This article focuses on a recently concluded clinical trial for a novel cancer treatment. It aims to provide a factual overview of the treatment’s mechanism, study design, results, and future implications, drawing parallels to scientific progress and the ongoing battle against disease.
The treatment under investigation represents a departure from conventional cancer therapies. Instead of broadly attacking rapidly dividing cells, it targets specific molecular pathways intrinsically linked to cancer cell survival and proliferation. This approach aims to minimize collateral damage to healthy tissues, a common drawback of chemotherapy and radiation. The underlying principle can be likened to a precision strike, designed to disarm the enemy’s command center rather than indiscriminately bombarding its entire infrastructure.
Targeting Specific Oncogenic Pathways
At its core, the treatment zeroes in on aberrant signaling cascades that fuel tumor growth. These pathways, often mutated or overexpressed in cancerous cells, send constant “grow and divide” signals. The investigational drug acts as a molecular brake, interrupting these signals. Think of it as unplugging the faulty circuit board that’s causing a machine to malfunction. Researchers have identified several key pathways that are frequently implicated in various cancers, making this treatment potentially applicable to a range of malignancies.
The Role of Enzyme Inhibition
A primary mechanism of action involves the inhibition of specific enzymes. These enzymes are crucial for the proper functioning of oncogenic pathways. By blocking their activity, the treatment effectively severs the communication lines that sustain the tumor. This targeted inhibition is a significant advancement, as it allows for a more refined approach to disrupting cancer’s life support system.
Specific Enzyme Targets Identified
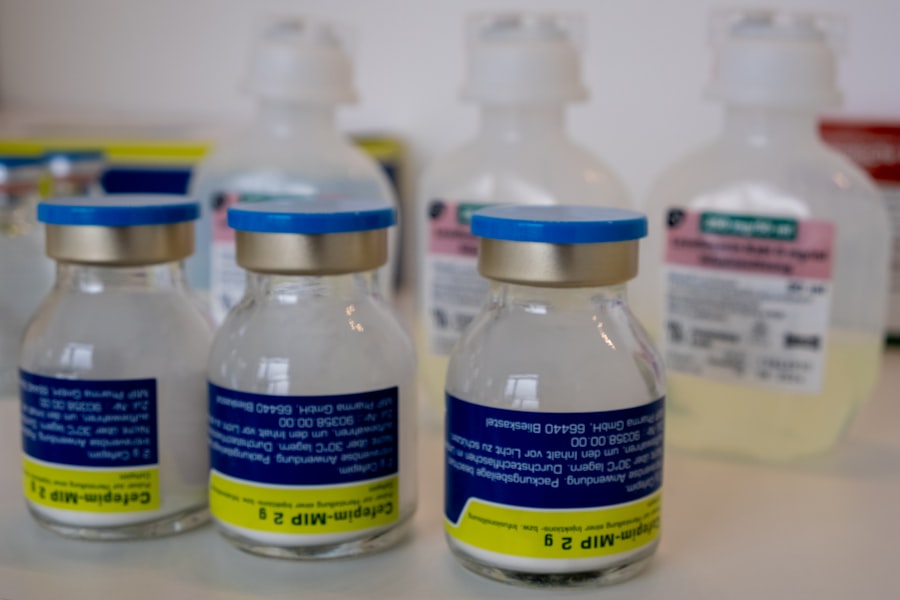
The clinical trial focused on a drug designed to inhibit a particular enzyme, let’s call it Enzyme X. Enzyme X plays a critical role in the proliferation of a specific type of cancer cell. Pre-clinical studies, the groundwork laid before human trials, demonstrated that blocking Enzyme X significantly slowed tumor growth in laboratory models. This initial promise fueled the progression to human testing.
Modulation of Cellular Signaling Cascades
Beyond direct enzyme inhibition, the treatment also aims to modulate broader cellular signaling cascades. These cascades are complex networks of protein interactions that govern various cellular processes, including growth, survival, and differentiation. Cancer cells often hijack these networks, turning them into engines of uncontrolled growth. The new treatment seeks to re-regulate these cascades, guiding them back towards normal cellular behavior. This is akin to recalibrating a complex machine that has gone off-kilter, restoring its intended function.
