Phase three clinical trials represent a critical juncture in the drug development process, serving as a bridge between the laboratory and the marketplace. These trials are typically conducted after a drug has successfully passed through phase one and phase two trials, which primarily focus on safety and preliminary efficacy. In phase three, the emphasis shifts to evaluating the drug’s effectiveness in a larger population, often involving thousands of participants across multiple sites.
This stage is essential for gathering comprehensive data that can inform regulatory decisions and ultimately determine whether a new treatment can be made available to the public. The significance of phase three trials cannot be overstated. They are designed to confirm the findings from earlier phases, providing a more definitive assessment of a drug’s therapeutic benefits and risks.
The results from these trials are pivotal not only for regulatory agencies like the U.S. Food and Drug Administration (FDA) but also for healthcare providers and patients who rely on evidence-based information to make informed decisions about treatment options. As such, phase three trials are often seen as the final hurdle before a new drug can enter the market, making them a focal point of interest for pharmaceutical companies, researchers, and regulatory bodies alike.
Key Takeaways
- Phase Three trials confirm a treatment’s safety and effectiveness in large patient groups.
- They aim to compare new treatments against current standards to establish benefits and risks.
- Careful participant recruitment and informed consent ensure ethical study conduct.
- Rigorous study design and data analysis are critical for reliable and valid results.
- Successful trials support regulatory approval and influence future medical practices.
Purpose and Goals of Phase Three Clinical Trials
The primary purpose of phase three clinical trials is to assess the efficacy of a new treatment compared to existing therapies or a placebo. This is achieved through randomized controlled trials (RCTs), which are considered the gold standard in clinical research. By randomly assigning participants to different treatment groups, researchers can minimize biases and ensure that the results are attributable to the intervention being tested rather than external factors.
The goal is to provide robust evidence that demonstrates whether the new drug is effective in treating a specific condition or disease. In addition to efficacy, phase three trials also aim to gather extensive safety data. While earlier phases may have identified some adverse effects, phase three trials involve a larger and more diverse population, which can reveal rare side effects that may not have been apparent in smaller studies.
This comprehensive safety evaluation is crucial for understanding the risk-benefit profile of the drug. Furthermore, phase three trials often explore various subgroups within the population, such as different age groups, genders, or those with comorbid conditions, to determine if the drug’s efficacy and safety profile varies among these groups.
Participant Recruitment and Informed Consent

Recruiting participants for phase three clinical trials is a complex process that requires careful planning and execution. Researchers must identify suitable candidates who meet specific inclusion and exclusion criteria defined by the study protocol. These criteria ensure that the trial population is representative of the broader patient population that will ultimately use the drug if it receives approval.
Recruitment strategies may include outreach through healthcare providers, advertisements in medical journals, or community engagement initiatives to raise awareness about the trial. Informed consent is a fundamental ethical requirement in clinical research, particularly in phase three trials where participants may be exposed to new treatments with unknown long-term effects. Before enrolling in a trial, potential participants must be provided with comprehensive information about the study’s purpose, procedures, potential risks, and benefits.
This process ensures that individuals can make an informed decision about their participation. Researchers must also emphasize that participation is voluntary and that individuals can withdraw from the study at any time without any repercussions on their standard medical care.
Study Design and Implementation
| Metric | Description | Typical Values | Importance |
|---|---|---|---|
| Sample Size | Number of participants or units included in the study | 30 – 1000+ | Determines statistical power and generalizability |
| Randomization Method | Technique used to assign participants to groups | Simple, Stratified, Block, Cluster | Reduces selection bias and confounding |
| Blinding | Whether participants, researchers, or assessors are unaware of group assignments | None, Single, Double, Triple | Minimizes bias in treatment and assessment |
| Study Duration | Length of time over which the study is conducted | Weeks to Years | Impacts ability to observe outcomes and effects |
| Data Collection Frequency | How often data is collected from participants | Daily, Weekly, Monthly, At specific milestones | Affects data resolution and participant burden |
| Primary Outcome Measure | Main variable used to assess the effect of the intervention | Depends on study objective (e.g., blood pressure, survival rate) | Focuses analysis and interpretation |
| Compliance Rate | Percentage of participants adhering to the study protocol | 70% – 100% | Influences validity of results |
| Dropout Rate | Percentage of participants who leave the study before completion | 0% – 30% | Impacts study power and bias |
The design of phase three clinical trials is meticulously crafted to address specific research questions while adhering to regulatory standards. Most commonly, these trials utilize a randomized controlled design, which allows for direct comparisons between the new treatment and either a placebo or an active comparator. This design helps eliminate confounding variables that could skew results.
