Treatment efficacy measures how well a medical intervention produces its intended therapeutic effect under controlled, optimal conditions. This metric serves as a fundamental standard for evaluating healthcare interventions and guides clinical decision-making for healthcare providers, researchers, and patients. Clinical trials represent the primary method for assessing treatment efficacy.
These studies compare the performance of specific interventions against control groups or alternative treatments using standardized protocols and controlled environments. The data generated from these trials provides quantitative evidence of a treatment’s ability to achieve desired clinical outcomes. Evidence-based medicine has increased the significance of treatment efficacy data in modern healthcare systems.
Healthcare providers rely on efficacy measurements to select appropriate therapies, develop treatment guidelines, and optimize patient outcomes. This systematic approach to treatment evaluation supports both individual patient care and population health management strategies. Treatment efficacy data enables healthcare professionals to make objective, data-driven treatment recommendations.
This evidence-based approach improves the consistency and quality of medical care while supporting the development of standardized treatment protocols across healthcare institutions.
Key Takeaways
- Treatment efficacy was systematically evaluated through a rigorous clinical research methodology.
- The study revealed significant findings that impact current patient care practices.
- Limitations were acknowledged, highlighting the need for further research to validate results.
- The study contributes valuable insights to the medical field, informing healthcare provider decisions.
- Recommendations emphasize ongoing research and adaptation of treatment protocols for improved outcomes.
Methodology of the Clinical Research Study
The methodology employed in clinical research studies is foundational to the integrity and validity of the findings. A well-structured study typically begins with a clear hypothesis that outlines the expected relationship between the treatment and its outcomes. In this context, researchers often utilize randomized controlled trials (RCTs) as the gold standard for assessing treatment efficacy.
RCTs involve randomly assigning participants to either an experimental group receiving the treatment or a control group receiving a placebo or standard care. This randomization helps eliminate bias and ensures that any observed effects can be attributed to the intervention itself. In addition to randomization, researchers must carefully define inclusion and exclusion criteria for study participants.
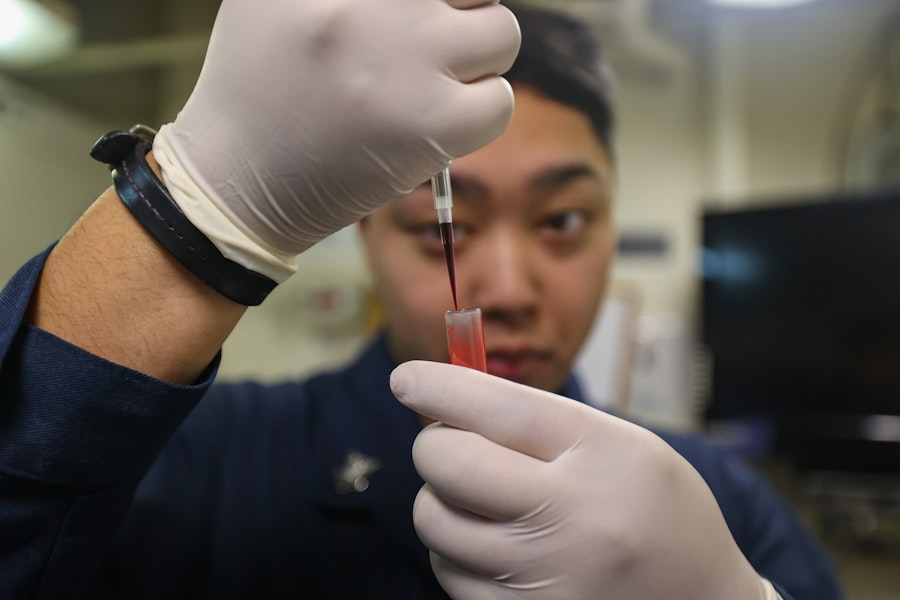
These criteria ensure that the study population is representative of the broader patient population while controlling for confounding variables that could skew results. Data collection methods are also crucial; they may include standardized questionnaires, clinical assessments, and laboratory tests to measure outcomes accurately. Furthermore, researchers often employ blinding techniques, where participants and/or investigators are unaware of group assignments, to minimize bias in reporting and assessing outcomes.
Findings and Results of the Study

The findings of a clinical research study are typically presented through a combination of statistical analyses and descriptive data. Researchers analyze the data collected during the trial to determine whether the treatment had a statistically significant effect on the primary outcome measures. For instance, if a new medication is being tested for its efficacy in reducing symptoms of a chronic condition, researchers would compare symptom scores between the treatment and control groups at various time points throughout the study.
