Maximizing Clinical Endpoint Solutions offers a pathway to streamline and enhance the effectiveness of clinical trials. As a critical component, these solutions aim to ensure that trial outcomes accurately reflect the true impact of an intervention. This involves a meticulous approach to defining, measuring, and analyzing clinical endpoints.
Clinical endpoints constitute the fundamental basis for evaluating the efficacy and safety of a medical treatment or intervention. They represent a direct measure of how a patient feels, functions, or survives. In essence, they are the ultimate destination of a clinical trial, indicating whether a treatment achieves its intended therapeutic goal.
Types of Clinical Endpoints
Clinical endpoints can be broadly categorized based on their nature and the aspect of patient health they represent.
Survival Endpoints
Survival endpoints are among the most definitive measures in clinical research, particularly in areas like oncology and infectious diseases. They focus on the duration of time until a specific event occurs, providing a clear indication of treatment benefit.
Overall Survival (OS)
Overall Survival measures the time from treatment assignment to death from any cause. It is considered a gold standard endpoint because it is less susceptible to certain biases and reflects the ultimate benefit of an intervention.
Progression-Free Survival (PFS)
Progression-Free Survival measures the time from treatment assignment to disease progression or death from any cause, whichever occurs first. It is often used in trials where delaying disease advancement is a primary treatment goal, even if overall survival is not immediately impacted.
Disease-Free Survival (DFS)
Disease-Free Survival is typically used in the adjuvant setting after a patient has undergone treatment for a disease and is assessed for recurrence. It measures the time from treatment until disease recurrence or death.
Clinical Event Endpoints
These endpoints focus on the occurrence of specific clinical events that indicate disease progression, treatment failure, or adverse outcomes.
Major Adverse Cardiovascular Events (MACE)
MACE is a composite endpoint commonly used in cardiovascular trials. It typically includes a combination of endpoints such as cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. Its composite nature allows for a more frequent accumulation of events, increasing statistical power.
Hospitalization Endpoints
Hospitalization for a specific condition, such as heart failure exacerbation or respiratory distress, serves as a clinical endpoint. It reflects a significant decline in a patient’s health status and the need for intervention.
Complication Endpoints
The occurrence of specific complications related to the disease or treatment, such as infection, bleeding, or organ damage, can be defined as endpoints. These highlight potential risks associated with an intervention.
Patient-Reported Outcomes (PROs)
Patient-Reported Outcomes are direct reports from patients about their health condition without interpretation from a clinician or investigator. These endpoints capture subjective experiences that are crucial for understanding the holistic impact of a treatment.
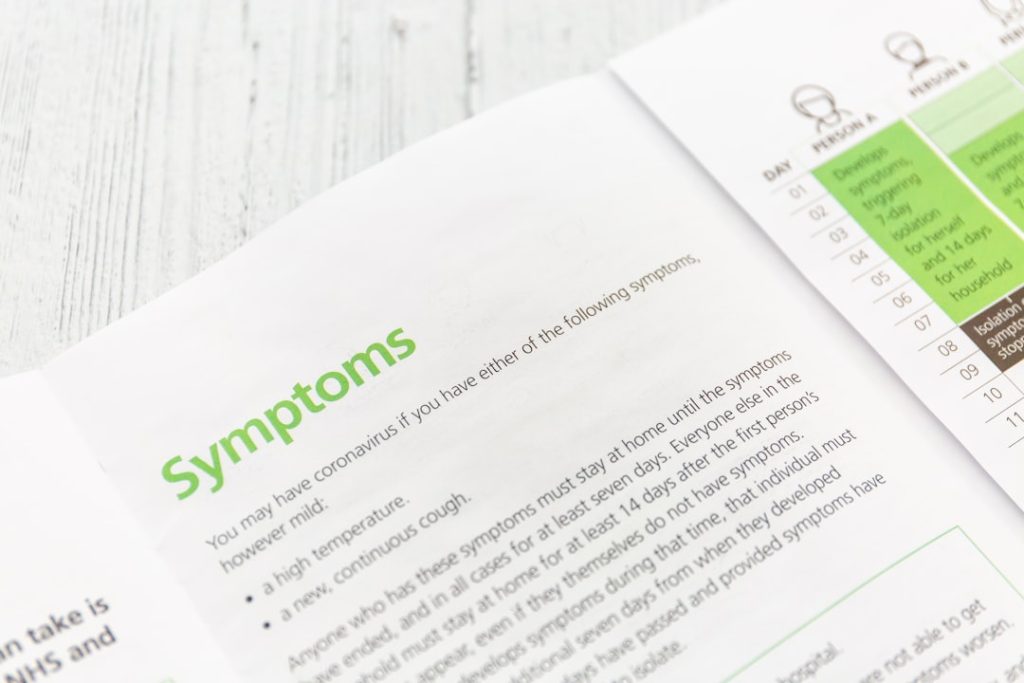
Symptom Scores
Patients can be asked to rate the severity of their symptoms using validated scales. This captures the patient’s perception of symptom burden and how it changes over time.
