of new treatments through rigorous testing processes.
- Conducting these trials involves a structured process that prioritizes patient care and ethical standards.
- Participation in Frontage clinical trials can directly impact patient outcomes and contribute to medical innovation.
- The future of Frontage clinical trials holds significant potential for breakthroughs in healthcare and treatment options.
The Role of Frontage Clinical Trials in Drug Development
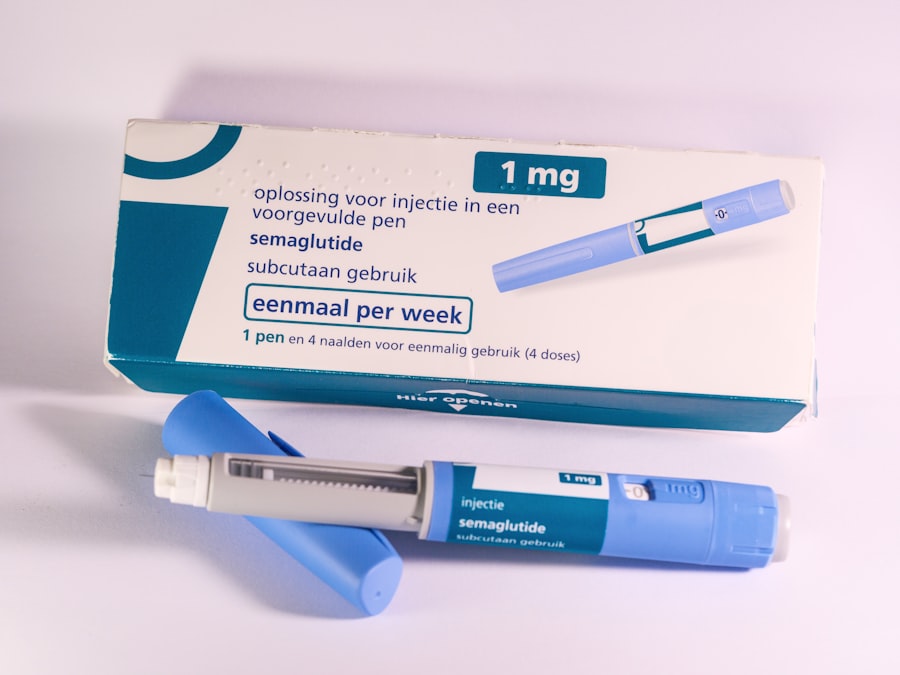
In the realm of drug development, Frontage clinical trials serve as a critical phase that determines whether a new therapeutic agent can transition from concept to reality. These trials are typically conducted in multiple phases, each designed to answer specific research questions regarding the drug’s pharmacokinetics, pharmacodynamics, and overall therapeutic potential. Phase I trials primarily focus on assessing safety and tolerability in a small group of healthy volunteers or patients, while Phase II trials expand the participant pool to evaluate efficacy and optimal dosing.
Phase III trials further validate these findings on a larger scale, often involving diverse populations to ensure that results are generalizable. The structured approach of Frontage clinical trials allows for meticulous data collection and analysis, which is essential for regulatory approval. Regulatory agencies such as the U.S.
Food and Drug Administration (FDA) rely heavily on the outcomes of these trials to make informed decisions about whether a drug should be approved for public use. The rigorous nature of these studies ensures that only those treatments that demonstrate significant benefits over existing options are brought to market. This not only protects patients but also fosters trust in the healthcare system, as patients can be assured that new therapies have undergone thorough evaluation before being prescribed.
How Frontage Clinical Trials Ensure Safety and Efficacy of New Treatments
Safety and efficacy are paramount considerations in the development of any new treatment, and Frontage clinical trials are designed specifically to address these concerns. Through a series of carefully controlled studies, researchers can identify potential side effects and adverse reactions associated with a new drug. For instance, during Phase I trials, participants are closely monitored for any unexpected reactions, allowing researchers to gather crucial data on how the drug interacts with the human body.
This initial phase is critical for establishing a safety profile that informs subsequent phases of testing. Efficacy is assessed through well-defined endpoints that measure how well a treatment works compared to existing therapies or placebos. In Phase II and III trials, researchers employ various methodologies, including randomized controlled trials (RCTs), to minimize bias and ensure that results are reliable.
For example, if a new cancer treatment is being tested, researchers might compare its effectiveness against standard chemotherapy regimens in a randomized manner. This rigorous evaluation process not only helps in determining whether a treatment is effective but also provides insights into which patient populations may benefit most from it. By ensuring both safety and efficacy through Frontage clinical trials, researchers can confidently advance new therapies into clinical practice.
The Process of Conducting Frontage Clinical Trials
Conducting Frontage clinical trials involves a complex series of steps that require meticulous planning and execution. The process begins with the design of the trial protocol, which outlines the study’s objectives, methodology, participant criteria, and statistical analysis plan. This protocol must be approved by an Institutional Review Board (IRB) to ensure that ethical standards are upheld and that participants’ rights are protected throughout the study.
