Hope serves as a cornerstone in the realm of clinical research, acting as a powerful motivator for patients, researchers, and healthcare professionals alike. For patients grappling with chronic illnesses or life-threatening conditions, the prospect of participating in clinical trials often embodies a glimmer of hope. This hope is not merely an abstract concept; it is a tangible force that can influence a patient’s mental and emotional well-being.
When individuals engage in clinical research, they often do so with the belief that their participation could lead to new treatments or even cures, not just for themselves but for future generations. This sense of purpose can significantly enhance their quality of life, providing them with a reason to remain optimistic amid challenging circumstances. Moreover, hope in clinical research extends beyond the individual patient experience.
It permeates the scientific community, inspiring researchers to push the boundaries of medical knowledge. The anticipation of discovering new therapies or understanding complex diseases fuels innovation and drives the scientific inquiry process. Researchers often find themselves motivated by the potential to make a difference in the lives of countless individuals.
This collective hope fosters collaboration among scientists, healthcare providers, and institutions, creating an environment where groundbreaking ideas can flourish. In this way, hope becomes a catalyst for progress, bridging the gap between theoretical research and practical application.
Key Takeaways
- Hope motivates participation and perseverance in clinical research, driving progress.
- Clinical research is essential for discovering new treatments and medical breakthroughs.
- Patients play a crucial role by contributing data and participating in studies.
- Ethical standards ensure patient safety and integrity in clinical trials.
- Emerging technologies and collaboration present new opportunities for advancing research.
How Clinical Research Leads to Medical Breakthroughs
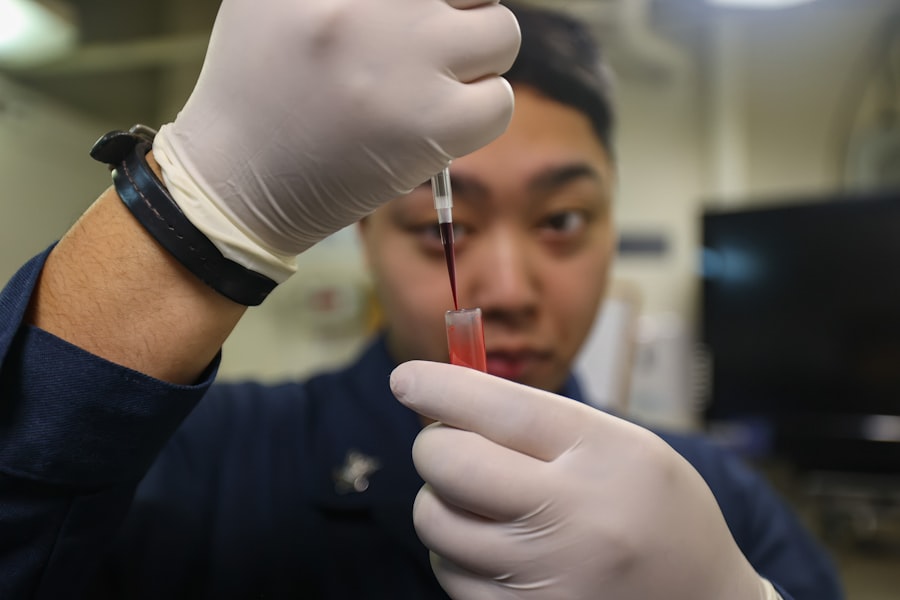
Clinical research is the bedrock upon which medical breakthroughs are built. Through meticulously designed studies, researchers gather critical data that informs the development of new treatments and therapies. For instance, the development of antiretroviral therapy for HIV/AIDS is a prime example of how clinical research can transform a once-deadly disease into a manageable condition.
Initial studies in the 1980s laid the groundwork for subsequent trials that led to the approval of various antiretroviral drugs. These breakthroughs not only improved patient outcomes but also reshaped public perception of HIV/AIDS, turning it from a death sentence into a chronic but manageable illness. Another notable example is the rapid development of mRNA vaccines during the COVID-19 pandemic.
The unprecedented speed at which these vaccines were developed and authorized for emergency use was made possible by years of prior research into mRNA technology. Clinical trials conducted by companies like Pfizer-BioNTech and Moderna demonstrated the efficacy and safety of these vaccines in record time. The success of these trials not only provided a critical tool in combating the pandemic but also opened new avenues for vaccine development against other infectious diseases and even cancer.