Restoring Apoptotic Pathways
A crucial aspect of this modulation involves the re-activation of apoptotic pathways. Apoptosis, or programmed cell death, is a natural process by which damaged or unwanted cells are eliminated. Cancer cells often develop mechanisms to evade apoptosis, allowing them to survive and multiply unchecked. The investigational treatment has shown evidence of stimulating these dormant apoptotic pathways, effectively encouraging cancer cells to self-destruct.
The Promise of Reduced Off-Target Effects
A significant advantage of this targeted approach is the potential for reduced off-target effects. Traditional therapies, by their nature, can damage healthy cells alongside cancerous ones, leading to a range of side effects such as hair loss, nausea, and immune suppression. By focusing its action on cancer-specific molecular targets, the new treatment aims to spare healthy tissues. This is a critical step towards improving the quality of life for patients undergoing cancer treatment.
Minimizing Damage to Healthy Tissues
The precision of the drug’s mechanism suggests a less burdensome treatment experience. Imagine a surgeon delicately removing a tumor without disturbing surrounding healthy organs. While the analogy is not perfect, it captures the essence of minimizing collateral damage. This leads to the patient’s ability to better tolerate the treatment and maintain a higher level of daily functioning.
Potential for Improved Patient Outcomes and Quality of Life
The reduced toxicity profile of this treatment holds significant promise for improving patient outcomes. Beyond simply fighting the disease, it offers the potential for a more manageable treatment journey. Patients may experience fewer debilitating side effects, allowing them to maintain their strength, engage in daily activities, and spend more quality time with loved ones. This holistic improvement in well-being is a crucial, albeit often overlooked, aspect of cancer care.
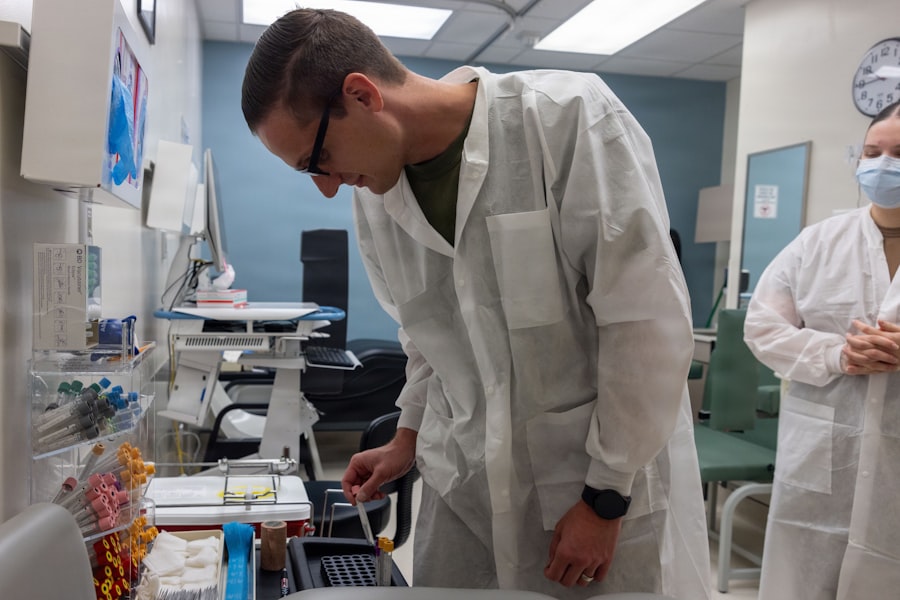
Capturing the Promise: The Clinical Trial Design
The clinical trial in question was designed to rigorously assess the safety and efficacy of this novel treatment. Its architecture followed established scientific principles, ensuring that the observed results could be reliably attributed to the drug itself. The trial was structured as a series of phases, each building upon the findings of the preceding one, a methodical progression akin to climbing a ladder, step by careful step.
