Clinical trials are a cornerstone of medical progress, acting as rigorous gateways for new treatments to reach patients. However, the journey from initial concept to regulatory approval is often fraught with challenges, impacting timelines, costs, and ultimately, the accessibility of life-changing therapies. This article explores optimization solutions designed to maximize the efficiency and effectiveness of clinical trials. Think of a clinical trial not as a single step, but as a complex ecosystem where each component plays a vital role. If one part falters, the entire system can become sluggish or even break down. Optimization seeks to fine-tune these interconnected elements.
The protocol is the blueprint of a clinical trial, dictating every aspect from patient selection criteria to data collection methods. A poorly designed protocol is like building a house on shaky foundations; it invites problems down the line. Therefore, robust protocol design is paramount for efficient trial execution.
Evidence-Based Protocol Generation
Modern protocol development increasingly leverages existing data and evidence to inform design choices. This can include meta-analyses of prior trials, real-world data, and insights from mechanistic studies. The goal is to avoid reinventing the wheel and to build upon established knowledge, ensuring the trial addresses a relevant clinical question with a scientifically sound methodology. This approach helps to clarify the critical questions the trial seeks to answer and the most effective ways to find those answers.
Adaptive Trial Designs
Traditional trials often follow a fixed path. Adaptive trial designs, in contrast, allow for pre-specified modifications to the trial’s course based on accumulating data. This can involve adjusting sample size, changing dosage regimens, or even modifying treatment arms. Adaptive designs are like navigating a ship with advanced sonar; they can adjust course in real-time based on changing conditions, rather than rigidly sticking to a pre-set route. This flexibility can lead to faster recruitment, reduced study duration, and a greater likelihood of demonstrating efficacy or futility sooner, thereby conserving resources.
Patient-Centric Protocol Development
Shifting the focus to the patient experience is central to modern optimization. This involves designing protocols that are less burdensome for participants, considering factors like the number of site visits, the invasiveness of procedures, and the clarity of informed consent documents. A patient-centric approach can improve recruitment and retention rates, which are often significant bottlenecks in trial progression. Engaging patient advocacy groups and patient representatives in the design phase can provide invaluable perspectives.
Leveraging Technology in Protocol Development
Software tools and artificial intelligence are beginning to play a more significant role in protocol development. These technologies can assist in identifying potential design flaws, predicting recruitment challenges, and ensuring compliance with regulatory guidelines. Predictive analytics can forecast potential issues before they arise, allowing for proactive mitigation strategies.
Enhancing Patient Recruitment and Retention
Patient recruitment and retention are frequently cited as the most significant hurdles in clinical trial operations. Without sufficient participants who remain engaged throughout the study, even the most promising therapies may fail to demonstrate their value. Achieving high recruitment and retention is akin to ensuring a steady flow of essential components to a manufacturing line; any disruption can halt production.
Strategic Site Selection
The choice of clinical trial sites is critical. Sites should be selected based on their patient population demographics, their experience with similar trials, their existing infrastructure, and their track record of successful patient enrollment. A scattered approach to site selection, without a clear understanding of local patient populations, is inefficient. Geographic distribution and accessibility for patients, including public transportation and parking, are also important considerations.
Decentralized Clinical Trials (DCTs) and Hybrid Models
Decentralized clinical trials move away from the traditional model where patients must visit a physical site for all study-related activities. This can involve remote monitoring, telehealth consultations, and home healthcare visits. Hybrid models combine elements of both traditional and decentralized approaches. DCTs can significantly broaden the potential patient pool by reducing geographical barriers and minimizing patient burden, thereby acting as a powerful tool to unlock access to trials for a wider range of individuals.
Digital Recruitment Strategies
The digital landscape offers numerous avenues for patient recruitment. This includes utilizing social media advertising, online patient communities, and partnerships with patient advocacy organizations. Targeted online campaigns can reach specific patient populations who may be unaware of relevant clinical trials. Building an online presence that educates potential participants about research opportunities is a proactive recruitment strategy.