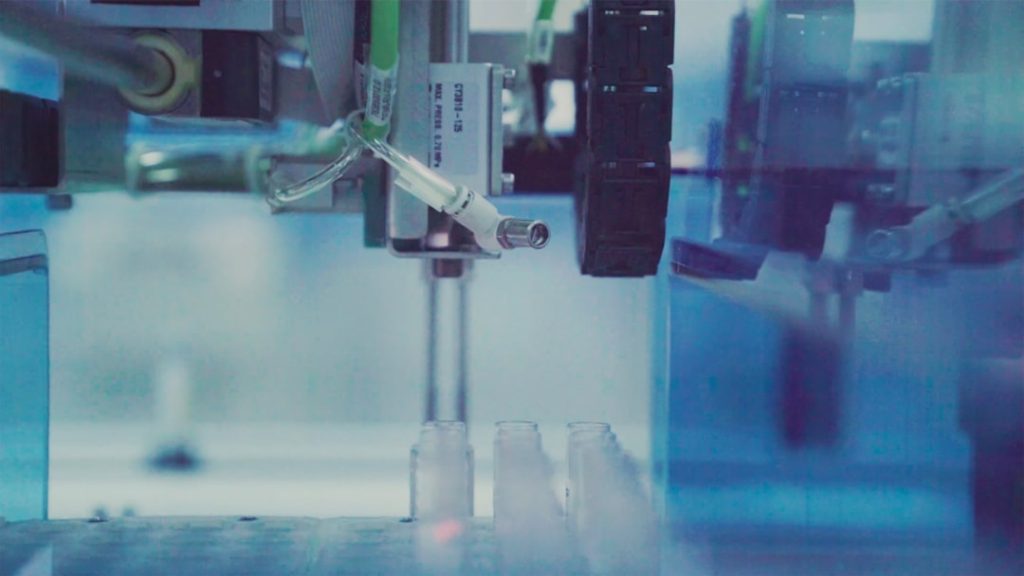
Additionally, many phase three trials are double-blinded, meaning neither the participants nor the researchers know who is receiving which treatment until the study concludes. This blinding helps reduce bias in reporting outcomes. Implementation of phase three trials involves rigorous adherence to protocols established during the planning phase.
This includes training investigators and site staff on study procedures, ensuring compliance with Good Clinical Practice (GCP) guidelines, and maintaining meticulous records of participant data. Monitoring is also a critical component during this phase; independent data monitoring committees (DMCs) may be established to oversee trial progress and ensure participant safety. These committees can recommend modifications or even halt a trial if significant safety concerns arise or if interim results indicate that the treatment is either highly effective or ineffective.
Data Collection and Analysis
Data collection in phase three clinical trials is systematic and comprehensive, focusing on both primary and secondary endpoints defined in the study protocol. Primary endpoints typically relate directly to the drug’s efficacy—such as improvement in symptoms or survival rates—while secondary endpoints may include quality of life measures or additional safety assessments. Data collection methods can vary widely, including patient-reported outcomes, laboratory tests, imaging studies, and clinician assessments.
Once data collection is complete, rigorous statistical analysis is conducted to interpret the results. This analysis often involves comparing outcomes between treatment groups using various statistical methods to determine whether observed differences are statistically significant. Researchers must also account for potential confounding factors that could influence results, such as baseline characteristics of participants or variations in treatment adherence.
The integrity of data analysis is paramount; thus, many trials employ independent statisticians who are not involved in the trial’s conduct to ensure objectivity.
Safety and Efficacy Evaluation
The evaluation of safety and efficacy during phase three clinical trials is multifaceted and ongoing throughout the study’s duration. Safety monitoring is particularly crucial as larger participant populations may reveal adverse effects that were not evident in earlier phases. Adverse events must be meticulously documented and analyzed to assess their frequency and severity in relation to the treatment being tested.
Researchers often employ predefined criteria for classifying adverse events, which helps standardize reporting across different sites. Efficacy evaluation goes beyond simply determining whether a drug works; it also involves understanding how well it works compared to existing treatments or placebos. This comparative effectiveness research is vital for informing clinical practice guidelines and ensuring that healthcare providers have access to evidence-based recommendations when choosing treatments for their patients.
Additionally, subgroup analyses can provide insights into how different populations respond to treatment, which can be particularly important for tailoring therapies to individual patient needs.
Regulatory Approval and Market Access
Upon completion of phase three trials, researchers compile their findings into a comprehensive report that forms part of a New Drug Application (NDA) submitted to regulatory agencies such as the FDA or European Medicines Agency (EMA). This application includes detailed information about the trial design, methodology, results, and proposed labeling for the drug. Regulatory agencies rigorously review this data to assess whether the benefits of the drug outweigh its risks before granting approval for market access.
The regulatory approval process can be lengthy and complex, often involving multiple rounds of questions from agency reviewers seeking clarification on various aspects of the trial data. In some cases, advisory committees may be convened to provide expert opinions on specific issues related to safety or efficacy before a final decision is made. Once approved, pharmaceutical companies must also navigate post-marketing surveillance requirements to monitor long-term safety and effectiveness in the general population.
Future Implications and Considerations
The landscape of phase three clinical trials is continually evolving due to advancements in technology, regulatory frameworks, and patient engagement strategies. One significant trend is the increasing use of adaptive trial designs, which allow for modifications to be made during the trial based on interim results without compromising scientific integrity. This flexibility can lead to more efficient trials that can bring effective treatments to market more quickly.
Moreover, there is a growing emphasis on patient-centered approaches in clinical research. Engaging patients in trial design and implementation can enhance recruitment efforts and improve retention rates while ensuring that studies address real-world concerns relevant to patients’ lives. As healthcare becomes increasingly personalized, future phase three trials may focus more on specific biomarkers or genetic profiles to tailor treatments to individual patients’ needs.
In conclusion, phase three clinical trials play an indispensable role in bringing new therapies from concept to reality. They provide critical evidence needed for regulatory approval while ensuring that patient safety remains at the forefront of medical research. As methodologies continue to advance and patient engagement becomes more integral to trial design, these studies will likely evolve further, paving the way for innovative treatments that meet the diverse needs of patients worldwide.