Clinical trials are structured research studies conducted to evaluate the safety and efficacy of new medical interventions, including drugs, devices, and treatment protocols. These trials are essential components of the medical research process, designed to gather data that can lead to new therapies or improve existing ones. They typically involve human participants and are conducted in a controlled environment to ensure that the results are reliable and valid.
The primary goal of clinical trials is to determine whether a new treatment is more effective than the current standard of care or to assess its safety profile. The design of clinical trials can vary significantly depending on the objectives of the study. Some trials may focus on a specific disease or condition, while others may explore broader health issues.
They can be randomized, where participants are assigned to different treatment groups by chance, or observational, where researchers observe outcomes without assigning specific treatments. The rigorous methodology employed in clinical trials is crucial for generating evidence that can inform clinical practice and regulatory decisions.
Key Takeaways
- Clinical trials are research studies that test new medical treatments or interventions on volunteers.
- They are essential for developing safe and effective medications and improving healthcare.
- Participants can include healthy volunteers or patients meeting specific criteria.
- Clinical trials progress through phases I to IV, each with distinct goals and methods.
- Informed consent ensures participants understand risks, benefits, and their rights before joining a trial.
Why are Clinical Trials Important?
Clinical trials play a pivotal role in advancing medical knowledge and improving patient care. They are the cornerstone of evidence-based medicine, providing the data necessary to support new treatment options and therapeutic strategies. By rigorously testing new interventions, clinical trials help ensure that only safe and effective treatments reach the market.
This process not only protects patients but also fosters innovation in healthcare, as researchers can explore novel approaches to disease management. Moreover, clinical trials contribute to the understanding of disease mechanisms and patient responses to treatment. For instance, they can reveal how genetic variations influence drug metabolism or how comorbidities affect treatment outcomes.
This information is invaluable for developing personalized medicine approaches, where treatments can be tailored to individual patient profiles. The insights gained from clinical trials can lead to breakthroughs that transform the standard of care for various conditions, ultimately improving health outcomes on a population level.
Who can Participate in Clinical Trials?
Participation in clinical trials is typically open to a diverse range of individuals, but eligibility criteria can vary widely depending on the specific study. Generally, participants must meet certain inclusion and exclusion criteria that are established by the researchers to ensure that the trial results are applicable to the target population. Inclusion criteria may include specific age ranges, gender, disease stage, or other health conditions, while exclusion criteria might disqualify individuals with certain comorbidities or those taking specific medications.
Recruitment strategies for clinical trials often aim to reach a broad demographic to ensure that findings are generalizable across different populations. This diversity is crucial for understanding how various factors—such as age, ethnicity, and socioeconomic status—can influence treatment efficacy and safety. Additionally, some trials may specifically seek participants from underrepresented groups to address disparities in healthcare access and outcomes.
Engaging a wide array of participants not only enriches the data collected but also enhances the relevance of the findings to real-world clinical practice.
The Phases of Clinical Trials
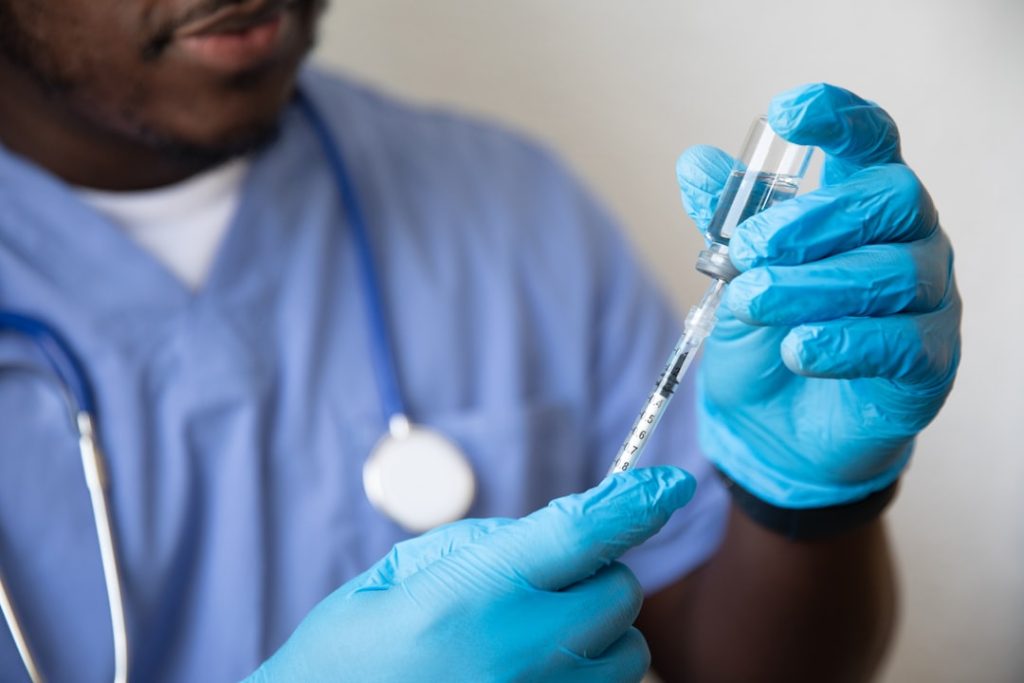
Clinical trials are typically conducted in a series of phases, each with distinct objectives and methodologies. Phase I trials primarily focus on assessing the safety and tolerability of a new intervention in a small group of healthy volunteers or patients. Researchers monitor participants closely for adverse effects and determine appropriate dosage levels.
