Clinical trial supply chain management is a critical component in the successful execution of pharmaceutical and biotechnology research. It encompasses the complex logistics and processes involved in ensuring that investigational medicinal products (IMPs) and associated materials are available at the right place, at the right time, and in the right quantity throughout the trial lifecycle. Optimizing this process is not merely about efficiency; it is fundamental to the integrity of clinical data, patient safety, and the overall cost-effectiveness of drug development. A poorly managed supply chain can lead to stalled trials, wasted resources, inaccurate results, and ultimately, delays in bringing life-saving treatments to market.
Accurate demand forecasting is the bedrock of effective clinical trial supply management. It involves predicting the precise quantities of IMPs and ancillary supplies needed at each study site, for each patient, over the entire duration of the trial. This is not a static calculation; it’s a dynamic process that requires constant refinement based on evolving trial parameters.
Patient Enrollment and Retention
The number of patients enrolled and their retention rate are direct drivers of supply needs. Underestimating enrollment leads to shortages, while overestimating can result in costly overproduction and wastage. Similarly, a high patient dropout rate means less IMP will be consumed than initially planned, creating a surplus. Real-time tracking of enrollment and proactive strategies to improve patient retention are therefore paramount. For instance, robust patient support programs can act as a strong anchor, keeping patients engaged in the trial and thus ensuring predictable IMP consumption.
Protocol Amendments and Changes
Clinical trial protocols are rarely set in stone. Amendments, whether driven by emerging scientific understanding, regulatory feedback, or operational challenges, can significantly impact supply requirements. A change in the dosage, frequency, or duration of treatment necessitates a recalibration of demand forecasts. Failing to adapt quickly to these changes can lead to either an immediate shortage of the revised IMP or an excess of the obsolete formulation. Therefore, a flexible forecasting system that can readily incorporate protocol amendments is essential.
Site-Specific Considerations
Each clinical trial site operates within its own unique environment. Factors such as local prescribing habits, investigator experience, patient demographics, and logistical capabilities at the site can influence IMP consumption. A one-size-fits-all approach to forecasting is therefore inadequate. Instead, demand planning must be granular, accounting for the specific nuances of each participating site. This might involve using historical data from similar trials conducted at those sites or collaborating closely with site investigators to understand their specific patient populations and how they might interact with the study protocol.
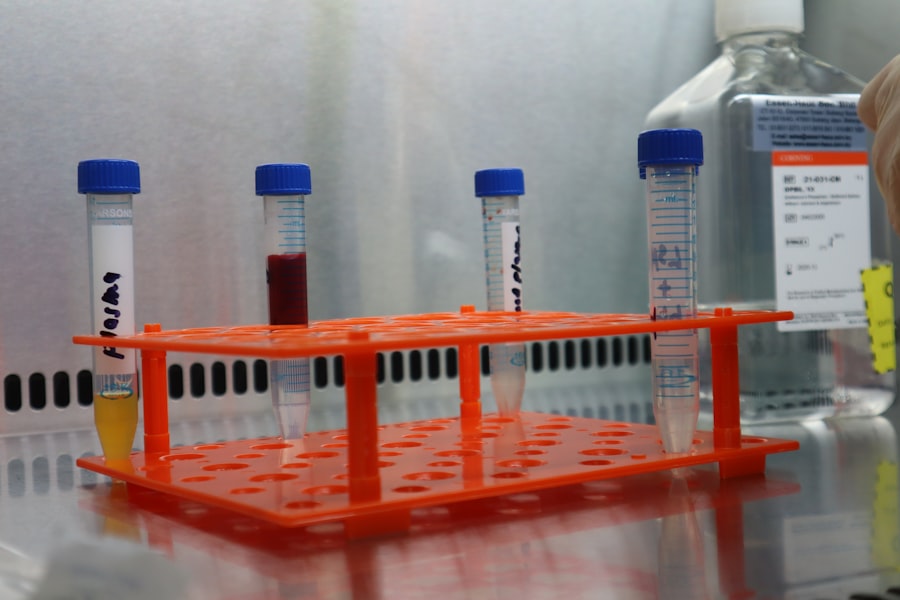
Inventory Management and Control
Once supplies are manufactured and distributed, their effective management within the supply chain becomes critical. Inventory control aims to minimize holding costs, prevent stockouts, and mitigate the risk of product expiry or spoilage. It requires a disciplined approach to tracking, storing, and allocating materials.
