Clinical trials represent the fundamental methodology for evaluating new medical treatments, pharmaceuticals, and devices in modern healthcare systems. These structured research studies generate evidence required for regulatory approval and clinical implementation through systematic assessment of safety and efficacy parameters. The development pathway from laboratory research to clinical application involves sequential trial phases, each designed to examine specific aspects of therapeutic interventions and establish comprehensive risk-benefit profiles.
Clinical trials serve multiple functions beyond regulatory requirements, providing essential data for evidence-based medicine and healthcare policy development. Through controlled experimental designs, these studies test scientific hypotheses and generate reliable data that guides clinical practice standards. Clinical trials also facilitate the development of novel therapeutic approaches for diseases with limited treatment options, potentially expanding therapeutic possibilities for previously untreatable conditions.
Knowledge of clinical trial methodology and objectives is therefore essential for healthcare professionals, researchers, and patients participating in the medical research process.
Key Takeaways
- Clinical trials are essential for testing the safety and effectiveness of new medical treatments.
- Phase 0 trials involve very limited human exposure to assess preliminary drug behavior.
- Phase I trials focus on safety and dosage in a small group of healthy volunteers.
- Phase II and III trials evaluate efficacy and monitor side effects in larger patient groups.
- Phase IV trials occur after approval to gather long-term safety data and real-world effectiveness.
Phase 0 Clinical Trials
Phase 0 clinical trials, also known as microdosing studies, represent a relatively new approach in the drug development process. These trials are designed to gather preliminary data on how a drug behaves in the human body without exposing participants to significant risk. Typically involving a small number of subjects, Phase 0 trials allow researchers to assess pharmacokinetics—the study of how a drug is absorbed, distributed, metabolized, and excreted—using subtherapeutic doses.
This phase is particularly valuable for compounds that have shown promise in preclinical studies but require further investigation before advancing to more extensive trials. One of the key advantages of Phase 0 trials is their ability to expedite the drug development process. By providing early insights into a drug’s behavior in humans, researchers can make informed decisions about whether to proceed with further testing.
For instance, if a drug demonstrates unfavorable pharmacokinetic properties in a Phase 0 trial, it may be abandoned early in the development process, saving time and resources. An example of this can be seen in the development of certain cancer therapies, where understanding how a drug interacts with human biology at an early stage can significantly influence subsequent trial designs.
Phase I Clinical Trials
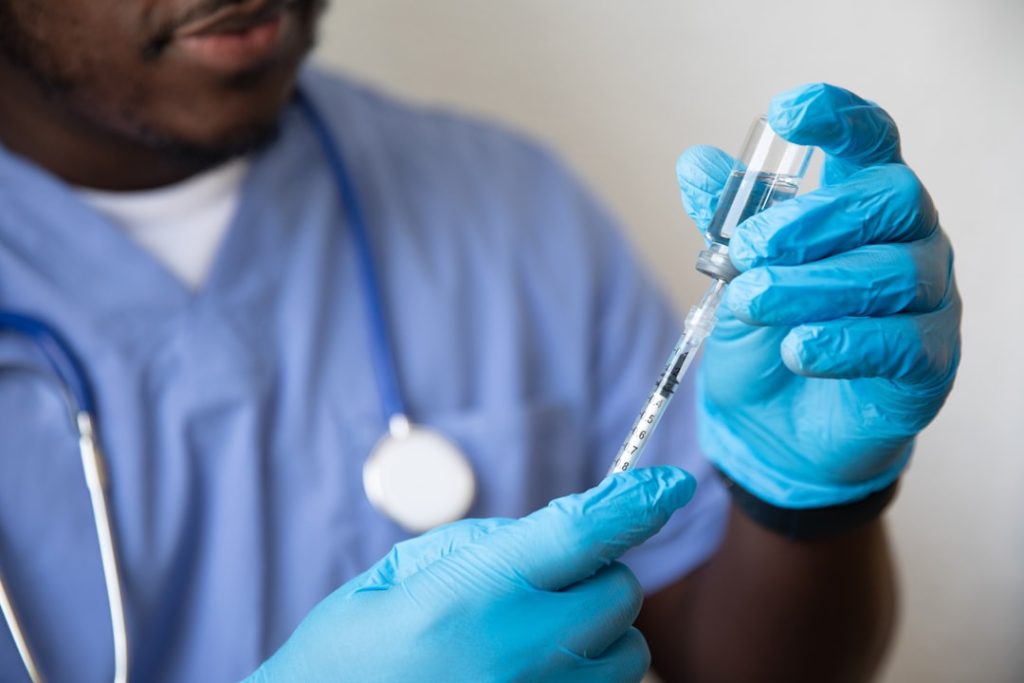
Phase I clinical trials are the first stage of testing in human subjects and primarily focus on assessing the safety and tolerability of a new drug or treatment. Typically involving a small group of healthy volunteers or patients with specific conditions, these trials aim to determine the maximum tolerated dose (MTD) and identify any potential side effects. Researchers closely monitor participants for adverse reactions and gather data on how the drug is metabolized in the body.
This phase is crucial for establishing a safety profile that will inform subsequent phases of testing. In addition to safety assessments, Phase I trials often explore different dosing regimens and administration routes. For example, a new chemotherapy agent may be tested in various formulations—such as intravenous versus oral administration—to determine which method yields the best therapeutic outcomes with minimal side effects.
