Clinical research is a vital component of the medical field, serving as the bridge between laboratory discoveries and practical applications in patient care. It encompasses a wide range of studies aimed at understanding health and disease, evaluating new treatments, and improving existing medical practices. The primary goal of clinical research is to generate evidence that can inform clinical decision-making, ultimately enhancing patient outcomes.
This research can take various forms, including clinical trials, observational studies, and epidemiological research, each contributing uniquely to the body of medical knowledge. The significance of clinical research cannot be overstated; it is the foundation upon which modern medicine is built. For instance, the development of vaccines, such as those for polio and measles, relied heavily on rigorous clinical trials to ensure safety and efficacy before public distribution.
Moreover, clinical research plays a crucial role in understanding the complexities of diseases, such as cancer and diabetes, leading to innovative treatment protocols and improved management strategies. As the healthcare landscape continues to evolve, the importance of robust clinical research remains paramount in addressing emerging health challenges and advancing medical science.
Key Takeaways
- Clinical research is essential for advancing medical knowledge and patient care.
- Ethical considerations, including informed consent, are critical to protect participant rights.
- Proper study design and rigorous data analysis ensure reliable and valid research outcomes.
- Regulatory compliance is mandatory to maintain research integrity and participant safety.
- Emerging technologies and methodologies are shaping the future of clinical research.
Ethical Considerations in Clinical Research
Ethical considerations are at the forefront of clinical research, ensuring that the rights and welfare of participants are protected throughout the study process. The principles of respect for persons, beneficence, and justice form the ethical framework guiding researchers. Respect for persons emphasizes the need for informed consent, allowing participants to make autonomous decisions regarding their involvement in research.
This principle is particularly crucial in vulnerable populations, where additional safeguards may be necessary to protect individuals from exploitation or harm. Beneficence requires researchers to maximize potential benefits while minimizing risks to participants. This principle is often operationalized through rigorous risk-benefit analyses conducted prior to study initiation.
For example, in a clinical trial evaluating a new cancer treatment, researchers must carefully weigh the potential therapeutic benefits against the risks of adverse side effects. Justice pertains to the equitable distribution of research burdens and benefits among different groups, ensuring that no particular population is unfairly targeted or excluded from participation. This principle has gained increased attention in recent years, particularly in light of historical injustices in medical research.
Designing a Clinical Research Study
The design of a clinical research study is a critical step that influences the validity and reliability of the findings. A well-structured study design begins with a clear research question that addresses a specific gap in knowledge or a pressing clinical issue. Researchers must decide on the type of study—be it interventional or observational—based on the objectives and hypotheses.
For instance, a randomized controlled trial (RCT) is often considered the gold standard for testing new interventions due to its ability to minimize bias through randomization. Once the study type is determined, researchers must develop a detailed protocol outlining the methodology, including participant selection criteria, sample size calculations, and data collection methods. The choice of endpoints—primary and secondary outcomes—also plays a crucial role in study design.
For example, in a trial assessing a new medication for hypertension, primary endpoints might include changes in blood pressure levels, while secondary endpoints could encompass quality of life measures or incidence of adverse events. Additionally, consideration must be given to statistical analysis plans to ensure that data will be interpreted correctly and meaningfully.
Data Collection and Analysis in Clinical Research
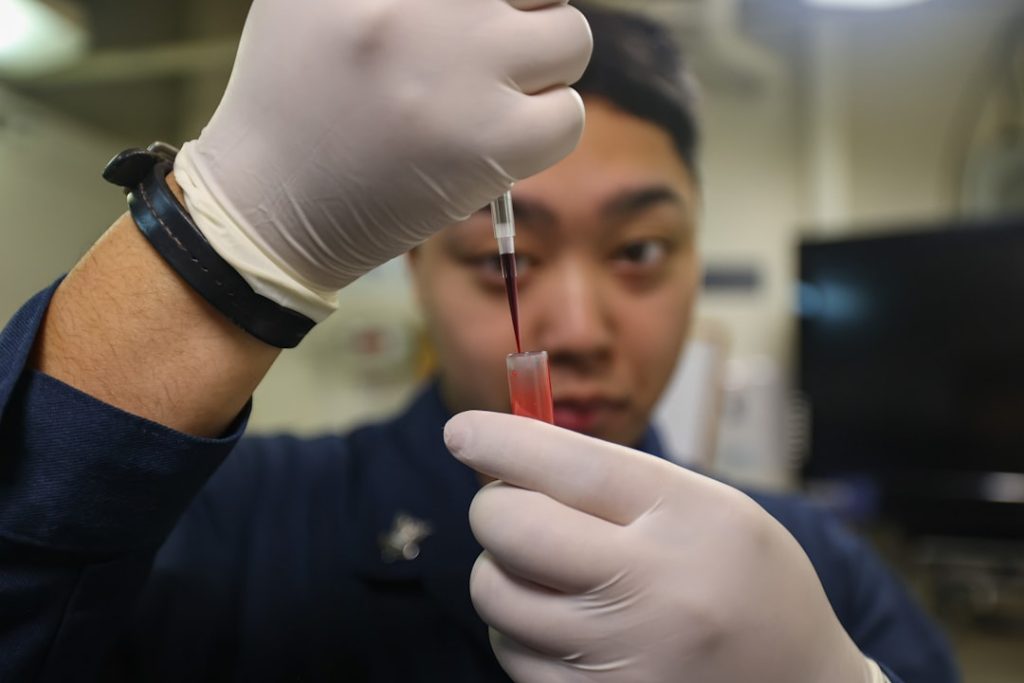
Data collection is a fundamental aspect of clinical research that directly impacts the integrity of study results. Researchers employ various methods for gathering data, including surveys, interviews, laboratory tests, and electronic health records. The choice of data collection method often depends on the study design and objectives.