Just-in-Time (JIT) vs. Just-in-Case (JIC) Strategies
The debate between JIT and JIC strategies is a recurring theme in supply chain management. A JIT approach aims to have materials arrive precisely when they are needed, minimizing inventory levels. In clinical trials, this can be highly efficient, reducing the risk of expiry. However, it is also susceptible to disruptions in the supply chain, which could lead to critical shortages. A JIC approach, conversely, involves holding larger buffer stocks to guard against unforeseen events. While this offers greater security, it increases warehousing costs, the risk of obsolescence, and the capital tied up in inventory. The optimal strategy often involves a hybrid approach, applying JIT principles where predictability is high and JIC for critical or long-lead-time items.
Expiry Date Management
Expiring IMPs represent a direct financial loss and a potential disruption to patient treatment. Rigorous monitoring of expiry dates throughout the supply chain is therefore non-negotiable. This includes tracking expiry dates for materials at central depots, in transit, and at the clinical trial sites. Implementing a first-expired, first-out (FEFO) inventory system is a standard practice here, ensuring that older stock is used before newer stock. Regular audits and clear communication channels with sites regarding upcoming expiry dates are vital to prevent wastage.
Cold Chain Integrity
Many IMPs require strict temperature control to maintain their efficacy and safety. This “cold chain” extends from the point of manufacture through storage, transportation, and ultimately administration to the patient. Maintaining cold chain integrity throughout this complex journey is a logistical feat akin to navigating a treacherous river, where any rupture in the chain can compromise the entire cargo. Specialized packaging, temperature monitoring devices, and validated shipping routes are essential. Any deviation from the required temperature range must be meticulously documented and assessed for its impact on product quality.
Distribution and Logistics
The physical movement of IMPs and ancillary supplies from the manufacturer to the clinical trial sites is a complex undertaking. This phase requires meticulous planning and execution to ensure timely and secure delivery.
Global Distribution Networks
Clinical trials are increasingly global, involving sites across multiple countries. Managing distribution across diverse geographical regions introduces a multitude of challenges, including varying customs regulations, import/export restrictions, and differing transportation infrastructures. Establishing a robust global distribution network requires partnerships with experienced logistics providers who understand the intricacies of international pharmaceutical shipments. This network acts as the circulatory system of the supply chain, delivering vital “nutrients” (IMPs) to where they are needed.
Temperature-Controlled Transportation
As mentioned previously, maintaining the cold chain during transportation is paramount for many IMPs. This necessitates the use of refrigerated vehicles, insulated containers, and specialized shipping methods. The selection of transport partners must prioritize those with proven cold chain capabilities and a strong track record in pharmaceutical logistics. Real-time temperature monitoring during transit provides crucial data to ensure the integrity of the shipment and allows for immediate intervention if any deviations occur.
Returns and Destruction Management
After their use in a trial, unused IMPs, sometimes referred to as “returns,” must be managed appropriately. This can involve returning them to a central depot for reconciliation, re-labeling for subsequent trials (if applicable and compliant with regulations), or secure destruction. Proper documentation of every return and destruction is critical for regulatory compliance and financial accountability. A well-defined process for returns and destruction prevents potential diversion, ensures accountability, and minimizes environmental impact.
Technology and Data Management

The effective management of clinical trial supplies is heavily reliant on robust technological solutions and meticulous data management practices. Technology acts as the nervous system, collecting, processing, and disseminating vital information to guide decision-making.
