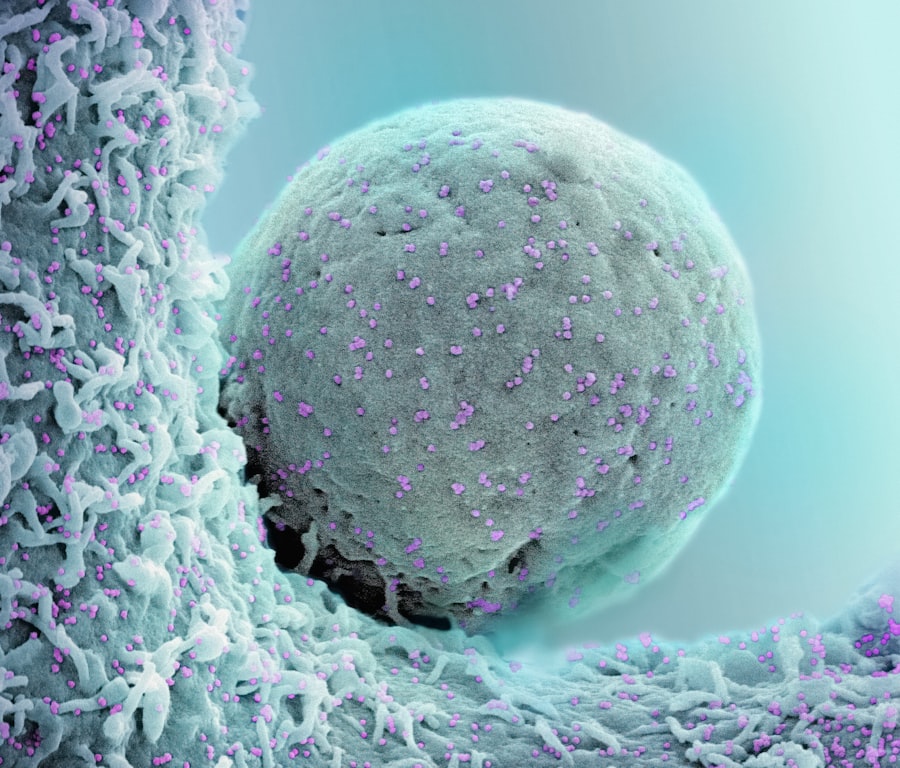
Targeted therapies represent a paradigm shift in the treatment of cancer, moving away from traditional chemotherapy and radiation approaches that indiscriminately affect both cancerous and healthy cells. These therapies are designed to specifically target molecular abnormalities that are unique to cancer cells, thereby minimizing damage to normal tissues and reducing side effects. By focusing on specific pathways and mutations that drive tumor growth, targeted therapies can inhibit cancer progression more effectively than conventional treatments.
For instance, drugs like trastuzumab (Herceptin) target the HER2 protein overexpressed in certain breast cancers, leading to improved outcomes for patients with this specific biomarker. The development of targeted therapies has been fueled by advances in our understanding of cancer biology and genetics. Researchers have identified various oncogenes and tumor suppressor genes that play critical roles in the development and progression of different cancers.
This knowledge has paved the way for the creation of drugs that can interfere with these molecular targets. For example, imatinib (Gleevec) was developed to treat chronic myeloid leukemia (CML) by specifically inhibiting the BCR-ABL fusion protein, a product of a chromosomal translocation that is characteristic of this disease. The success of such targeted therapies has not only improved survival rates but has also transformed the way oncologists approach cancer treatment, emphasizing the importance of personalized medicine.
Key Takeaways
- Targeted therapies focus on specific cancer biomarkers to personalize treatment and improve outcomes.
- Overcoming resistance mechanisms is crucial for the long-term success of targeted cancer treatments.
- Combining targeted therapies with immunotherapy can enhance the effectiveness of cancer care.
- Pediatric cancers present unique challenges that require tailored approaches to targeted therapy.
- Advancements in precision medicine are driving the future of cancer treatment and clinical application.
Identifying Biomarkers for Personalized Treatment
Biomarkers are biological indicators that can provide critical information about the presence or progression of disease, as well as the likely response to specific treatments. In the context of cancer, biomarkers can be genetic, epigenetic, or proteomic in nature and are essential for the successful implementation of targeted therapies. The identification of these biomarkers allows clinicians to tailor treatment plans based on the individual characteristics of a patient’s tumor, leading to more effective and less toxic treatment regimens.
For instance, the presence of mutations in the EGFR gene can indicate that a patient with non-small cell lung cancer (NSCLC) is likely to respond to EGFR inhibitors such as erlotinib or gefitinib. The process of identifying biomarkers involves sophisticated techniques such as next-generation sequencing (NGS), which allows for comprehensive genomic profiling of tumors. This technology enables researchers to detect mutations, copy number variations, and other genomic alterations that may inform treatment decisions.
Additionally, liquid biopsies are emerging as a non-invasive method to identify circulating tumor DNA (ctDNA) in the bloodstream, providing real-time insights into tumor dynamics and treatment response. As our understanding of cancer genomics continues to evolve, the potential for discovering new biomarkers will enhance the precision of targeted therapies and improve patient outcomes.
Overcoming Resistance to Targeted Therapies

Despite the promise of targeted therapies, resistance remains a significant challenge in cancer treatment. Tumors can develop resistance through various mechanisms, including genetic mutations, activation of alternative signaling pathways, or changes in tumor microenvironment. For example, patients treated with EGFR inhibitors may initially respond well; however, they often develop resistance due to secondary mutations in the EGFR gene or activation of bypass pathways such as MET amplification.