A notable case is the development of imatinib (Gleevec), a groundbreaking treatment for chronic myeloid leukemia (CML). The initial Phase I trial demonstrated not only safety but also promising efficacy, leading to further studies that ultimately transformed CML treatment paradigms.
Phase II Clinical Trials
Phase II clinical trials build upon the findings from Phase I by focusing on the efficacy of a treatment while continuing to monitor its safety. This phase typically involves a larger group of participants who have the condition that the drug aims to treat. Researchers seek to determine whether the drug produces a beneficial effect on the disease and at what dose this effect is most pronounced.
Phase II trials often employ randomized designs and may include control groups receiving standard treatments or placebos to provide comparative data. One significant aspect of Phase II trials is their ability to refine treatment protocols based on preliminary efficacy data. For instance, if an investigational drug shows promise in reducing tumor size in cancer patients during Phase II testing, researchers may adjust dosing schedules or combination therapies to enhance its effectiveness.
A prime example is the development of trastuzumab (Herceptin) for HER2-positive breast cancer. Initial Phase II trials revealed substantial tumor response rates, leading to accelerated approval and subsequent Phase III studies that confirmed its benefits in larger populations.
Phase III Clinical Trials
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety and dosage | 20-100 healthy volunteers | Several months | Safety, side effects, pharmacokinetics | 70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Effectiveness, optimal dose | 33% |
| Phase 3 | Confirm effectiveness and monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Comparison with standard treatments | 25-30% |
| Phase 4 | Post-marketing surveillance | Varies (thousands) | Ongoing | Long-term effects, rare side effects | N/A |
Phase III clinical trials are pivotal in the drug development process as they provide definitive evidence regarding a treatment’s efficacy and safety in larger populations. These trials typically involve hundreds or thousands of participants across multiple sites and are designed to compare the new treatment against standard care or placebo in a randomized controlled setting. The primary goal is to establish whether the new intervention offers significant benefits over existing therapies, which is critical for regulatory approval by agencies such as the U.S.
Food and Drug Administration (FDA). The rigorous nature of Phase III trials ensures that any observed effects are statistically significant and clinically meaningful. For example, the landmark trial for the anticoagulant rivaroxaban (Xarelto) demonstrated its superiority over warfarin in preventing stroke in patients with atrial fibrillation.
The results not only led to its approval but also changed clinical practice guidelines worldwide. The comprehensive data generated during Phase III trials serve as the foundation for labeling claims and inform healthcare providers about the best treatment options available.
Phase IV Clinical Trials

Phase IV clinical trials, also known as post-marketing studies, occur after a drug has received regulatory approval and is available for public use. These trials serve several purposes: they monitor long-term safety and effectiveness, assess the drug’s performance in diverse populations, and evaluate its impact on quality of life. Phase IV studies can take various forms, including observational studies, randomized controlled trials, or registry-based research.
One critical aspect of Phase IV trials is their ability to identify rare adverse events that may not have been apparent during earlier phases due to limited sample sizes or short follow-up periods. For instance, after the approval of certain vaccines, Phase IV studies have been instrumental in monitoring long-term safety profiles and identifying any infrequent side effects that may arise once a larger population is vaccinated. The ongoing evaluation of medications through Phase IV trials ensures that healthcare providers have access to up-to-date information regarding risks and benefits, ultimately enhancing patient safety.
Understanding the Importance of Each Phase
Each phase of clinical trials plays a vital role in ensuring that new treatments are safe and effective before they reach patients. The structured approach allows researchers to systematically evaluate various aspects of a drug’s performance while minimizing risks to participants. Phase 0 provides early insights into pharmacokinetics; Phase I establishes safety profiles; Phase II assesses efficacy; Phase III confirms benefits against standard treatments; and Phase IV monitors long-term outcomes post-approval.
The importance of this phased approach cannot be overstated. It not only protects participants but also builds public trust in medical research. By adhering to rigorous standards throughout each phase, researchers can provide robust evidence that informs clinical practice and regulatory decisions.
Furthermore, understanding these phases helps stakeholders—including patients—navigate the complexities of clinical research and appreciate the significance of participation in such studies.
Conclusion and Future of Clinical Trials
The landscape of clinical trials is continually evolving, driven by advancements in technology, regulatory changes, and an increasing emphasis on patient-centered research. Innovations such as adaptive trial designs allow for more flexible methodologies that can adjust based on interim results, potentially speeding up the development process while maintaining scientific rigor. Additionally, the integration of real-world evidence from electronic health records and patient registries is enhancing our understanding of treatment effects outside controlled environments.
As we look toward the future, there is a growing recognition of the need for diversity in clinical trial populations to ensure that findings are applicable across different demographics. Efforts are underway to engage underrepresented groups in research actively, addressing historical disparities in access to clinical trials. The incorporation of patient perspectives into trial design is also gaining traction, emphasizing outcomes that matter most to those affected by diseases.
In summary, clinical trials remain an essential component of medical advancement, with each phase contributing uniquely to our understanding of new therapies. As methodologies continue to evolve and adapt to contemporary challenges, the potential for breakthroughs in treatment options will only expand, ultimately benefiting patients worldwide.