Effective site management is a cornerstone of successful clinical trials, serving as the bridge between the research objectives and the practical realities of conducting studies. The management of clinical trial sites encompasses a wide array of responsibilities, including the selection of appropriate sites, ensuring compliance with regulatory requirements, and maintaining the integrity of data collection. A well-managed site can significantly enhance the quality of the trial, leading to more reliable results and ultimately contributing to the advancement of medical science.
The importance of effective site management cannot be overstated; it directly impacts patient safety, data quality, and the overall timeline of the trial. Moreover, effective site management fosters a collaborative environment among stakeholders, including sponsors, investigators, and site staff. This collaboration is essential for addressing challenges that may arise during the trial, such as recruitment difficulties or unexpected regulatory changes.
When site management is executed proficiently, it not only streamlines operations but also builds trust among all parties involved. This trust is crucial for maintaining participant engagement and ensuring that the trial adheres to ethical standards. In essence, effective site management is not merely an operational necessity; it is a strategic imperative that can determine the success or failure of a clinical trial.
Key Takeaways
- Effective site management is crucial for the success and integrity of clinical trials.
- Common challenges include site selection, patient recruitment, regulatory compliance, and communication barriers.
- Streamlining site selection and activation accelerates trial initiation and reduces delays.
- Utilizing technology enhances patient recruitment, data management, and overall site efficiency.
- Continuous performance monitoring and strong collaboration improve trial outcomes and compliance.
Key Challenges in Clinical Trial Site Management
Clinical trial site management is fraught with challenges that can impede progress and compromise the integrity of the study. One of the most significant challenges is the recruitment and retention of participants. Many trials struggle to meet their enrollment targets due to various factors, including stringent eligibility criteria, competition from other studies, and a lack of awareness among potential participants about the benefits of clinical trials.
This challenge is compounded by the need for diverse participant populations to ensure that findings are generalizable across different demographics. Another critical challenge lies in regulatory compliance. Clinical trials are subject to a myriad of regulations that vary by country and region.
Navigating these complex regulatory landscapes requires meticulous attention to detail and a thorough understanding of local laws and guidelines. Failure to comply with these regulations can lead to severe consequences, including delays in trial timelines, financial penalties, or even termination of the study. Additionally, maintaining compliance necessitates ongoing training and education for site staff, which can strain resources and divert attention from other essential tasks.
Strategies for Streamlining Site Selection and Activation

Streamlining site selection and activation is vital for expediting clinical trials and ensuring that they remain on schedule. One effective strategy is to develop a comprehensive site feasibility assessment process that evaluates potential sites based on their capabilities, experience, and patient population. This assessment should include an analysis of the site’s previous performance in clinical trials, as well as its infrastructure and resources.
By identifying sites with a proven track record, sponsors can minimize risks associated with underperforming sites. Another strategy involves leveraging data analytics to inform site selection decisions. By utilizing historical data from previous trials, sponsors can identify trends and patterns that indicate which sites are more likely to succeed in recruiting participants and adhering to protocols.
Additionally, employing technology platforms that facilitate real-time communication between sponsors and sites can expedite the activation process. These platforms can streamline document submissions, approvals, and training sessions, thereby reducing delays that often plague traditional activation methods.
Best Practices for Efficient Patient Recruitment and Retention
Efficient patient recruitment and retention are critical components of successful clinical trials. One best practice is to engage with potential participants early in the process through community outreach initiatives. By educating the public about the importance of clinical trials and addressing common misconceptions, sponsors can foster a more informed patient population that is willing to participate.
Collaborating with healthcare providers to identify potential participants can also enhance recruitment efforts, as these providers can serve as trusted sources of information. Retention strategies are equally important, as losing participants midway through a trial can compromise data integrity. Implementing regular follow-ups and maintaining open lines of communication with participants can help keep them engaged throughout the study.
Providing incentives, such as travel reimbursements or access to new treatments, can also encourage participants to remain involved. Additionally, creating a supportive environment at the trial site—where participants feel valued and heard—can significantly enhance retention rates.