This phenomenon underscores the need for ongoing research to understand the mechanisms underlying resistance and to develop strategies to overcome it. One approach to combat resistance is the use of combination therapies that target multiple pathways simultaneously. By employing a multi-faceted strategy, oncologists can potentially prevent or delay the emergence of resistant clones within a tumor.
For instance, combining targeted therapies with other agents that inhibit alternative pathways or enhance immune responses may provide a more robust treatment approach. Clinical trials are currently exploring various combinations, such as pairing BRAF inhibitors with MEK inhibitors in patients with BRAF-mutant melanoma, which has shown promise in overcoming resistance and improving patient outcomes.
Combining Targeted Therapies with Immunotherapy
The integration of targeted therapies with immunotherapy represents an exciting frontier in cancer treatment. While targeted therapies focus on specific molecular alterations within tumors, immunotherapy harnesses the body’s immune system to recognize and attack cancer cells. The combination of these two approaches has the potential to enhance therapeutic efficacy and improve patient outcomes.
For example, combining checkpoint inhibitors like pembrolizumab with targeted therapies such as BRAF/MEK inhibitors has shown synergistic effects in patients with melanoma harboring BRAF mutations. This combination strategy is particularly appealing because it addresses different aspects of tumor biology. Targeted therapies can reduce tumor burden and potentially enhance antigen presentation, making cancer cells more recognizable to the immune system.
Meanwhile, immunotherapy can help eliminate residual disease and prevent recurrence by promoting long-lasting immune memory against cancer cells. Ongoing clinical trials are investigating various combinations across different cancer types, aiming to identify optimal treatment regimens that maximize benefits while minimizing adverse effects.
Addressing the Challenges of Targeted Therapies in Pediatric Cancers
| Metric | Value |
|---|---|
| Journal Name | Journal of Clinical Cancer Research |
| Impact Factor (2023) | 12.531 |
| 5-Year Impact Factor | 13.245 |
| Immediacy Index | 2.134 |
| CiteScore | 14.7 |
| H-Index | 150 |
| Publisher | American Association for Cancer Research |
| Publication Frequency | Monthly |
While targeted therapies have revolutionized adult oncology, their application in pediatric cancers presents unique challenges. Pediatric tumors often exhibit distinct biological characteristics compared to adult cancers, including differences in genetic mutations and tumor microenvironments. Additionally, many targeted therapies developed for adults have not been adequately tested in children, leading to a gap in available treatment options for young patients.
For instance, while imatinib has been a game-changer for adult CML patients, its use in pediatric populations requires careful consideration due to differences in pharmacokinetics and potential side effects. Moreover, the rarity of many pediatric cancers complicates research efforts aimed at developing targeted therapies. With fewer patients available for clinical trials, it can be challenging to gather sufficient data to support regulatory approval for new treatments.
Collaborative efforts among institutions and organizations are essential to facilitate research in this area. Initiatives like the Children’s Oncology Group (COG) aim to conduct large-scale studies that can provide insights into the efficacy and safety of targeted therapies in children. By fostering collaboration and focusing on biomarker-driven approaches, researchers hope to improve outcomes for pediatric cancer patients through tailored treatment strategies.
Harnessing the Potential of Precision Medicine in Cancer Care
Precision medicine represents a transformative approach in oncology that seeks to customize treatment based on individual patient characteristics, including genetic makeup, tumor biology, and environmental factors. The integration of precision medicine into cancer care has been facilitated by advancements in genomic technologies and bioinformatics, enabling clinicians to make informed decisions about treatment options tailored to each patient’s unique profile. This approach not only enhances therapeutic efficacy but also minimizes unnecessary exposure to ineffective treatments.
One notable example of precision medicine in action is the use of comprehensive genomic profiling to guide therapy selection for patients with advanced solid tumors. By analyzing a patient’s tumor DNA for actionable mutations, oncologists can identify targeted therapies that are most likely to yield positive outcomes. For instance, patients with tumors harboring NTRK gene fusions may benefit from TRK inhibitors like larotrectinib or entrectinib, regardless of tumor type.
This shift towards a more personalized approach underscores the importance of understanding individual tumor biology and leveraging available treatments accordingly.
Exploring the Future of Targeted Therapies in Cancer Treatment
The future of targeted therapies in cancer treatment is poised for significant advancements as research continues to uncover new molecular targets and refine existing therapeutic strategies. One promising area is the development of next-generation targeted agents that can overcome resistance mechanisms associated with current therapies. For example, novel compounds designed to target specific mutations or bypass resistant pathways are being explored in clinical trials, offering hope for patients who have exhausted standard treatment options.
Additionally, advancements in artificial intelligence (AI) and machine learning are expected to play a crucial role in identifying new targets and predicting treatment responses. By analyzing vast datasets from genomic studies and clinical trials, AI algorithms can uncover patterns that may not be immediately apparent to human researchers. This could lead to the discovery of novel biomarkers and therapeutic targets that enhance our understanding of cancer biology and improve treatment outcomes.
Translating Research Findings into Clinical Practice
The translation of research findings into clinical practice is essential for ensuring that advancements in targeted therapies benefit patients effectively and efficiently. Bridging the gap between laboratory discoveries and real-world applications requires collaboration among researchers, clinicians, regulatory agencies, and pharmaceutical companies. Initiatives aimed at streamlining clinical trial processes and expediting drug approvals are critical for bringing innovative therapies to market.
Moreover, ongoing education and training for healthcare professionals are vital to ensure they remain informed about emerging therapies and their appropriate use in clinical settings. As new targeted agents become available, oncologists must be equipped with the knowledge necessary to interpret biomarker testing results and make informed treatment decisions based on individual patient profiles. By fostering a culture of collaboration and continuous learning within the oncology community, we can enhance the implementation of targeted therapies and ultimately improve patient care outcomes across diverse populations.