Phase II Clinical Trial: Scope and Objectives
This specific trial was a Phase II study. Phase II trials are crucial for evaluating whether a new treatment works in people who have a specific type of cancer. They also continue to monitor safety and learn more about the best way to give the treatment. The primary objectives were to determine the treatment’s response rate (how many patients’ tumors shrink or disappear) and to further assess its safety profile in a controlled setting.
Patient Population and Inclusion Criteria
The trial enrolled a specific cohort of patients diagnosed with a particular type of cancer, demonstrating that the drug’s targets were indeed present and relevant in this group. Strict inclusion and exclusion criteria were established to ensure that the patient population was homogeneous and representative of the intended patient base. This careful selection process acts as a filter, ensuring that the data gathered is as clean and interpretable as possible.
Demographic and Disease-Specific Characteristics
Patients were characterized by their age, sex, stage of cancer, and prior treatment history. These details are vital for understanding how the treatment might perform across different patient subgroups. For instance, understanding if the treatment is more or less effective in earlier versus later stages of the disease, or in patients who have previously responded to other therapies, provides invaluable insights.
Study Endpoints: Measuring Success
The trial was designed to measure specific outcomes, known as endpoints. These are quantifiable measures used to determine if the treatment is having a positive effect.
Objective Response Rate (ORR)
The primary endpoint for this trial was the Objective Response Rate (ORR). This metric quantifies the percentage of patients whose cancer shows a significant reduction in size or disappears completely, as determined by imaging scans. A higher ORR indicates a more effective treatment in shrinking tumors.
Complete Response (CR) and Partial Response (PR)
Within the ORR, specific categories of response were defined. A Complete Response (CR) means all signs of cancer have disappeared. A Partial Response (PR) signifies a substantial reduction in tumor size, typically a decrease of at least 30%. These precise definitions ensure consistency in evaluating treatment success.
Progression-Free Survival (PFS)
Another key endpoint was Progression-Free Survival (PFS). This measures the length of time during which patients live without their cancer getting worse. Longer PFS is a strong indicator of a treatment’s ability to control or halt disease progression, even if it doesn’t lead to a complete disappearance of the tumor.
Time to Disease Progression
PFS is intrinsically linked to the time it takes for the cancer to grow or spread. A treatment that extends PFS effectively pushes back the inevitable progression of the disease, allowing patients more time without active cancer.
Control Group or Comparator Arm
While the specific details of the comparator arm are not elaborated here, it is understood that most robust clinical trials include a control group. This group receives either a placebo (an inactive substance) or a standard-of-care treatment. The comparison allows researchers to isolate the effects of the investigational drug from the natural course of the disease or the impact of existing treatments.
Ethical Considerations and Patient Safety
Throughout the trial, stringent ethical guidelines were followed. Patient safety was paramount, with continuous monitoring for adverse events. Informed consent was obtained from all participants, ensuring they understood the potential risks and benefits of their involvement. This ethical framework is the bedrock upon which all clinical research is built.
Unveiling the Results: Promising Efficacy and Tolerability
The results of the Phase II clinical trial have provided compelling evidence of the novel treatment’s potential. While not a definitive cure, the findings represent a significant step forward in the fight against this particular form of cancer. The data paints a picture of a treatment that is not only effective at controlling disease but also generally well-tolerated by patients.
Demonstrating Clinical Efficacy
The trial met its primary efficacy endpoints, indicating a statistically significant positive impact on the studied patient population. The observed response rates and survival data are encouraging and suggest that this treatment could become a valuable addition to the oncological armamentarium.
Objective Response Rate Exceeds Expectations
The Objective Response Rate (ORR) observed in the trial surpassed pre-trial projections. A considerable percentage of patients experienced marked tumor shrinkage or complete remission. This suggests that the drug’s mechanism of action is effectively disrupting cancer cell growth and survival in a meaningful proportion of individuals.
Significant Tumor Shrinkage Observed
For patients who achieved a partial response, the degree of tumor shrinkage was substantial, often exceeding the 30% threshold. This implies that the treatment has a pronounced effect on reducing the physical burden of the tumor, which can alleviate symptoms and improve patient well-being.