Improving the Informed Consent Process
The informed consent process is not merely a regulatory requirement; it is a fundamental ethical obligation and a critical component of patient retention. Simplifying complex medical jargon, providing multi-format information (videos, infographics), and allowing ample time for questions and discussion can improve patient understanding and confidence. A clear and transparent consent process builds trust, which is essential for long-term participant engagement.
Proactive Patient Support and Engagement
Maintaining patient engagement requires ongoing effort. This can involve regular communication from study coordinators, personalized reminders about appointments, and addressing any concerns or issues promptly. Creating a supportive environment where patients feel valued and heard is crucial for preventing dropout. This can also extend to providing logistical support, such as travel assistance or childcare, to alleviate common barriers to participation.
Optimizing Data Management and Analytics

The data generated by clinical trials is the bedrock upon which treatment decisions are made. Efficient and accurate data management is not just about storage; it’s about transforming raw information into actionable insights. Poor data management is like having a library with misplaced books; valuable information is present but inaccessible or unreliable.
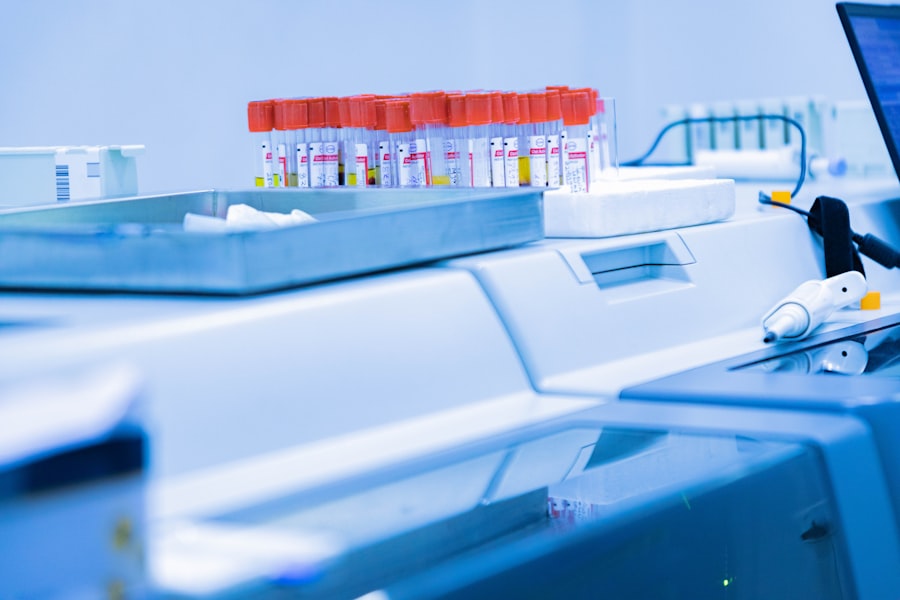
Electronic Data Capture (EDC) Systems
The adoption of Electronic Data Capture (EDC) systems has revolutionized data management. EDC systems streamline data entry, reduce transcription errors, and enable real-time data access and review. This digital transformation of data collection moves away from cumbersome paper-based systems, allowing for quicker identification of trends and inconsistencies.
Data Standardization and Interoperability
Standardizing data formats and ensuring interoperability between different systems are crucial for efficient data analysis. This allows for seamless integration of data from various sources, including EDC, laboratory systems, and wearable devices. A common data language ensures that information from different research endeavors can be understood and compared, fostering collaboration and accelerating discovery.
Real-Time Data Monitoring and Analytics
Real-time data monitoring allows study teams to identify potential issues, such as deviations from the protocol or unexpected safety signals, as they emerge. Advanced analytics, including predictive modeling and machine learning, can uncover subtle patterns and trends in the data that might otherwise go unnoticed. This proactive approach to data analysis is like having a vigilant air traffic controller; it monitors all incoming flights (data) and can alert to potential collisions (issues) before they occur.
