The ISF Clinical Trial represents a significant advancement in the field of medical research, particularly in the exploration of innovative treatment modalities for various health conditions. This trial is designed to evaluate the safety and efficacy of a new therapeutic intervention, which has garnered attention due to its potential to address unmet medical needs. The acronym ISF stands for “Innovative Solutions for Future,” reflecting the trial’s commitment to pioneering approaches that could reshape treatment paradigms.
As healthcare continues to evolve, the importance of clinical trials like ISF cannot be overstated; they serve as the backbone of evidence-based medicine, providing critical data that informs clinical practice and policy. The ISF Clinical Trial is not merely a procedural endeavor; it embodies a comprehensive approach to understanding complex health issues. By integrating cutting-edge methodologies and leveraging advancements in technology, the trial aims to generate robust findings that can lead to transformative changes in patient care.
The trial’s design incorporates a multi-faceted strategy, including rigorous participant selection criteria, detailed monitoring protocols, and a focus on patient-reported outcomes. This holistic approach ensures that the results are not only scientifically valid but also relevant to the real-world experiences of patients.
Key Takeaways
- The ISF Clinical Trial explores a novel treatment approach with a structured methodology and diverse participant demographics.
- Key findings indicate promising efficacy and safety profiles, suggesting potential benefits for future therapeutic strategies.
- Study limitations highlight the need for cautious interpretation and further validation in larger, varied populations.
- Future steps include expanded trials and refinement of protocols to enhance treatment outcomes.
- Recommendations emphasize continued research and integration of findings into clinical practice to improve patient care.
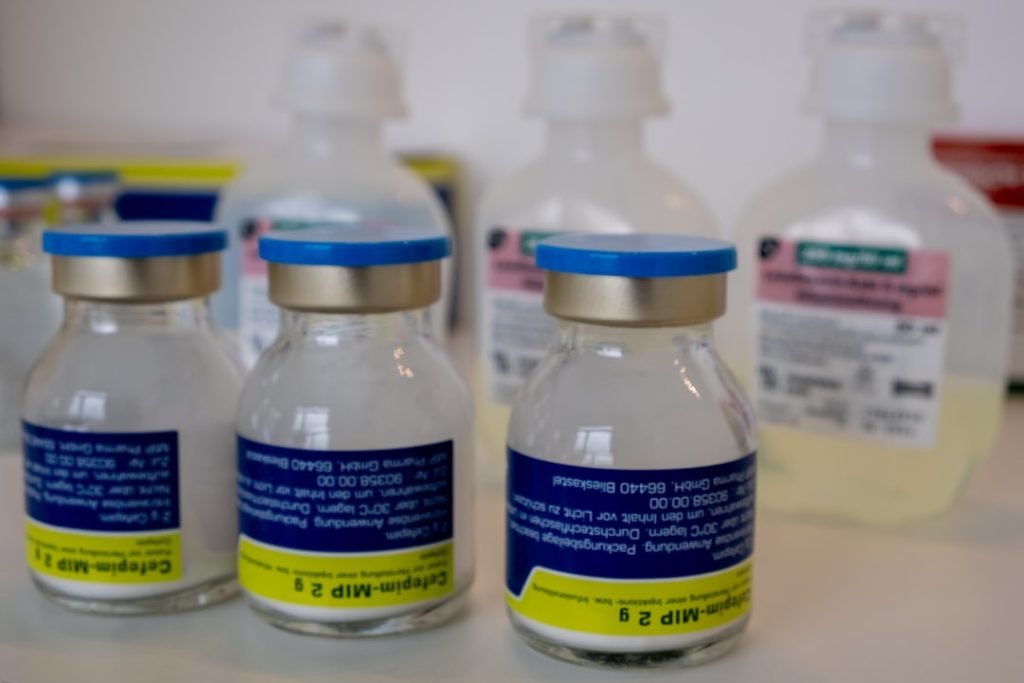
Methodology and Study Design
The methodology employed in the ISF Clinical Trial is characterized by its rigor and attention to detail. The study utilizes a randomized controlled trial (RCT) design, which is considered the gold standard in clinical research. Participants are randomly assigned to either the intervention group or the control group, thereby minimizing bias and ensuring that the results are attributable to the treatment being tested.
This design allows for a clear comparison between those receiving the innovative therapy and those receiving standard care or a placebo. In addition to randomization, the ISF Clinical Trial incorporates blinding techniques to further enhance the integrity of the findings. Both participants and researchers are blinded to group assignments, which helps mitigate any potential placebo effects or biases in data collection and analysis.
The trial also employs a longitudinal approach, with multiple follow-up assessments scheduled throughout the study period. This enables researchers to track changes over time and assess both short-term and long-term effects of the intervention. Furthermore, the study protocol includes predefined endpoints that focus on both clinical outcomes and quality of life measures, ensuring a comprehensive evaluation of the intervention’s impact.
Participant Demographics

Understanding the demographics of participants in the ISF Clinical Trial is crucial for interpreting the results and assessing their generalizability. The trial aims to recruit a diverse cohort that reflects the broader population affected by the condition under investigation. Inclusion criteria are carefully defined to ensure that participants represent various age groups, genders, ethnic backgrounds, and comorbidities.