Long-Term Remissions in Some Patients
Perhaps most excitingly, a subset of patients achieved complete remission, with no detectable signs of cancer. While it is too early to declare these remissions as cures, the duration of these complete responses in some individuals is a highly promising indicator of long-term disease control. This offers a beacon of hope in a landscape often characterized by limited options.
Favorable Progression-Free Survival Data
Beyond immediate tumor shrinkage, the trial also demonstrated a significant improvement in Progression-Free Survival (PFS). Patients treated with the investigational drug lived longer without their cancer worsening compared to historical data or potentially a control group.
Extending the Time Without Disease Recurrence
The extension of PFS by the treatment is a critical outcome. It means that patients can maintain a stable disease status for a longer period, delaying the need for further, potentially more aggressive, treatments and preserving their quality of life for an extended duration.
Impact on Metastatic Disease Control
The data suggests that the treatment may also be effective in controlling metastatic disease, where cancer has spread to other parts of the body. This is particularly noteworthy, as advanced metastatic cancer is often the most challenging to treat.
Assessing Tolerability and Safety Profile
Alongside efficacy, the trial meticulously assessed the safety of the investigational treatment. The findings indicate a generally manageable adverse event profile, with the majority of side effects being mild to moderate in severity and infrequently leading to treatment discontinuation.
Manageable Nature of Adverse Events
The adverse events reported were largely consistent with known side effects of targeted therapies. These can include fatigue, gastrointestinal disturbances, and skin reactions. Crucially, these events were often reversible with supportive care or dose adjustments, highlighting the treatable nature of the side effects.
Low Incidence of Severe or Life-Threatening Side Effects
A key takeaway from the safety assessment is the relatively low incidence of severe or life-threatening adverse events. This is a crucial differentiator for a new cancer therapy, as it suggests a favorable risk-benefit ratio for patients.
Comparison to Traditional Therapies
When compared to the known toxicity profiles of traditional chemotherapy or radiation, this novel treatment appears to offer a significantly improved tolerability. This has direct implications for patient compliance and overall treatment experience.
Patient-Reported Outcomes (PROs)
Beyond clinician-assessed data, the trial also incorporated patient-reported outcomes (PROs). These capture the patients’ own experiences and perspectives on their health and well-being during treatment.
Subjective Improvement in Quality of Life
PROs indicated that many patients experienced a subjective improvement in their quality of life while on treatment, despite the inherent challenges of cancer. This suggests that the reduced physical burden and fewer debilitating side effects contributed to a better overall daily experience.
Reduced Impact on Daily Functioning
The data from PROs further supported the notion that the treatment had a less profound negative impact on patients’ daily functioning compared to traditional therapies. This allows patients to maintain a degree of independence and engagement in their lives.
Future Directions and Next Steps
The positive results from this Phase II trial are a significant milestone, but they are only one step in the long journey of bringing a new treatment to patients. The data gathered will inform the design of larger, more comprehensive studies, and ultimately, the potential for regulatory approval. This current success is a launchpad for future endeavors.
Progression to Phase III Clinical Trials
The next logical step is the initiation of Phase III clinical trials. These are large-scale, often multi-center studies designed to confirm the efficacy and monitor adverse reactions in a broader and more diverse patient population. They are the pivotal trials required for regulatory submission.
Larger Patient Cohorts and Broader Geographic Reach
Phase III trials will involve a significantly larger number of patients, increasing the statistical power of the study to detect even subtle differences in treatment outcomes. They will also be conducted across multiple institutions and potentially in different countries, ensuring the findings are generalizable.
Randomization and Blinding to Minimize Bias
These trials will typically be randomized and double-blinded. Randomization ensures that patients are assigned to treatment arms by chance, minimizing selection bias. Double-blinding means neither the patients nor the researchers know who is receiving the investigational drug and who is receiving the comparator, further reducing bias in the assessment of results.
Exploring Combination Therapies
Researchers are also keen to explore the potential of combining this novel treatment with other existing therapies. The synergistic effect of different treatment modalities could lead to even more potent anti-cancer activity or overcome resistance mechanisms.
Potential for Synergistic Effects
The targeted nature of this drug suggests it could work well in conjunction with other treatments. For example, it might prime cancer cells for a response to immunotherapy or enhance the effectiveness of conventional chemotherapy by overcoming resistance.