Interactive Response Technology (IRT) / Interactive Web Response System (IWRS)
IRT or IWRS systems are digital platforms that play a central role in automating and controlling the dispensing of IMPs at clinical trial sites. These systems manage patient randomization, drug allocation, and drug accountability, ensuring the correct IMP is given to the correct patient at the correct time. They act as the conductor of an orchestra, ensuring each instrument (site, patient, drug) plays in harmony. Real-time data generated by these systems provides invaluable insights into drug consumption, site performance, and potential supply chain bottlenecks.
Supply Chain Visibility Platforms
End-to-end supply chain visibility platforms provide a comprehensive overview of IMPs and ancillary supplies as they move through the various stages of the supply chain. These platforms integrate data from multiple sources, offering real-time tracking of inventory levels, shipment status, and potential risks. This enhanced visibility allows for proactive problem-solving rather than reactive crisis management. Imagine having a live map of all your critical shipments; this is the power of visibility platforms.
Data Analytics and Reporting
The vast amounts of data generated throughout the clinical trial supply chain are a goldmine of information. Advanced data analytics and reporting tools can transform this raw data into actionable insights. By analyzing trends in enrollment, consumption patterns, and logistical performance, sponsors can identify areas for optimization, refine forecasting models, and improve the overall efficiency and effectiveness of their supply chain. This is akin to an experienced navigator using charts and instruments to chart the best course.
Risk Management and Mitigation
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Inventory Accuracy | Percentage of clinical trial supplies accurately tracked in the system | 95% – 99% | High |
| Order Fulfillment Time | Average time taken to fulfill supply orders from request to delivery | 1 – 3 days | High |
| Supply Wastage Rate | Percentage of clinical supplies wasted due to expiry, damage, or mismanagement | 1% – 5% | Medium |
| Temperature Excursion Incidents | Number of times supplies were exposed to out-of-range temperatures | 0 – 2 per trial | High |
| Cycle Time for Resupply | Time taken to replenish supplies once stock reaches reorder level | 2 – 5 days | High |
| Compliance Rate | Percentage of supply management activities compliant with regulatory standards | 98% – 100% | Critical |
| System Downtime | Amount of time the supply management system is unavailable | Medium | |
| Forecast Accuracy | Accuracy of supply demand forecasting compared to actual usage | 85% – 95% | High |
The clinical trial supply chain is inherently susceptible to various risks, from natural disasters and geopolitical instability to supplier failures and quality issues. Proactive risk management and the development of mitigation strategies are therefore not an option but a necessity.
Supplier Qualification and Management
The reliability of suppliers, from IMP manufacturers to logistics providers, is a cornerstone of a stable supply chain. A rigorous supplier qualification process, including audits and performance monitoring, is essential. Establishing strong relationships with trusted suppliers and having contingency plans for supplier disruptions are crucial mitigation strategies. These suppliers are the trusted artisans who craft and deliver the tools for scientific discovery.
Business Continuity Planning (BCP)
BCP is designed to ensure that an organization can continue to operate in the face of disruptions. For clinical trial supply chains, this involves developing detailed plans for various scenarios, such as natural disasters, pandemics, or unexpected manufacturing issues. These plans should outline alternative sourcing strategies, emergency distribution routes, and communication protocols to minimize the impact on trial continuity and patient safety. A BCP is like a well-rehearsed emergency drill, ensuring that when the unexpected happens, the team knows exactly what to do.
Quality Control and Assurance
Maintaining the quality and integrity of IMPs throughout the supply chain is paramount for patient safety and data validity. Robust quality control measures at every stage, from manufacturing to storage and distribution, are essential. This includes adherence to Good Manufacturing Practices (GMPs) and Good Distribution Practices (GDPs). Regular quality audits and a clear process for investigating and addressing any quality deviations are critical for mitigating risks associated with product quality. The unwavering commitment to quality is the shield that protects the integrity of the entire endeavor.