Functional Status Measures
These PROs assess a patient’s ability to perform daily activities. This can range from simple mobility to more complex tasks, providing insights into the treatment’s impact on quality of life and functional independence.
Quality of Life (QoL) Questionnaires
Comprehensive QoL questionnaires assess various domains of a patient’s well-being, including physical, emotional, and social functioning. These offer a broad perspective on how a treatment affects a patient’s overall life experience.
The Importance of Endpoint Selection
The careful selection of clinical endpoints is paramount to the success of any clinical trial. An inappropriate endpoint can lead to misleading results, wasted resources, and ultimately, a failure to identify a truly effective intervention, or conversely, the endorsement of an ineffective one. It’s like choosing the wrong destination on a map; you’ll end up somewhere you didn’t intend.
Alignment with Research Question
Endpoints must directly address the primary research question of the trial. If the question is about reducing mortality, survival endpoints are crucial. If it’s about improving daily functioning, PROs are essential.
Clinical Relevance
Endpoints should not only be statistically measurable but also have genuine clinical significance for patients and healthcare providers. A statistically significant reduction in a minor laboratory marker might not translate to a meaningful benefit for a patient.
Data Availability and Feasibility
The chosen endpoints must be reliably and consistently measurable within the constraints of the trial. This involves considering the availability of appropriate assessment tools, the burden on participants, and the logistics of data collection.
Leveraging WCG for Enhanced Endpoint Solutions
WCG, through its comprehensive suite of services and expertise, plays a pivotal role in optimizing clinical endpoint solutions. WCG acts as a guiding force, helping researchers navigate the complexities of endpoint definition, selection, and implementation.
Centralized Review and Oversight
WCG’s centralized review process provides a consistent and standardized approach to the evaluation of clinical trial protocols, including the critical aspect of endpoint selection.
Protocol Review Efficiency
By centralizing the review of multiple protocols, WCG streamlines the process, reducing redundant efforts and accelerating trial initiation. This allows for quicker progression towards acquiring valuable endpoint data.
Consistency in Endpoint Definition
WCG’s expert committees ensure consistency in the definition and validation of clinical endpoints across different trials and sites. This is vital for comparability of results and for avoiding ambiguity in data interpretation.
Ethical Considerations and Participant Protection
The ethical conduct of clinical trials is at the forefront of WCG’s mission. This extends to ensuring that endpoints are defined and measured in a way that prioritizes participant safety and well-being.
Minimizing Participant Burden
WCG advocates for endpoints that are clinically meaningful yet minimize the burden on participants. This involves carefully considering the frequency and invasiveness of assessments.
Informed Consent Transparency
The selection and explanation of endpoints are critical components of the informed consent process. WCG ensures that participants fully understand what is being measured and why, empowering them to make informed decisions.
Data Integrity and Quality Assurance
Maintaining the integrity and quality of endpoint data is non-negotiable. WCG’s systems and processes are designed to safeguard this data throughout the trial lifecycle.
Standardized Data Collection Protocols
WCG promotes the use of standardized protocols for data collection related to clinical endpoints. This reduces variability and enhances the reliability of the amassed information.
Monitoring and Auditing
WCG’s oversight includes monitoring and auditing trial sites to ensure that endpoint data is collected accurately and in accordance with the protocol. This acts as a crucial quality control mechanism.
Strategies for Maximizing Endpoint Data Collection

Effective strategies are essential for capturing high-quality endpoint data that truly reflects the intervention’s impact. This involves a proactive and meticulous approach to all stages of data collection.
Defining Measurable Data Points
Clearly defining the specific data points that will be collected for each endpoint is the first step toward robust data collection.
Objective Measures
Wherever possible, endpoints should be supported by objective measures that can be independently verified. This minimizes subjective interpretation and enhances reproducibility.
