Global clinical trials are pivotal in the advancement of medical science and the development of new therapies. They serve as a critical mechanism for evaluating the safety and efficacy of new drugs, devices, and treatment protocols across diverse populations. By conducting trials on an international scale, researchers can gather data that reflects a wide array of genetic backgrounds, environmental factors, and lifestyle variations.
This diversity is essential for understanding how different populations respond to treatments, which can lead to more personalized and effective healthcare solutions. Moreover, global clinical trials facilitate faster recruitment of participants, which can significantly shorten the timeline for bringing new therapies to market. In many cases, the prevalence of certain diseases varies by region; thus, conducting trials in multiple countries allows for a more efficient accumulation of data.
For instance, a drug targeting a specific type of cancer may find a larger pool of eligible participants in regions where that cancer is more prevalent. This not only accelerates the research process but also enhances the statistical power of the findings, leading to more robust conclusions about the treatment’s effectiveness.
Key Takeaways
- Global clinical trials are essential for diverse and comprehensive medical research outcomes.
- Conducting trials worldwide offers benefits like varied patient populations but faces logistical and regulatory challenges.
- Regulatory bodies play a crucial role in ensuring safety, compliance, and ethical standards across countries.
- Ethical considerations, including informed consent and equitable treatment, are vital in global trial conduct.
- Collaborations, technological innovations, and future strategies are shaping the evolution and impact of global clinical trials.
Advantages and Challenges of Conducting Clinical Trials Worldwide
Conducting clinical trials on a global scale presents numerous advantages, including access to a broader patient population and the ability to study diseases that may be endemic to specific regions. This geographical diversity can yield insights that are not possible in localized studies. For example, trials conducted in tropical regions may uncover unique responses to treatments for diseases like malaria or dengue fever, which are less common in temperate climates.
Additionally, global trials can help pharmaceutical companies tap into emerging markets, potentially leading to increased revenue streams and greater global health impact. However, these advantages come with significant challenges. One major hurdle is navigating the complex regulatory landscape that varies from country to country.
Each nation has its own set of laws and guidelines governing clinical research, which can complicate study design and implementation. Furthermore, cultural differences can influence patient recruitment and retention. In some cultures, there may be skepticism about medical research or a lack of understanding regarding informed consent, which can hinder participation rates.
Addressing these challenges requires careful planning and a deep understanding of local contexts.
The Role of Regulatory Bodies in Global Clinical Trials
Regulatory bodies play a crucial role in overseeing global clinical trials to ensure that they are conducted ethically and safely. Organizations such as the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the World Health Organization (WHO) establish guidelines that govern the conduct of clinical research.
These regulations are designed to protect participants from harm and ensure that the data collected is reliable and valid. For instance, regulatory agencies require that trials adhere to Good Clinical Practice (GCP) standards, which outline the responsibilities of sponsors, investigators, and ethics committees. In addition to ensuring compliance with ethical standards, regulatory bodies also facilitate international collaboration by harmonizing guidelines across borders.
Initiatives such as the International Council for Harmonisation (ICH) aim to streamline the regulatory process for clinical trials conducted in multiple countries. By promoting consistency in data requirements and trial protocols, these organizations help reduce duplication of effort and expedite the approval process for new therapies. However, despite these efforts, discrepancies still exist between regulatory frameworks, which can create obstacles for researchers seeking to conduct multinational studies.
Ethical Considerations in Global Clinical Trials
Ethical considerations are paramount in the design and execution of global clinical trials. Researchers must navigate complex moral landscapes that vary by culture and legal framework. Informed consent is a fundamental ethical principle that requires participants to fully understand the nature of the trial, its potential risks and benefits, and their right to withdraw at any time without penalty.
However, achieving true informed consent can be challenging in regions where literacy rates are low or where there is a lack of trust in medical institutions. Additionally, researchers must be vigilant about the potential for exploitation in vulnerable populations. There is a risk that individuals from low-income countries may be enrolled in trials without adequate understanding or compensation for their participation.
This raises questions about equity and justice in research practices. Ethical review boards play a critical role in assessing trial protocols to ensure that they prioritize participant welfare and adhere to ethical standards. The establishment of community advisory boards can also help bridge cultural gaps and ensure that local perspectives are considered in trial design.
The Impact of Global Clinical Trials on Healthcare Access and Equity
| Region | Number of Clinical Trials | Percentage of Global Trials | Top Therapeutic Areas | Average Trial Duration (months) |
|---|---|---|---|---|
| North America | 12,500 | 35% | Oncology, Cardiovascular, Neurology | 24 |
| Europe | 9,000 | 25% | Oncology, Infectious Diseases, Immunology | 22 |
| Asia-Pacific | 8,000 | 22% | Infectious Diseases, Oncology, Metabolic Disorders | 20 |
| Latin America | 3,000 | 8% | Infectious Diseases, Cardiovascular, Respiratory | 18 |
| Africa | 1,500 | 4% | Infectious Diseases, Malaria, HIV/AIDS | 16 |
| Middle East | 1,000 | 3% | Oncology, Diabetes, Cardiovascular | 19 |
Global clinical trials have significant implications for healthcare access and equity. By testing new treatments in diverse populations, these trials can lead to breakthroughs that improve health outcomes for underrepresented groups. For example, research on cardiovascular diseases conducted in various ethnic populations has revealed differences in drug metabolism and efficacy, leading to more tailored treatment options that consider genetic diversity.