For instance, in an observational study examining lifestyle factors affecting heart disease risk, researchers may utilize questionnaires to gather self-reported data on diet and physical activity levels. Once data is collected, rigorous analysis is essential to draw valid conclusions from the findings. Statistical methods are employed to interpret data accurately and assess relationships between variables.
For example, regression analysis may be used to determine whether there is a significant association between smoking and lung cancer incidence while controlling for confounding factors such as age and gender. Advanced techniques such as machine learning are increasingly being integrated into data analysis processes, allowing researchers to uncover complex patterns within large datasets that traditional methods may overlook.
Importance of Informed Consent in Clinical Research
| Metric | Description | Typical Value/Range | Importance in Clinical Research |
|---|---|---|---|
| Sample Size | Number of participants in a study | 30 – 1000+ | Determines statistical power and validity of results |
| Randomization | Process of assigning participants to groups by chance | Yes/No | Reduces bias and confounding variables |
| Blinding | Concealing group allocation from participants/investigators | Single, Double, or Triple Blind | Prevents bias in treatment administration and assessment |
| Control Group | Group receiving standard treatment or placebo | Present/Absent | Provides baseline for comparison |
| Primary Outcome | Main result measured to assess intervention effect | Varies by study | Focuses the study and guides analysis |
| Informed Consent Rate | Percentage of eligible participants who consent | 70% – 95% | Ensures ethical participation and compliance |
| Adverse Event Rate | Frequency of negative side effects reported | Varies widely | Monitors safety of interventions |
| Follow-up Rate | Percentage of participants completing the study | 80% – 100% | Ensures data completeness and reliability |
| Statistical Significance (p-value) | Probability that results are due to chance | < 0.05 | Determines if findings are likely true effects |
Informed consent is a cornerstone of ethical clinical research practice, ensuring that participants are fully aware of their rights and the nature of their involvement before agreeing to participate. The informed consent process involves providing potential participants with comprehensive information about the study’s purpose, procedures, risks, benefits, and alternatives. This transparency empowers individuals to make informed decisions about their participation based on their values and preferences.
Moreover, informed consent is not merely a one-time event but an ongoing dialogue throughout the study. Researchers must continually engage with participants to address any questions or concerns that may arise during the course of the research. This approach fosters trust between researchers and participants and reinforces the ethical commitment to respect individual autonomy.
In recent years, there has been a growing emphasis on enhancing informed consent processes through innovative approaches such as multimedia presentations or simplified consent forms tailored to diverse populations.
Regulatory Compliance in Clinical Research

Regulatory compliance is essential in clinical research to ensure that studies are conducted ethically and safely while adhering to established guidelines and standards. Various regulatory bodies oversee clinical research activities, including the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and institutional review boards (IRBs).
These organizations set forth regulations that govern aspects such as study design, participant safety monitoring, and reporting requirements. Compliance with Good Clinical Practice (GCP) guidelines is paramount for researchers conducting clinical trials. GCP encompasses principles that ensure the integrity of data collected during studies while safeguarding participant rights and welfare.
For instance, researchers must maintain accurate records of all study-related activities and ensure that any adverse events are reported promptly to regulatory authorities. Failure to comply with these regulations can result in severe consequences, including penalties for researchers or institutions and potential harm to participants.
Challenges in Conducting Clinical Research
Conducting clinical research presents numerous challenges that can impact study outcomes and timelines. One significant challenge is participant recruitment; finding eligible individuals who are willing to participate can be difficult due to various factors such as fear of side effects or lack of awareness about ongoing studies. For example, trials for rare diseases often struggle with recruitment due to limited patient populations.
Additionally, maintaining participant retention throughout the study duration poses another hurdle. Dropout rates can skew results and compromise the validity of findings. Researchers must implement strategies to enhance participant engagement and retention, such as regular follow-ups or providing incentives for continued participation.
Furthermore, logistical challenges related to data collection—such as coordinating multiple sites or managing large datasets—can complicate study execution and require careful planning and resource allocation.
Future Trends in Clinical Research
The landscape of clinical research is continuously evolving, driven by advancements in technology and changing societal needs. One notable trend is the increasing use of digital health technologies, including telemedicine and mobile health applications, which facilitate remote patient monitoring and data collection. These innovations not only enhance accessibility for participants but also allow for real-time data capture, improving the efficiency of studies.
Another emerging trend is the integration of artificial intelligence (AI) into clinical research processes. AI algorithms can analyze vast amounts of data quickly and accurately, identifying patterns that may inform treatment decisions or predict patient outcomes. Additionally, machine learning techniques are being utilized to optimize trial designs by predicting which patient populations are most likely to benefit from specific interventions.
Moreover, there is a growing emphasis on patient-centered research approaches that prioritize participant perspectives throughout the research process. Engaging patients as partners in research design and implementation can lead to more relevant outcomes and improve overall satisfaction with clinical trials. As these trends continue to shape the future of clinical research, they hold promise for enhancing the quality and impact of studies aimed at improving health outcomes worldwide.