This phase is crucial for identifying any potential risks associated with the treatment before it is tested in larger populations. Phase II trials expand the participant pool and aim to evaluate the efficacy of the intervention while continuing to monitor safety. These studies often involve patients who have the condition that the treatment is intended to address.
Researchers gather preliminary data on how well the treatment works and may explore different dosages or treatment regimens. If Phase II results are promising, the trial progresses to Phase III, which involves larger groups of participants across multiple sites. Phase III trials are designed to confirm efficacy, monitor side effects more comprehensively, and compare the new treatment against standard therapies.
Successful completion of these phases is essential for obtaining regulatory approval from agencies such as the U.S. Food and Drug Administration (FDA).
Risks and Benefits of Participating in Clinical Trials
| Aspect | Description | Example Metrics |
|---|---|---|
| Definition | Research studies performed in people that are aimed at evaluating a medical, surgical, or behavioral intervention. | N/A |
| Phases | Stages of clinical trials to test safety, efficacy, dosage, and side effects. |
Phase 1: 20-100 participants Phase 2: 100-300 participants Phase 3: 1,000-3,000 participants Phase 4: Post-marketing surveillance |
| Purpose | To determine if new treatments are safe and effective. | Success rate: ~70% of drugs pass Phase 3 |
| Duration | Time taken to complete each phase varies. |
Phase 1: Several months Phase 2: Several months to 2 years Phase 3: 1-4 years Phase 4: Ongoing |
| Participants | Individuals who volunteer to take part in the study. | Enrollment numbers vary by trial size and phase |
| Regulatory Oversight | Monitored by agencies like FDA, EMA to ensure safety and ethics. | Approval required before moving to next phase |
Participating in clinical trials comes with both potential risks and benefits that individuals must carefully consider before enrolling. On one hand, participants may gain access to cutting-edge treatments that are not yet available to the general public. This access can be particularly valuable for patients with conditions that have limited treatment options or for those who have exhausted standard therapies.
Additionally, participants often receive close medical supervision and monitoring throughout the trial, which can lead to improved health outcomes. However, there are inherent risks associated with clinical trial participation. New treatments may have unknown side effects or may not be effective for all individuals.
Participants may experience adverse reactions that were not identified during earlier phases of testing. Furthermore, there is no guarantee that the experimental treatment will provide any benefit compared to existing therapies. It is essential for potential participants to weigh these risks against the potential benefits and to engage in open discussions with their healthcare providers about their options.
Informed Consent in Clinical Trials

Informed consent is a fundamental ethical requirement in clinical trials, ensuring that participants understand what their involvement entails before agreeing to participate. The informed consent process involves providing potential participants with comprehensive information about the study’s purpose, procedures, risks, benefits, and their rights as participants. This process is designed to empower individuals to make informed decisions about their participation based on a clear understanding of what is expected.
The informed consent document typically includes details about the study’s duration, any required visits or procedures, potential side effects, and contact information for study personnel. Researchers must ensure that participants comprehend this information and have an opportunity to ask questions before signing the consent form. It is important to note that consent is an ongoing process; participants should feel free to withdraw from the study at any time without penalty or loss of benefits related to their standard care.
How to Find and Join a Clinical Trial
Finding and joining a clinical trial can be a straightforward process if individuals know where to look and what steps to take. Numerous resources are available for those interested in participating in clinical research studies. Websites such as ClinicalTrials.gov provide comprehensive databases of ongoing clinical trials across various medical conditions and locations.
Users can search for studies based on specific criteria such as disease type, location, or phase of research. Once individuals identify a trial that interests them, they should reach out to the study coordinators or principal investigators for more information about eligibility requirements and enrollment procedures. Healthcare providers can also be valuable resources; they may have knowledge of ongoing trials relevant to their patients’ conditions or may even be involved in conducting research themselves.
Engaging with support groups or patient advocacy organizations can also provide insights into available clinical trials and help connect individuals with researchers.
The Future of Clinical Trials
The landscape of clinical trials is evolving rapidly due to advancements in technology and changes in regulatory frameworks. One significant trend is the increasing use of digital health technologies, such as mobile apps and wearable devices, which facilitate remote monitoring and data collection during trials. These innovations allow researchers to gather real-time data on patient outcomes while enhancing participant engagement through more convenient participation options.
Additionally, there is a growing emphasis on patient-centered approaches in clinical trial design. Researchers are increasingly involving patients in the planning stages of studies to ensure that trials address relevant questions and outcomes that matter most to them. This shift towards patient engagement not only improves recruitment efforts but also enhances the quality of data collected by aligning research objectives with patient needs.
As personalized medicine continues to gain traction, future clinical trials may focus more on targeted therapies based on genetic profiles or biomarkers rather than one-size-fits-all approaches. This shift could lead to more effective treatments with fewer side effects for specific patient populations. Overall, the future of clinical trials holds great promise for advancing medical science and improving healthcare delivery through innovative methodologies and a greater focus on patient involvement.