Such breakthroughs underscore the vital role that clinical research plays in advancing medical science and improving public health.
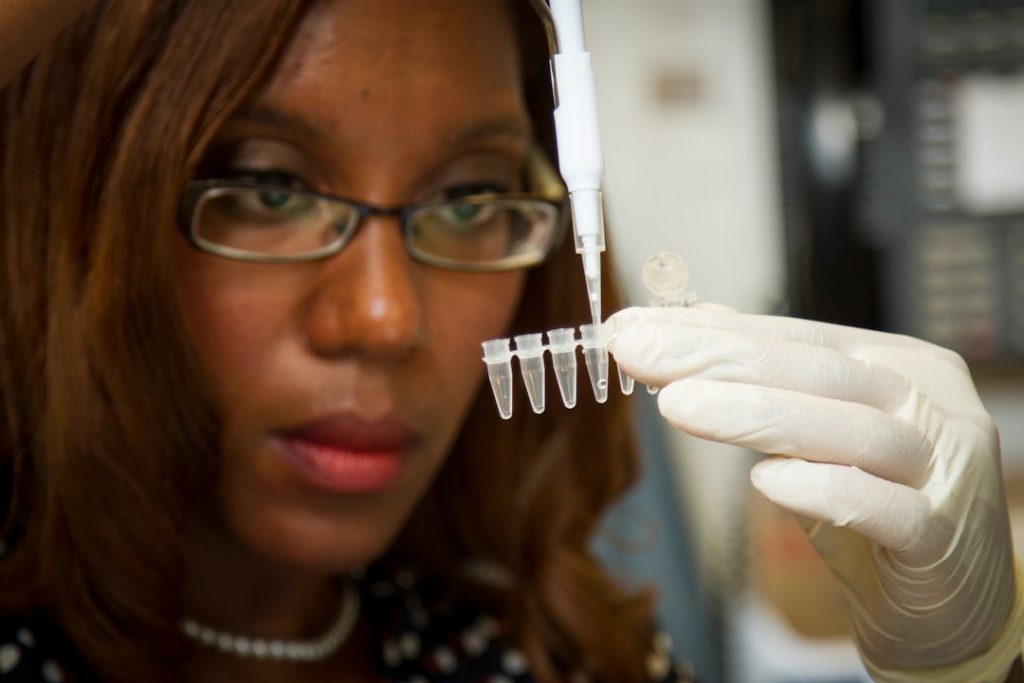
The Role of Patients in Advancing Medical Research
Patients are not merely subjects in clinical trials; they are active participants whose contributions are essential to the advancement of medical research. Their involvement provides researchers with invaluable insights into the lived experiences of those affected by various conditions. Patient-reported outcomes, which capture the patient’s perspective on their health status and treatment effects, have become increasingly important in clinical trials.
For example, in oncology research, understanding how a treatment impacts a patient’s quality of life can be just as crucial as measuring tumor shrinkage. This shift towards patient-centered research emphasizes the need for patient engagement throughout the research process. Furthermore, patients often serve as advocates for clinical research, raising awareness about specific diseases and encouraging others to participate in trials.
Organizations like the Patient-Centered Outcomes Research Institute (PCORI) have emerged to promote patient involvement in research design and implementation. By incorporating patient feedback into study protocols, researchers can ensure that trials address real-world concerns and priorities. This collaborative approach not only enhances the relevance of research findings but also fosters trust between patients and researchers, ultimately leading to more effective treatments and improved health outcomes.
Ethical Considerations in Clinical Research
Ethical considerations are paramount in clinical research, ensuring that studies are conducted with integrity and respect for participants’ rights and well-being. Informed consent is a fundamental ethical principle that requires researchers to provide potential participants with comprehensive information about the study’s purpose, procedures, risks, and benefits before they agree to participate. This process empowers individuals to make informed decisions about their involvement in research while safeguarding their autonomy.
Additionally, ethical oversight is provided by Institutional Review Boards (IRBs), which review study protocols to ensure that they meet ethical standards and protect participants from harm. The Tuskegee Syphilis Study serves as a historical reminder of the consequences of unethical research practices, highlighting the importance of transparency and accountability in clinical trials. Modern ethical guidelines emphasize the need for equitable recruitment practices to ensure diverse populations are represented in research studies.