Subjective Measures with Validated Instruments
When subjective endpoints are necessary, it is crucial to utilize validated instruments and scales that have demonstrated reliability and validity. This provides a structured approach to capturing patient experiences.
Implementing Robust Data Management Systems
The foundation of reliable endpoint data lies in a robust and well-managed data system.
Electronic Data Capture (EDC)
The implementation of EDC systems facilitates efficient and accurate data entry, reducing transcription errors and allowing for real-time data review.
Data Validation Rules
Establishing and enforcing data validation rules within the EDC system helps to identify and correct errors at the source, significantly improving data quality.
Investigator and Site Training
The individuals collecting the data are critical to its quality. Comprehensive training ensures they understand their roles and responsibilities.
Protocol Understanding
Thorough training on the protocol, with a specific emphasis on endpoint definitions and collection methods, is essential for all site personnel.
Use of Assessment Tools
Hands-on training in the proper use of specific assessment tools, such as rating scales or diagnostic equipment, is vital to ensure accurate and consistent measurements.
Analyzing Endpoint Data for Meaningful Insights
Collecting data is only the first half of the equation. The subsequent analysis unlocks the true value of the endpoint information.
Statistical Methodologies
The choice of statistical methodologies must align with the type of endpoint and the trial design to ensure valid and interpretable results.
Appropriate Statistical Tests
Selecting the correct statistical tests for parametric and non-parametric data, as well as for time-to-event data, is crucial for drawing accurate conclusions. For example, using a t-test for data that doesn’t meet parametric assumptions might be like trying to fit a square peg into a round hole – it simply won’t work effectively.
Handling Missing Data
Robust strategies for handling missing endpoint data are necessary to avoid biased results. This may involve imputation techniques or sensitivity analyses.
Interpretation of Results
The statistical findings must be translated into clinically meaningful insights.
Clinical Significance vs. Statistical Significance
It is important to distinguish between statistical significance (likely due to a real effect) and clinical significance (the magnitude of the effect and its impact on patients). A statistically significant finding may not always be clinically relevant.
Biomarker Correlations
Where applicable, correlations between clinical endpoint data and relevant biomarkers can provide deeper understanding of the intervention’s mechanism of action and potential predictive factors.
Future Directions in Clinical Endpoint Solutions
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of Clinical Endpoints Supported | Total types of clinical endpoints WCG supports in trials | 150+ | Endpoints |
| Average Time to Endpoint Adjudication | Average duration to complete endpoint adjudication process | 14 | Days |
| Global Reach | Number of countries where WCG provides clinical endpoint solutions | 50+ | Countries |
| Number of Trials Supported | Total clinical trials utilizing WCG endpoint solutions annually | 500+ | Trials |
| Endpoint Adjudication Accuracy | Percentage accuracy in endpoint adjudication decisions | 99.5 | % |
| Customer Satisfaction Rate | Percentage of clients satisfied with WCG clinical endpoint services | 95 | % |
The field of clinical endpoint solutions is continuously evolving, driven by advancements in technology, a deeper understanding of disease, and a growing emphasis on patient-centered research.
Digital Health and Wearable Technology
The integration of digital health tools and wearable devices offers new avenues for objective and continuous endpoint data collection.
Remote Monitoring
Wearable sensors can track physiological parameters such as heart rate, activity levels, and sleep patterns, providing real-time insights into a patient’s condition outside of traditional clinical visits. This can be akin to having a continuous, unobtrusive observer in the patient’s life.
Digital Biomarkers
The data generated by these devices can be used to develop and validate digital biomarkers, which are objective measures of physiological or behavioral states derived from digital data.
Real-World Data (RWD) and Real-World Evidence (RWE)
The increasing availability of RWD is opening up new possibilities for endpoint evaluation and validation.
Complementing Trial Data
RWD can complement data from controlled clinical trials by providing insights into how interventions perform in broader, more diverse patient populations under routine care.
Post-Market Surveillance
RWD and RWE are becoming increasingly important for post-market surveillance, helping to monitor the long-term safety and effectiveness of approved treatments.
Artificial Intelligence and Machine Learning
AI and machine learning hold significant promise for advancing clinical endpoint solutions.
Predictive Modeling
These technologies can be used to develop predictive models that identify patients at higher risk of disease progression or adverse events, allowing for more targeted interventions and endpoint selection.
Endpoint Discovery
AI can aid in the discovery of novel endpoints or refine the definition of existing ones by analyzing large datasets and identifying patterns that might not be apparent through traditional methods.