Data Integrity and Security Measures
Maintaining the integrity and security of clinical trial data is paramount. Robust validation processes, audit trails, and access controls are essential to ensure that the data is accurate, reliable, and protected from unauthorized access or alteration. This builds trust in the findings and ensures regulatory compliance.
Leveraging Artificial Intelligence (AI) in Data Analysis
AI and machine learning are increasingly being employed to analyze vast datasets, identify biomarkers, predict treatment responses, and even assist in the development of new trial designs. AI can sift through complex data with a speed and precision that surpasses human capabilities, uncovering insights that can accelerate the drug development process.
Streamlining Operational Efficiency and Cost Management
Clinical trial costs can be substantial, and inefficiencies can exacerbate these expenses, impacting the affordability and accessibility of new treatments. Optimizing operational aspects is key to ensuring that resources are used effectively. Think of operational efficiency as a well-oiled engine; every part working in harmony to maximize output with minimal waste.
Centralized Trial Management
Centralized trial management models, as opposed to decentralized approaches to oversight, can consolidate administrative and operational functions, leading to greater consistency and efficiency. This can include centralizing contract negotiation, site monitoring, and financial management. A unified command center for trial operations can reduce duplication of effort and ensure adherence to standardized procedures.
Outsourcing and Strategic Partnerships
Engaging Contract Research Organizations (CROs) and other specialized service providers can bring expertise and resources that may not be available in-house. Strategic partnerships can optimize specific aspects of trial execution, such as data management, pharmacovigilance, or patient recruitment. Selecting the right partners is as crucial as choosing the right team members for a complex project.
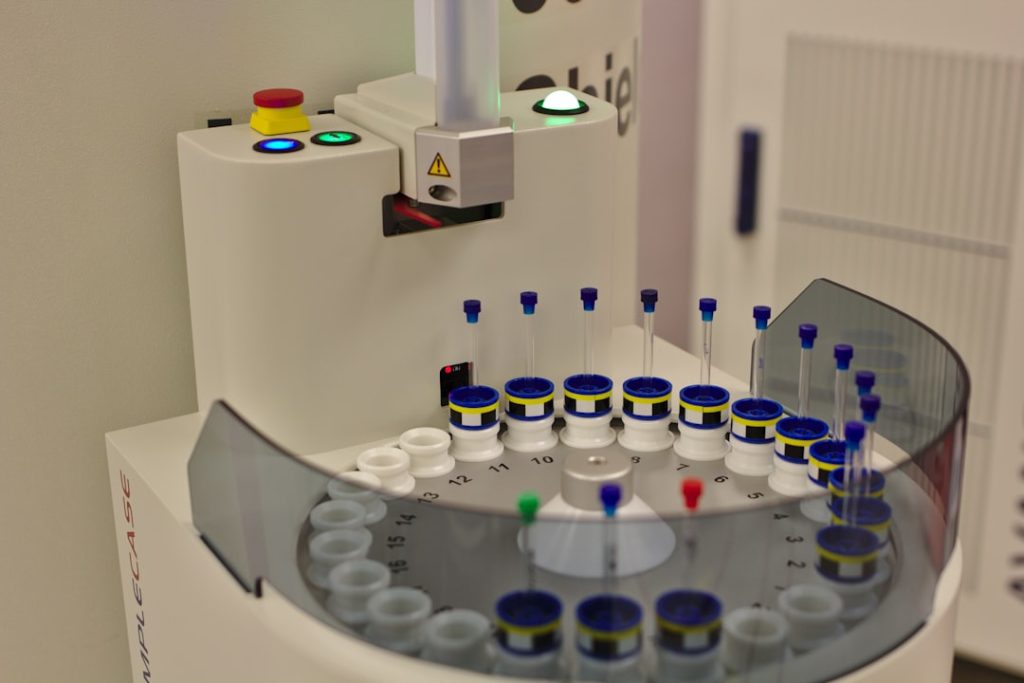
Supply Chain Management for Investigational Products
Efficient management of the investigational product supply chain is critical. This includes forecasting demand, managing inventory, and ensuring timely delivery to study sites. Disruptions in the supply chain can lead to trial delays and increased costs. A well-managed supply chain is the lifeblood of a trial, ensuring that treatments are available when and where they are needed.
