Lung cancer remains one of the most prevalent and deadly forms of cancer worldwide, accounting for a significant number of cancer-related deaths each year. According to the World Health Organization, lung cancer is responsible for approximately 1.8 million deaths annually, making it the leading cause of cancer mortality globally. The disease primarily arises from the uncontrolled growth of abnormal cells in the lungs, which can form tumors that disrupt normal respiratory function.
The two main types of lung cancer are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), with NSCLC being the more common variant, representing about 85% of all cases. The risk factors associated with lung cancer are well-documented, with smoking being the most significant contributor. However, non-smokers can also develop lung cancer due to factors such as exposure to secondhand smoke, environmental pollutants, and genetic predispositions.
The symptoms often manifest in the later stages of the disease, making early detection challenging. Common signs include persistent cough, chest pain, weight loss, and difficulty breathing. Given the complexity of lung cancer and its treatment landscape, understanding current therapies and emerging research is crucial for patients and healthcare providers alike.
Key Takeaways
- Lung cancer treatment is evolving with ongoing clinical trials testing new therapies.
- Clinical trials are crucial for developing more effective lung cancer treatments.
- Patient eligibility criteria determine who can participate in specific clinical trials.
- Participating in trials offers potential benefits but also carries certain risks.
- Finding and enrolling in trials can provide access to cutting-edge treatments and impact future care.
Current Treatment Options
The treatment landscape for lung cancer has evolved significantly over the past few decades, incorporating a range of modalities tailored to the specific type and stage of the disease. For early-stage non-small cell lung cancer, surgical resection remains a cornerstone of treatment. This may involve lobectomy, where a lobe of the lung is removed, or pneumonectomy, which entails the removal of an entire lung.
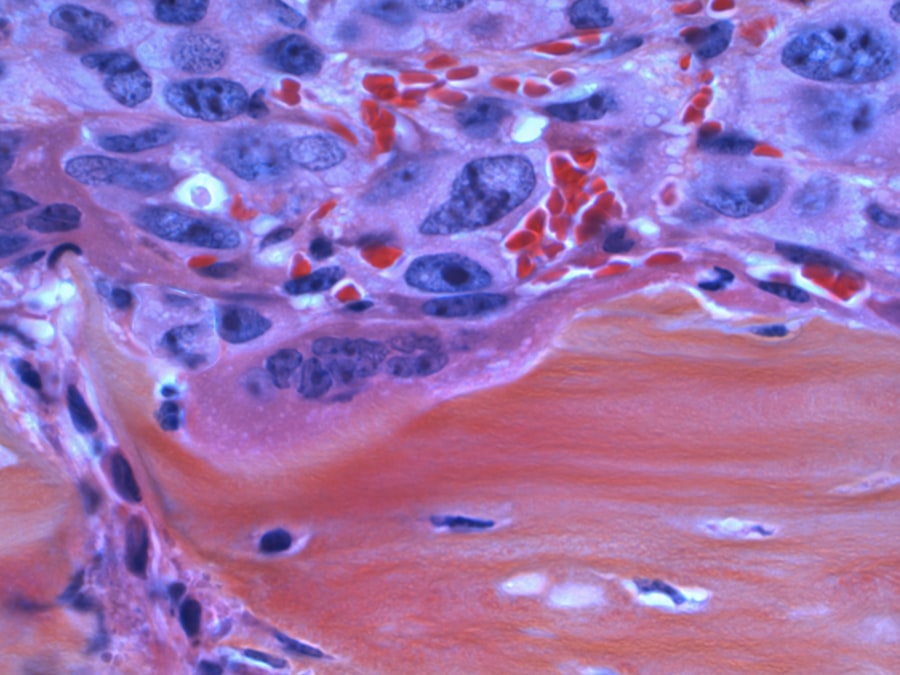
In cases where surgery is not feasible due to the tumor’s location or the patient’s overall health, radiation therapy may be employed as a curative or palliative measure. For advanced stages of lung cancer, systemic therapies such as chemotherapy and targeted therapy play a pivotal role. Chemotherapy utilizes cytotoxic drugs to kill rapidly dividing cancer cells but often comes with significant side effects due to its impact on healthy cells.