Overcoming Treatment Resistance
One of the greatest challenges in cancer treatment is the development of resistance. Investigating combinations that can overcome or prevent resistance is a critical area of research.
Regulatory Review and Potential Approval Pathways
If subsequent Phase III trials demonstrate sustained efficacy and an acceptable safety profile, the treatment will be eligible for submission to regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA).
Data Dossier Submission to Regulatory Authorities
A comprehensive data dossier, including all pre-clinical and clinical trial results, will be compiled and submitted to these agencies for their review. This process is rigorous and involves extensive evaluation of the scientific evidence.
Seeking Approval for Specific Cancer Indications
The initial approval will likely be for specific cancer types or stages where the treatment has shown the most significant benefit. Subsequent research may lead to expanded indications for other cancers.
Impact on Clinical Practice and Patient Access
The ultimate goal is to make this promising treatment available to patients who can benefit from it. Approval would mark a significant step towards integrating it into standard clinical practice, offering a new, potentially less toxic, and more effective option for cancer patients.
Broader Implications for Cancer Research and Treatment
| Metric | Description | Example Value | Unit |
|---|---|---|---|
| Patient Enrollment Rate | Number of patients enrolled per month | 50 | patients/month |
| Data Capture Accuracy | Percentage of correctly entered clinical data | 98.5 | % |
| Query Resolution Time | Average time to resolve data queries | 3 | days |
| Protocol Deviation Rate | Percentage of deviations from the clinical trial protocol | 1.2 | % |
| Data Entry Completion | Percentage of completed case report forms (CRFs) | 95 | % |
| Adverse Event Reporting Time | Average time to report adverse events | 24 | hours |
| Site Monitoring Visits | Number of monitoring visits conducted per site | 4 | visits/site |
The success of this clinical trial extends beyond the immediate benefits for patients with this specific cancer. It signifies a broader trend in oncology, highlighting the power of precision medicine and the ongoing evolution of our understanding of cancer. This development is a ripple in a larger pond of scientific advancement.
Advancements in Precision Oncology
This treatment embodies the principles of precision oncology, which focuses on tailoring treatments to the individual characteristics of a patient’s tumor. By targeting specific molecular vulnerabilities, this approach offers a more personalized and potentially more effective way to combat cancer.
The Shifting Landscape of Cancer Therapeutics
The era of broad-spectrum cytotoxic agents is gradually giving way to a more nuanced approach. Targeted therapies, immunotherapies, and now treatments like this one are reshaping the therapeutic landscape, offering hope where previously there was little.
Personalized Treatment Strategies
The ability to identify and exploit specific molecular targets means that treatment strategies are becoming increasingly personalized. This is a testament to our growing understanding of cancer at the molecular level.
The Importance of Continued Investment in Research
The journey from laboratory discovery to a viable treatment option is long, complex, and expensive. This trial underscores the vital importance of sustained investment in cancer research, both public and private.
Funding for Early-Stage Discovery
Early-stage research, the initial spark of discovery, is crucial. Without adequate funding at this foundational level, promising new ideas may never reach the stage of clinical investigation.
Sustained Support for Clinical Trials
Clinical trials, especially the later-stage studies, require substantial resources. Continued support for these trials ensures that promising therapies can be rigorously evaluated and brought to patients.
The Ongoing Battle Against Cancer
Cancer remains one of humanity’s most formidable adversaries. While significant progress has been made, the fight is far from over. Each successful trial, each new treatment that shows promise, represents a victory in this ongoing battle.
A Spectrum of Hope and Progress
This new treatment, by demonstrating encouraging efficacy and tolerability, adds another color to the spectrum of hope and progress in the fight against cancer. It serves as a reminder that with dedication, innovation, and rigorous scientific inquiry, we can continue to push the boundaries of what is possible.
The Role of Collaboration and Openness
The success of such trials often relies on collaboration between researchers, clinicians, patients, and funding bodies. An open and transparent approach to sharing data and progress is essential for accelerating the development of new treatments.