Risk-Based Monitoring (RBM)
Risk-Based Monitoring shifts the focus from traditional, comprehensive site monitoring to a more targeted approach. It involves identifying critical study processes and data points that pose the greatest risk to data integrity and patient safety, and then focusing monitoring efforts on those areas. This allows for more efficient allocation of monitoring resources, ensuring that the most important aspects are under close scrutiny, like a spotlight illuminating critical passageways.
Budget Management and Cost Containment
Rigorous budget management, including detailed cost forecasting, regular review of expenditures, and identification of cost-saving opportunities, is essential. Early identification of potential cost overruns and the implementation of corrective actions can prevent significant financial strain.
Enhancing Regulatory Compliance and Quality Assurance
| Metric | Description | Typical Value | Impact on Clinical Trial |
|---|---|---|---|
| Patient Recruitment Rate | Speed at which eligible patients are enrolled | 5-10 patients per site per month | Faster recruitment shortens trial duration |
| Screen Failure Rate | Percentage of patients who fail eligibility criteria | 20-30% | Lower rates improve efficiency and reduce costs |
| Protocol Deviation Rate | Frequency of deviations from the trial protocol | 5-15% | Minimizing deviations ensures data integrity |
| Data Entry Error Rate | Percentage of errors in clinical data entry | 1-3% | Lower error rates improve data quality and analysis |
| Site Activation Time | Time taken to initiate a clinical trial site | 30-60 days | Reducing activation time accelerates trial start |
| Patient Retention Rate | Percentage of patients completing the trial | 80-90% | Higher retention improves study validity |
| Cost per Patient | Average cost incurred per enrolled patient | Varies widely by trial phase and indication | Optimization reduces overall trial expenses |
Adherence to regulatory requirements and maintaining high quality standards are non-negotiable in clinical trials. Failure in these areas can lead to costly delays, rejections, or even the invalidation of trial results. Regulatory compliance is the bedrock upon which the trustworthiness of medical research is built; without it, the entire edifice crumbles.
Proactive Regulatory Strategy and Planning
Developing a proactive regulatory strategy from the outset of a trial is crucial. This involves understanding the requirements of relevant regulatory agencies (e.g., FDA, EMA) and incorporating them into the protocol design and operational plans. Early engagement with regulatory bodies can also provide valuable guidance and prevent misunderstandings.
Robust Quality Management Systems (QMS)
Implementing a comprehensive Quality Management System (QMS) ensures that all trial activities are conducted in accordance with established procedures and regulatory standards. A QMS provides a framework for consistent quality and continuous improvement. It acts as the internal compass guiding all trial activities towards adherence to standards.
Regular Internal Audits and Inspections
Conducting regular internal audits and inspections helps to identify and address potential compliance issues before they become significant problems. These internal reviews serve as a dress rehearsal for external inspections, allowing teams to refine their processes and documentation.
Training and Competency Assessment of Study Staff
Ensuring that all study staff are adequately trained and competent in their respective roles is fundamental to quality and compliance. This includes training on the protocol, Good Clinical Practice (GCP) guidelines, and specific study procedures. Competency assessments verify that training has been effective.
Leveraging Technology for Compliance Monitoring
Technology can play a vital role in monitoring compliance. This includes using software for electronic trial master files (eTMF), audit trail review, and deviation management. These tools can automate many compliance-related tasks and provide real-time visibility into compliance status.
By implementing these optimization solutions, the clinical trial process can become more efficient, cost-effective, and ultimately, more successful in bringing vital new therapies to patients. The continuous pursuit of betterment in each of these areas is what propels medical innovation forward.