Once the protocol is approved, researchers begin recruiting participants who meet specific inclusion and exclusion criteria. This recruitment process is crucial for ensuring that the trial population accurately reflects the demographics of the broader patient population that will ultimately use the treatment. After enrollment, participants undergo baseline assessments before being assigned to treatment groups.
Throughout the trial, data is collected at various intervals to monitor safety and efficacy outcomes. This data is then analyzed using sophisticated statistical methods to draw meaningful conclusions about the treatment’s performance.
The Impact of Frontage Clinical Trials on Patient Care and Outcomes
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of Trials | Total clinical trials conducted by Frontage | 150 | Trials |
| Therapeutic Areas | Number of therapeutic areas covered | 10 | Areas |
| Patient Enrollment | Total patients enrolled across all trials | 12,000 | Patients |
| Trial Phases | Distribution of trials by phase | Phase I: 30%, Phase II: 40%, Phase III: 30% | Percentage |
| Average Trial Duration | Average length of clinical trials | 18 | Months |
| Geographic Reach | Number of countries where trials are conducted | 15 | Countries |
| Success Rate | Percentage of trials meeting primary endpoints | 75 | Percentage |
The impact of Frontage clinical trials on patient care is profound and multifaceted. By rigorously testing new treatments before they become widely available, these trials ensure that patients receive therapies that have been proven to be safe and effective. This not only enhances patient outcomes but also contributes to more personalized medicine approaches, where treatments can be tailored to individual patient needs based on trial findings.
Furthermore, participation in Frontage clinical trials often provides patients with access to cutting-edge therapies that may not yet be available through standard care pathways. For instance, patients with rare diseases or those who have exhausted all conventional treatment options may find hope through participation in clinical trials testing novel therapies. This access can lead to improved quality of life and even survival benefits for patients who might otherwise have limited options.
Additionally, the data generated from these trials can inform future treatment guidelines and best practices, ultimately benefiting a larger patient population.
The Ethical Considerations of Frontage Clinical Trials
Ethical considerations are paramount in the conduct of Frontage clinical trials, as they involve human subjects who may be vulnerable or facing serious health challenges. Informed consent is a cornerstone of ethical research practices; participants must be fully aware of the potential risks and benefits associated with their involvement in a trial. This process ensures that individuals make educated decisions about their participation without coercion or undue influence.
Moreover, ethical oversight is provided by Institutional Review Boards (IRBs) or Ethics Committees (ECs), which review trial protocols to ensure that they adhere to ethical standards and protect participants’ rights. These bodies assess factors such as risk minimization, equitable selection of participants, and provisions for monitoring adverse events throughout the trial duration. The ethical framework surrounding Frontage clinical trials is designed to uphold the dignity and welfare of participants while advancing scientific knowledge.
The Future of Frontage Clinical Trials and Their Potential Contributions to Medical Innovation
The future of Frontage clinical trials is poised for transformation as advancements in technology and data analytics continue to reshape the landscape of medical research. Innovations such as artificial intelligence (AI) and machine learning are being integrated into trial design and execution, enabling researchers to identify suitable candidates more efficiently and analyze vast amounts of data with unprecedented speed. These technologies can enhance patient recruitment strategies by identifying individuals who meet specific criteria based on electronic health records or genetic profiles.
Additionally, decentralized clinical trials are gaining traction as a means to increase accessibility and participation rates among diverse populations. By leveraging telemedicine and remote monitoring technologies, researchers can conduct trials that allow participants to engage from their homes rather than requiring them to travel to clinical sites. This approach not only reduces barriers to participation but also enhances patient retention throughout the trial process.
As these innovations continue to evolve, Frontage clinical trials will likely become more efficient, inclusive, and capable of addressing complex medical challenges.
How to Participate in Frontage Clinical Trials and Contribute to Advancing Medical Research
Participating in Frontage clinical trials offers individuals an opportunity to contribute significantly to medical research while potentially gaining access to novel treatments. Those interested in participating should first consult with their healthcare providers to discuss eligibility based on their medical history and current health status. Healthcare professionals can provide valuable insights into ongoing clinical trials relevant to specific conditions or diseases.
Individuals can also explore various online registries and databases that list active clinical trials by condition or location. Websites such as ClinicalTrials.gov provide comprehensive information about ongoing studies, including eligibility criteria, study locations, and contact information for research teams. By expressing interest in participation, individuals can engage with researchers who will guide them through the informed consent process and answer any questions they may have about what participation entails.
In conclusion, Frontage clinical trials represent a vital component of medical research that drives innovation while ensuring patient safety and efficacy in new treatments. Through rigorous methodologies and ethical oversight, these trials contribute significantly to advancing healthcare outcomes for patients worldwide.