Leveraging Technology for Improved Site Management
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Patient Enrollment Rate | Number of patients enrolled per site per month | 5-15 patients/month | High – impacts study timelines |
| Screen Failure Rate | Percentage of screened patients who do not meet inclusion criteria | 20-40% | Medium – affects recruitment efficiency |
| Protocol Deviation Rate | Number of deviations per 100 patient visits | 1-5 deviations/100 visits | High – affects data quality and compliance |
| Query Resolution Time | Average time to resolve data queries raised by monitors | 3-7 days | High – impacts data cleaning and database lock |
| Site Activation Time | Time from site selection to site initiation visit | 4-8 weeks | Medium – affects overall study start-up |
| Monitoring Visit Frequency | Number of monitoring visits per site per month | 1-2 visits/month | Medium – ensures compliance and data integrity |
| Adverse Event Reporting Timeliness | Time from event occurrence to reporting | 24-72 hours | High – critical for patient safety |
| Data Entry Lag | Time between patient visit and data entry into EDC | 1-3 days | Medium – affects real-time data monitoring |
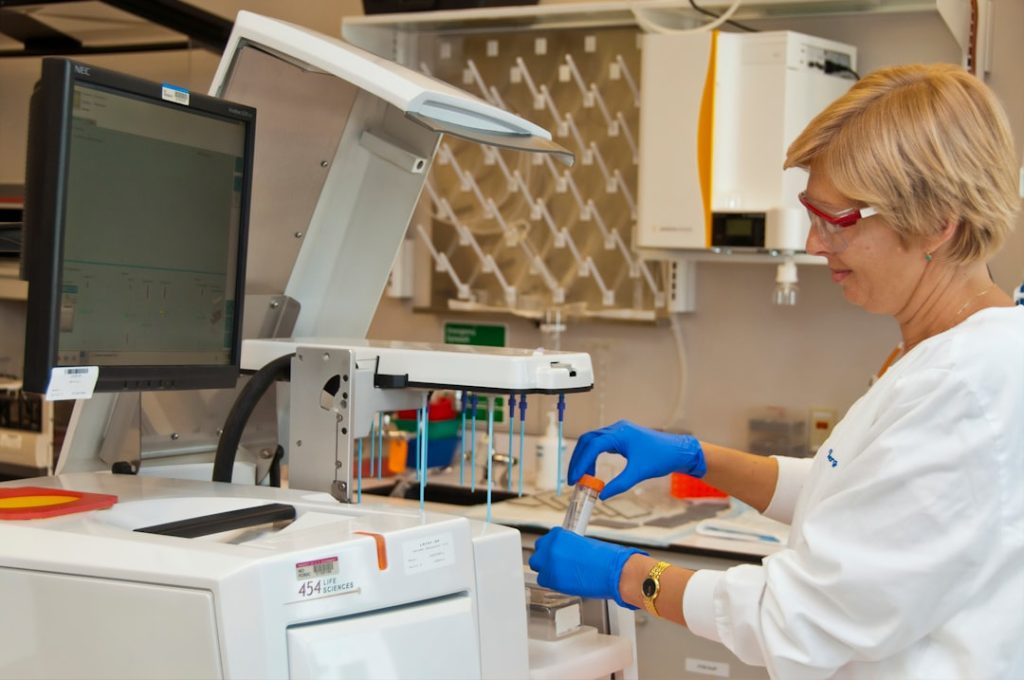
The integration of technology into clinical trial site management has revolutionized how studies are conducted. Electronic data capture (EDC) systems have replaced traditional paper-based methods, allowing for more efficient data collection and real-time monitoring of trial progress. These systems not only reduce the risk of errors associated with manual data entry but also facilitate quicker access to critical information for decision-making.
Moreover, technology can enhance communication among stakeholders involved in clinical trials. Platforms that enable secure messaging and document sharing streamline collaboration between sponsors and site staff, ensuring that everyone is on the same page regarding study protocols and timelines. Additionally, mobile applications designed for patient engagement can improve participant adherence by providing reminders for appointments or medication schedules.
By leveraging these technological advancements, clinical trial sites can operate more efficiently while maintaining high standards of quality and compliance.
Overcoming Regulatory and Compliance Hurdles in Site Management

Navigating regulatory and compliance hurdles is one of the most daunting aspects of clinical trial site management. Each country has its own set of regulations governing clinical research, which can create confusion for sponsors and site staff alike. To overcome these challenges, it is essential to establish a robust compliance framework that includes regular training sessions for all personnel involved in the trial.
This training should cover not only local regulations but also international guidelines such as Good Clinical Practice (GCP). Additionally, employing dedicated regulatory affairs professionals can help ensure that all aspects of the trial adhere to applicable laws and guidelines. These experts can assist in preparing necessary documentation for regulatory submissions and provide ongoing support throughout the trial’s duration.
By fostering a culture of compliance within the site management team, organizations can mitigate risks associated with non-compliance while enhancing their reputation within the research community.
Enhancing Communication and Collaboration Among Site Staff and Sponsors
Effective communication and collaboration between site staff and sponsors are essential for the smooth operation of clinical trials. Establishing clear lines of communication from the outset helps prevent misunderstandings that could lead to delays or errors in protocol implementation. Regular meetings—whether virtual or in-person—can facilitate open dialogue about study progress, challenges encountered, and potential solutions.
Moreover, fostering a collaborative environment encourages site staff to voice concerns or suggestions regarding study procedures. When site personnel feel empowered to contribute their insights, it not only enhances morale but also leads to more innovative solutions to common challenges faced during trials. Utilizing collaborative tools such as shared project management software can further streamline communication by providing a centralized platform for tracking tasks, deadlines, and responsibilities.
Measuring and Monitoring Site Performance for Continuous Improvement
To ensure continuous improvement in clinical trial site management, it is crucial to implement robust performance measurement systems. Key performance indicators (KPIs) should be established to evaluate various aspects of site operations, including patient enrollment rates, data quality metrics, and compliance adherence. Regularly reviewing these KPIs allows sponsors to identify areas where sites excel as well as areas needing improvement.
In addition to quantitative metrics, qualitative feedback from site staff can provide valuable insights into operational challenges or inefficiencies. Conducting post-trial evaluations that include input from all stakeholders helps create a comprehensive understanding of what worked well and what could be improved in future studies. By fostering a culture of continuous improvement through regular monitoring and feedback loops, organizations can enhance their site management practices over time, ultimately leading to more successful clinical trials.