Results may also be stratified by demographic factors such as age, gender, or comorbidities to identify any differential effects of the treatment across subpopulations. In many cases, researchers will report not only the primary outcomes but also secondary outcomes that may provide additional insights into the treatment’s overall impact on patient health and quality of life. For example, alongside symptom reduction, researchers might assess changes in functional status or patient-reported outcomes, which can offer a more comprehensive view of how a treatment affects patients’ daily lives.
Implications for Patient Care
The implications of research findings on treatment efficacy extend far beyond the confines of academic journals; they have profound effects on patient care practices. When a treatment is shown to be effective, it can lead to changes in clinical guidelines and protocols, ultimately influencing how healthcare providers approach patient management. For instance, if a new therapy demonstrates superior efficacy compared to existing treatments for a specific condition, clinicians may adopt this therapy as a first-line option, thereby improving patient outcomes.
Moreover, understanding treatment efficacy can empower patients in their healthcare decisions. When patients are informed about the effectiveness of various treatment options, they can engage in shared decision-making with their healthcare providers. This collaborative approach fosters a sense of agency among patients and can lead to increased adherence to treatment plans.
Additionally, when patients are aware of evidence-based treatments that have been proven effective, they may feel more confident in their care journey, which can enhance their overall satisfaction with the healthcare system.
Limitations and Future Research Directions
| Metric | Description | Typical Value/Range | Importance |
|---|---|---|---|
| Enrollment Rate | Number of participants enrolled per month | 5-50 participants/month | Measures recruitment efficiency |
| Retention Rate | Percentage of participants completing the study | 70%-95% | Indicates participant adherence and study validity |
| Adverse Event Rate | Incidence of adverse events reported during the study | Varies by study type | Assesses safety of intervention |
| Protocol Deviation Rate | Percentage of participants with protocol deviations | 1%-10% | Reflects study quality and compliance |
| Data Query Rate | Number of data queries per 100 data points | 5-15 queries/100 data points | Indicates data quality and accuracy |
| Time to Database Lock | Duration from last patient visit to database lock | 1-3 months | Measures study data finalization speed |
| Study Completion Rate | Percentage of studies completed on time | 60%-85% | Reflects overall study management efficiency |
Despite the rigorous methodologies employed in clinical research studies, limitations often exist that can affect the interpretation of findings. One common limitation is the generalizability of results; findings from a specific study population may not be applicable to all patients with a given condition. For example, if a study primarily includes younger adults, its results may not be relevant for older populations who may respond differently to treatments due to age-related physiological changes.
Additionally, many studies face challenges related to sample size and duration. Small sample sizes can limit statistical power and increase the risk of Type I and Type II errors, while short study durations may not capture long-term effects or adverse events associated with treatments. Future research directions should focus on addressing these limitations by conducting larger-scale studies with diverse populations and longer follow-up periods.
Furthermore, exploring real-world evidence through observational studies can complement clinical trial data and provide insights into how treatments perform in everyday practice.
Discussion of the Study’s Contribution to the Field
The contribution of a clinical research study to its field is often measured by its ability to advance knowledge and inform practice. A well-executed study that demonstrates significant treatment efficacy can pave the way for further investigations into related areas. For instance, if a new drug shows promise in treating a chronic illness, subsequent studies may explore its mechanisms of action, optimal dosing regimens, or potential interactions with other medications.
Moreover, studies that identify specific patient populations that benefit most from a treatment can lead to more personalized approaches in medicine. This shift towards precision medicine emphasizes tailoring interventions based on individual characteristics rather than adopting a one-size-fits-all approach. As researchers continue to build on existing knowledge through innovative studies, they contribute to an evolving understanding of disease management and therapeutic strategies.
Considerations for Healthcare Providers
Healthcare providers play a pivotal role in translating research findings into clinical practice. To effectively implement evidence-based treatments, providers must stay informed about the latest research developments and understand how these findings apply to their patient populations. This requires ongoing education and training in interpreting clinical trial data and integrating it into patient care strategies.
Additionally, providers should consider individual patient factors when recommending treatments based on efficacy data. Factors such as comorbidities, patient preferences, and potential side effects must be weighed against the benefits of a given intervention. Engaging patients in discussions about their treatment options fosters an environment of shared decision-making and enhances adherence to prescribed therapies.
Conclusion and Recommendations for Further Action
In light of the critical importance of treatment efficacy in guiding clinical practice, it is essential for stakeholders within healthcare—researchers, clinicians, policymakers—to prioritize ongoing research efforts aimed at evaluating new therapies and refining existing ones. Future studies should strive for inclusivity in participant selection to ensure that findings are applicable across diverse populations. Furthermore, healthcare systems should invest in infrastructure that supports continuous education for providers regarding emerging evidence-based practices.
By fostering an environment where research informs practice and patient engagement is prioritized, we can enhance treatment efficacy and ultimately improve health outcomes for all patients.