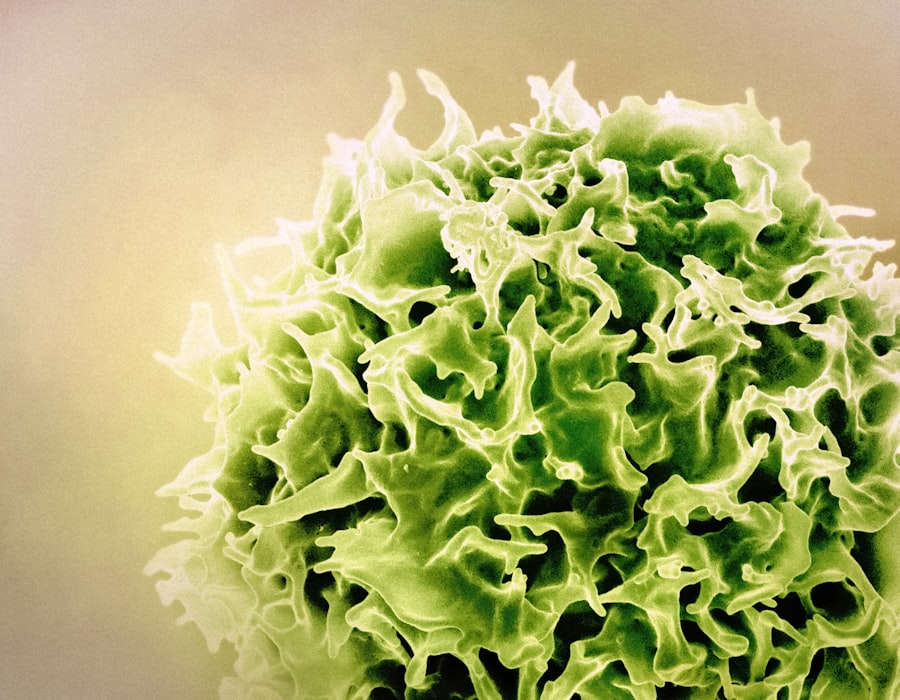
Targeted therapies, on the other hand, focus on specific molecular targets associated with cancer growth. For instance, drugs like erlotinib and gefitinib target mutations in the epidermal growth factor receptor (EGFR), which are prevalent in certain NSCLC patients. Immunotherapy has also emerged as a revolutionary approach, harnessing the body’s immune system to fight cancer cells.
Agents like pembrolizumab and nivolumab have shown promise in improving survival rates for patients with advanced lung cancer.
Importance of Clinical Trials
Clinical trials are essential for advancing our understanding of lung cancer and improving treatment outcomes. These studies are designed to evaluate new therapies, assess their efficacy and safety, and determine optimal dosing regimens. By participating in clinical trials, patients gain access to cutting-edge treatments that may not yet be available through standard care protocols.
Moreover, clinical trials contribute to the broader scientific knowledge base, helping researchers identify which therapies work best for specific patient populations. The significance of clinical trials extends beyond individual patient benefits; they are crucial for developing new standards of care. For example, many current treatment options for lung cancer have emerged from rigorous clinical trials that tested novel agents against existing therapies.
The data generated from these studies inform clinical guidelines and help shape future research directions. Furthermore, clinical trials often include diverse patient populations, which can lead to more inclusive treatment strategies that consider variations in genetics, ethnicity, and comorbidities.
New Therapies Being Tested
| Therapy Name | Type | Target Condition | Phase of Trial | Primary Outcome Measure | Estimated Completion Date |
|---|---|---|---|---|---|
| TheraCure-1 | Gene Therapy | Cystic Fibrosis | Phase 2 | Improvement in lung function (FEV1) | 2025-03 |
| ImmunoX | Monoclonal Antibody | Rheumatoid Arthritis | Phase 3 | Reduction in joint inflammation | 2024-12 |
| NeuroHeal | Small Molecule Drug | Alzheimer’s Disease | Phase 1 | Safety and tolerability | 2024-09 |
| OncoVax | Cancer Vaccine | Melanoma | Phase 2 | Immune response activation | 2025-06 |
| CardioRestore | Stem Cell Therapy | Heart Failure | Phase 3 | Improvement in ejection fraction | 2025-01 |
The landscape of lung cancer treatment is continually evolving, with numerous new therapies currently under investigation in clinical trials. One promising area of research involves the development of novel immunotherapeutic agents that aim to enhance the immune response against tumor cells. For instance, bispecific T-cell engagers (BiTEs) are designed to redirect T-cells to recognize and attack cancer cells more effectively.