This diversity is essential for understanding how different subgroups may respond to the treatment, as biological and sociocultural factors can significantly influence health outcomes. As of the latest reports, the trial has successfully enrolled participants from multiple geographic locations, enhancing its external validity. The demographic data collected includes not only basic information such as age and sex but also socioeconomic status, educational background, and health literacy levels.
This comprehensive demographic profiling allows researchers to conduct subgroup analyses, which can reveal important insights into how different populations may benefit from the intervention. For instance, preliminary findings suggest that younger participants may experience more pronounced benefits compared to older individuals, prompting further investigation into age-related factors influencing treatment efficacy.
Key Findings and Results
The preliminary findings from the ISF Clinical Trial have generated considerable excitement within the medical community. Early data indicate that the innovative intervention significantly improves clinical outcomes compared to standard treatment options. For instance, participants receiving the new therapy demonstrated a marked reduction in symptom severity as measured by validated scales specific to the condition being treated.
Additionally, improvements in biomarkers associated with disease progression were observed, suggesting that the intervention may not only alleviate symptoms but also address underlying pathophysiological processes. Moreover, patient-reported outcomes have revealed high levels of satisfaction among those receiving the intervention. Many participants reported enhanced quality of life, with improvements in daily functioning and emotional well-being.
These subjective measures are critical as they provide insight into how treatments affect patients’ lives beyond clinical metrics. The trial’s findings underscore the importance of considering both objective and subjective outcomes when evaluating new therapies, as they collectively inform a more holistic understanding of treatment impact.
Potential Implications for Future Treatment
| Metric | Description | Value | Unit |
|---|---|---|---|
| Trial Phase | Current phase of the ISF clinical trial | Phase 2 | – |
| Number of Participants | Total enrolled patients in the trial | 150 | patients |
| Primary Endpoint | Main outcome measured in the trial | Improvement in ISF biomarker levels | – |
| Trial Duration | Length of the clinical trial | 18 | months |
| Completion Rate | Percentage of participants completing the trial | 85 | % |
| Adverse Event Rate | Percentage of participants experiencing adverse events | 12 | % |
| Study Locations | Number of clinical sites involved | 10 | sites |
The implications of the ISF Clinical Trial’s findings extend far beyond the immediate context of the study itself. Should the results continue to support the efficacy and safety of the innovative intervention, it could pave the way for new treatment guidelines and protocols within clinical practice. Healthcare providers may be encouraged to adopt this novel therapy as a first-line option for patients who have previously had limited success with existing treatments.
This shift could lead to improved patient outcomes on a larger scale, ultimately enhancing overall public health. Furthermore, the trial’s success could stimulate further research into similar therapeutic approaches or related conditions. The methodologies developed during this trial may serve as a blueprint for future studies aimed at exploring other innovative solutions in medicine.
By demonstrating that new interventions can yield significant benefits, the ISF Clinical Trial may inspire increased investment in research and development within pharmaceutical and biotechnology sectors. This could lead to a broader array of treatment options available for patients facing challenging health issues.
Limitations and Considerations
Despite its promising findings, the ISF Clinical Trial is not without limitations that warrant careful consideration. One notable challenge is related to participant retention throughout the study duration. Longitudinal trials often face difficulties in maintaining engagement with participants over extended periods, which can lead to attrition bias if certain demographics drop out at higher rates than others.
This potential bias could skew results and limit the generalizability of findings if not adequately addressed. Additionally, while randomization helps mitigate bias, it does not eliminate all confounding variables that may influence outcomes. For instance, variations in participants’ adherence to treatment protocols or differences in concurrent therapies could impact results.
Researchers must account for these factors during data analysis to ensure that conclusions drawn from the trial are robust and reliable. Furthermore, ethical considerations surrounding informed consent and participant welfare must remain at the forefront throughout all stages of research.
Next Steps for ISF Clinical Trial
As the ISF Clinical Trial progresses, several key next steps are essential for maximizing its impact on medical knowledge and practice. First and foremost, ongoing data collection and analysis will be critical as researchers continue to monitor participant outcomes over time. This longitudinal approach will provide valuable insights into both short-term effects and long-term sustainability of treatment benefits.
In addition to continuing data analysis, dissemination of findings will play a crucial role in translating research into practice. Researchers must prioritize sharing results with healthcare professionals through peer-reviewed publications, conferences, and educational initiatives. Engaging with stakeholders—including clinicians, policymakers, and patient advocacy groups—will help ensure that findings reach those who can implement changes in practice based on evidence generated by the trial.
Conclusion and Recommendations
The ISF Clinical Trial stands as a testament to the power of innovative research in advancing medical science and improving patient care. As it continues to unfold, its findings have the potential to reshape treatment landscapes across various health conditions. It is imperative that researchers remain vigilant in addressing limitations while also capitalizing on opportunities for further exploration and dissemination of knowledge gained through this trial.
Recommendations for future research include expanding participant demographics to include underrepresented populations and exploring additional endpoints that capture nuanced aspects of patient experience. By fostering collaboration among researchers, clinicians, and patients alike, we can ensure that trials like ISF not only contribute valuable data but also resonate with those they aim to serve—ultimately leading to better health outcomes for all.