This commitment to ethical conduct not only protects participants but also enhances the validity and generalizability of research findings.
Challenges and Opportunities in Clinical Research
| Metric | Value | Details |
|---|---|---|
| Number of Clinical Trials | 25 | Active and completed trials as of 2024 |
| Therapeutic Areas | Oncology, Neurology, Cardiology | Primary focus areas for research studies |
| Patient Enrollment | 1,200+ | Total patients enrolled across all trials |
| Study Phases | Phase I, II, III | Range of clinical trial phases conducted |
| Average Study Duration | 18 months | Typical length of clinical trials |
| Geographic Reach | North America, Europe, Asia | Regions where trials are conducted |
| Regulatory Approvals | 15 | Number of studies with regulatory clearance |
Clinical research faces numerous challenges that can hinder progress and innovation. One significant obstacle is recruitment; finding eligible participants who meet specific criteria can be time-consuming and resource-intensive. Many potential candidates may be unaware of ongoing trials or hesitant to participate due to concerns about safety or efficacy.
Additionally, regulatory hurdles can slow down the approval process for new treatments, delaying access for patients who desperately need them. Despite these challenges, there are also significant opportunities for growth and improvement within clinical research. The advent of digital health technologies has transformed how researchers engage with participants and collect data.
Telemedicine has made it easier for patients to participate in trials from their homes, broadening access to those who may have previously faced barriers due to geographic location or mobility issues. Furthermore, advancements in data analytics and artificial intelligence are enabling researchers to identify patterns and insights from vast datasets more efficiently than ever before. These innovations hold great promise for streamlining clinical trials and accelerating the pace of medical discovery.
The Impact of Clinical Research on Healthcare

The impact of clinical research on healthcare is profound and far-reaching. It serves as the foundation for evidence-based medicine, guiding clinical practice and informing treatment guidelines across various specialties. For instance, randomized controlled trials have established standard treatment protocols for conditions such as hypertension, diabetes, and heart disease, leading to improved patient outcomes and reduced healthcare costs.
Moreover, clinical research plays a crucial role in addressing public health challenges by identifying effective interventions for disease prevention and management. Vaccination programs, screening initiatives, and lifestyle modification strategies are all informed by rigorous research studies that demonstrate their efficacy. The ongoing efforts to combat antibiotic resistance exemplify how clinical research can inform public health policies aimed at preserving the effectiveness of existing treatments while developing new therapeutic options.
Future Trends in Clinical Research
As we look toward the future, several trends are poised to shape the landscape of clinical research significantly. One notable trend is the increasing emphasis on personalized medicine, which tailors treatments based on individual genetic profiles and other unique characteristics. Advances in genomics and biotechnology are enabling researchers to develop targeted therapies that offer greater efficacy with fewer side effects.
This shift towards precision medicine holds great promise for conditions such as cancer, where treatments can be customized based on specific tumor markers. Additionally, there is a growing focus on real-world evidence (RWE) as a complement to traditional clinical trial data. RWE leverages data from electronic health records, insurance claims, and patient registries to provide insights into how treatments perform in everyday clinical settings.
This approach allows researchers to assess long-term outcomes and safety profiles beyond the controlled environment of clinical trials, ultimately leading to more informed decision-making in healthcare.
The Role of Hope in the Future of Medical Breakthroughs
Hope will continue to play an integral role in shaping the future of medical breakthroughs as we navigate an increasingly complex healthcare landscape. As new technologies emerge and our understanding of diseases deepens, hope will serve as a guiding principle for both patients and researchers alike. The anticipation surrounding innovative therapies—such as gene editing techniques like CRISPR or advancements in immunotherapy—fuels optimism about what lies ahead.
Moreover, fostering a culture of hope within clinical research can enhance patient engagement and participation rates in trials. When patients believe that their involvement could lead to meaningful advancements in treatment options, they are more likely to contribute their time and resources to research efforts. This symbiotic relationship between hope and scientific inquiry will be essential as we strive to overcome existing challenges and unlock new possibilities for improving health outcomes worldwide.
In conclusion, hope remains a vital force within clinical research, driving progress and inspiring collaboration among all stakeholders involved in advancing medical science. As we continue to explore new frontiers in healthcare, nurturing this sense of hope will be crucial for realizing the full potential of clinical research in transforming lives through innovative treatments and therapies.