Early-phase trials have shown encouraging results in patients with advanced lung cancer who have exhausted standard treatment options. Another exciting avenue is the exploration of combination therapies that integrate different treatment modalities to improve efficacy. For example, combining immunotherapy with targeted therapy has shown potential in overcoming resistance mechanisms that often limit treatment success.
Trials investigating combinations such as checkpoint inhibitors with anti-angiogenic agents or chemotherapy are ongoing and may lead to more effective treatment regimens for patients with various subtypes of lung cancer.
Patient Eligibility for Clinical Trials
Eligibility criteria for clinical trials are established to ensure patient safety and to create a homogenous study population that can yield reliable results. These criteria often include factors such as age, overall health status, stage of disease, previous treatments received, and specific genetic markers associated with lung cancer. For instance, some trials may focus exclusively on patients with specific mutations like ALK or ROS1 rearrangements, while others may be open to a broader range of participants.
Patients interested in participating in clinical trials should engage in thorough discussions with their healthcare providers to understand the specific eligibility requirements for each study. It is also essential for patients to consider their own health conditions and preferences when evaluating potential participation in a trial. Some trials may require frequent visits for monitoring or involve experimental treatments that could lead to unknown side effects.
Therefore, informed consent is a critical component of the process, ensuring that patients are fully aware of what participation entails.
Potential Benefits and Risks of Participating
Participating in a clinical trial can offer several potential benefits for patients with lung cancer. One significant advantage is access to innovative treatments that may not yet be available through standard care pathways. These therapies could provide hope for patients who have limited options due to advanced disease or previous treatment failures.
Additionally, participants often receive close monitoring from healthcare professionals throughout the trial period, which can lead to more personalized care. However, there are inherent risks associated with clinical trial participation that patients must consider carefully. Experimental treatments may not be effective for everyone and could lead to unexpected side effects or complications that are not yet fully understood.
Furthermore, some trials may involve placebo groups where participants receive no active treatment at all, which can be particularly challenging for those with advanced disease seeking immediate relief from symptoms. Patients should weigh these potential risks against the possible benefits and discuss their concerns openly with their healthcare team before making a decision.
How to Find and Enroll in a Clinical Trial
Finding a suitable clinical trial can be a daunting task for patients navigating their lung cancer journey. Several resources are available to assist individuals in locating trials that match their specific circumstances. Websites such as ClinicalTrials.gov provide comprehensive databases of ongoing studies across various conditions, including lung cancer.
Patients can search by location, type of cancer, and other relevant criteria to identify potential trials. Once a patient identifies a trial of interest, the next step involves contacting the research team or institution conducting the study. This initial communication typically includes an assessment of eligibility based on the trial’s criteria and an explanation of what participation entails.
Healthcare providers can also play a vital role in this process by referring patients to appropriate trials or providing insights into ongoing research initiatives within their institutions.
Future Implications for Lung Cancer Treatment
The future implications for lung cancer treatment are promising as research continues to advance our understanding of this complex disease. With ongoing investigations into personalized medicine approaches—tailoring treatments based on individual genetic profiles—there is potential for more effective therapies that minimize side effects while maximizing efficacy. The integration of artificial intelligence and machine learning into oncology research may further enhance our ability to predict treatment responses and identify suitable candidates for specific therapies.
Moreover, as new therapeutic agents emerge from clinical trials, there is hope for improved survival rates and quality of life for patients diagnosed with lung cancer. The shift towards combination therapies and novel immunotherapeutic strategies signifies a transformative era in oncology where multidisciplinary approaches may become standard practice. As researchers continue to unravel the complexities of lung cancer biology and treatment resistance mechanisms, the horizon looks increasingly optimistic for those affected by this challenging disease.