This can ultimately enhance healthcare access for populations that have historically been marginalized in clinical research. However, disparities still exist in how benefits from global clinical trials are distributed. Often, successful treatments developed through these trials may not be accessible to participants or communities involved in the research due to high costs or lack of healthcare infrastructure.
This raises ethical concerns about whether those who contribute to scientific advancements are adequately compensated or supported when new therapies become available. Addressing these inequities requires a concerted effort from researchers, policymakers, and healthcare providers to ensure that advancements in medicine translate into tangible benefits for all populations.
Collaborations and Partnerships in Global Clinical Trials

Collaborations between various stakeholders are essential for the success of global clinical trials. Partnerships between pharmaceutical companies, academic institutions, government agencies, and non-profit organizations can enhance resource sharing and expertise. For instance, collaborations with local universities can provide valuable insights into cultural nuances that affect patient recruitment and retention strategies.
Additionally, partnerships with non-governmental organizations (NGOs) can facilitate outreach efforts to engage communities that may be hesitant to participate in clinical research. Moreover, public-private partnerships have emerged as a powerful model for advancing global health initiatives through clinical trials. These collaborations can leverage funding from both sectors to support research efforts aimed at addressing pressing health challenges in low- and middle-income countries.
An example is the collaboration between the Bill & Melinda Gates Foundation and pharmaceutical companies to develop vaccines for diseases like malaria and tuberculosis. Such partnerships not only enhance research capabilities but also foster innovation by combining diverse expertise and resources.
Emerging Trends and Innovations in Global Clinical Trials
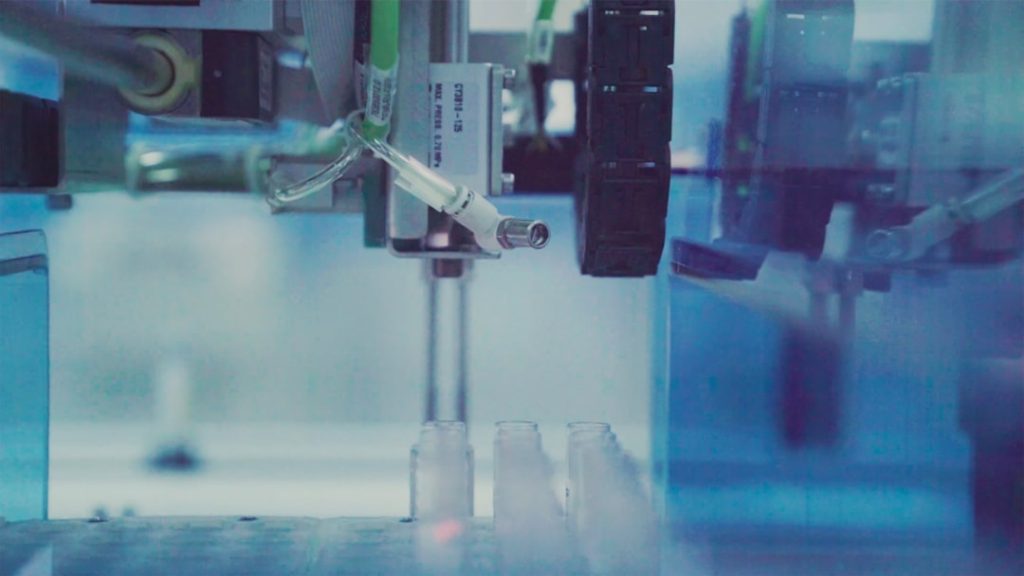
The landscape of global clinical trials is evolving rapidly due to technological advancements and innovative methodologies. One notable trend is the increasing use of digital health technologies, such as telemedicine and mobile health applications, which facilitate remote patient monitoring and data collection. These tools can enhance participant engagement by allowing individuals to participate from their homes while providing researchers with real-time data on treatment outcomes.
This shift towards decentralized clinical trials has been accelerated by the COVID-19 pandemic, which highlighted the need for flexible approaches to conducting research. Another emerging trend is the integration of artificial intelligence (AI) and machine learning into trial design and analysis. These technologies can streamline patient recruitment by identifying eligible participants more efficiently through electronic health records and other data sources.
Additionally, AI can assist in analyzing complex datasets generated during trials, enabling researchers to uncover patterns that may not be immediately apparent through traditional statistical methods. As these innovations continue to develop, they hold the potential to transform how global clinical trials are conducted.
Future Directions for Global Clinical Trials
Looking ahead, the future of global clinical trials will likely be shaped by ongoing advancements in technology, regulatory harmonization efforts, and an increasing emphasis on patient-centered approaches. As digital tools become more integrated into trial processes, researchers will need to adapt their methodologies to ensure that they remain compliant with regulatory standards while maximizing participant engagement. This may involve developing new frameworks for data privacy and security as well as addressing ethical considerations related to remote participation.
Furthermore, there is a growing recognition of the importance of including diverse populations in clinical research to ensure that new therapies are effective across different demographic groups. Future trials will likely prioritize inclusivity by actively seeking out underrepresented populations and addressing barriers to participation. This shift will require collaboration among stakeholders at all levels—researchers must work closely with community leaders, healthcare providers, and regulatory bodies to create an environment conducive to equitable participation.
In conclusion, global clinical trials represent a vital component of modern medical research with far-reaching implications for healthcare access and equity worldwide. As challenges persist alongside emerging opportunities, ongoing dialogue among stakeholders will be essential for navigating this complex landscape effectively.