Sleep quality is a multifaceted concept that encompasses not only the duration of sleep but also its depth and restorative properties. It is a critical component of overall health and well-being, influencing cognitive function, emotional regulation, and physical health. The World Health Organization recognizes sleep as a fundamental human need, essential for optimal functioning.
Poor sleep quality can lead to a myriad of health issues, including obesity, diabetes, cardiovascular diseases, and mental health disorders. Understanding the nuances of sleep quality is vital for both individuals seeking to improve their health and researchers aiming to develop effective interventions. The importance of sleep quality extends beyond mere rest; it plays a crucial role in various physiological processes.
During sleep, the body undergoes essential repair and maintenance activities, such as muscle growth, tissue repair, and the release of hormones that regulate appetite and stress. Furthermore, sleep is integral to memory consolidation and learning. The brain processes and organizes information acquired during the day, making it easier to recall later.
Thus, the quality of sleep directly impacts not only physical health but also cognitive performance and emotional stability.
Key Takeaways
- Understanding sleep quality is essential for overall health and well-being.
- Common sleep disorders include insomnia, sleep apnea, and restless leg syndrome.
- Clinical tests such as polysomnography help diagnose sleep issues accurately.
- Improved sleep quality positively affects cognitive function, mood, and physical health.
- Practical recommendations include maintaining a regular sleep schedule and creating a restful environment.
Common Sleep Disorders
Sleep disorders are prevalent conditions that disrupt the normal sleep cycle, leading to significant impairments in daily functioning. Among the most common disorders are insomnia, sleep apnea, restless legs syndrome (RLS), and narcolepsy. Insomnia is characterized by difficulty falling asleep or staying asleep, often resulting in daytime fatigue and irritability.
It can be triggered by various factors, including stress, anxiety, and certain medical conditions. Chronic insomnia can lead to long-term health consequences, making it imperative for individuals to seek effective treatment options. Sleep apnea is another widespread disorder that involves repeated interruptions in breathing during sleep.
This condition can lead to fragmented sleep and reduced oxygen levels in the blood, resulting in excessive daytime sleepiness and increased risk of cardiovascular problems. Obstructive sleep apnea (OSA) is the most common form, often associated with obesity and anatomical abnormalities in the upper airway. Treatment options for sleep apnea may include lifestyle changes, continuous positive airway pressure (CPAP) therapy, or surgical interventions.
Restless legs syndrome, characterized by an uncontrollable urge to move the legs, often exacerbates insomnia and can significantly impact sleep quality. Narcolepsy, a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, can lead to sudden bouts of sleep during the day and is often accompanied by cataplexy—a sudden loss of muscle tone triggered by strong emotions.
Clinical Test Methodology
Clinical tests for assessing sleep quality typically involve a combination of subjective assessments and objective measurements. Subjective assessments often include standardized questionnaires such as the Pittsburgh Sleep Quality Index (PSQI) or the Epworth Sleepiness Scale (ESS), which gauge an individual’s perception of their sleep patterns and daytime sleepiness. These tools provide valuable insights into the subjective experience of sleep quality but may be influenced by personal biases or varying interpretations of questions.
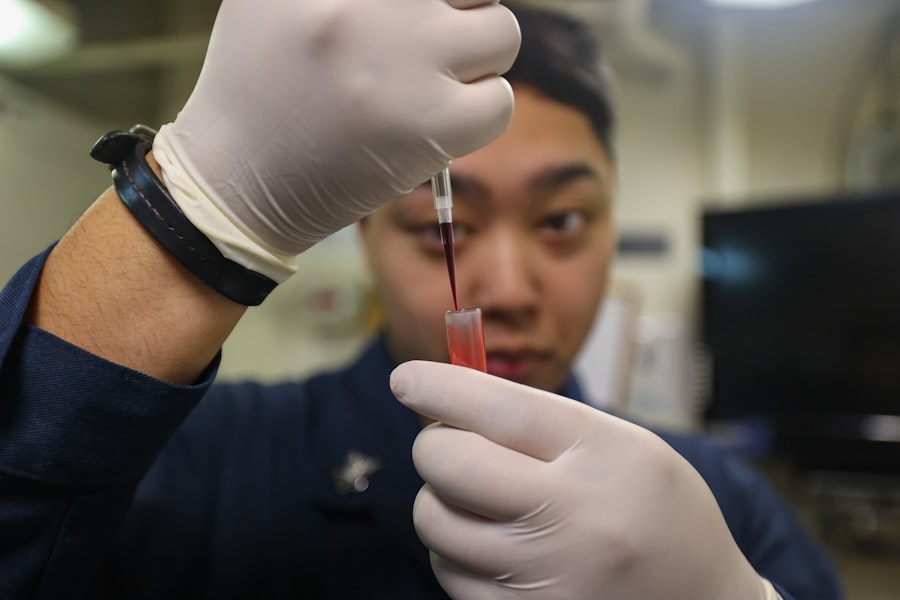
Objective measurements are often obtained through polysomnography (PSG), a comprehensive test that records brain waves, oxygen levels, heart rate, and breathing during sleep. PSG is considered the gold standard for diagnosing sleep disorders as it provides detailed information about sleep architecture, including the duration of different sleep stages such as REM (rapid eye movement) and non-REM sleep. Additionally, actigraphy—a method that uses a wrist-worn device to monitor movement—can provide insights into sleep patterns over extended periods in a naturalistic setting.
Combining subjective and objective measures allows researchers and clinicians to gain a holistic understanding of an individual’s sleep quality.
Results of Clinical Tests
| Test Name | Patient ID | Date Conducted | Result | Reference Range | Units | Comments |
|---|---|---|---|---|---|---|
| Complete Blood Count (CBC) | PT12345 | 2024-05-15 | Normal | N/A | N/A | All parameters within normal limits |
| Blood Glucose | PT12346 | 2024-05-16 | 105 | 70 – 110 | mg/dL | Fasting glucose level |
| Cholesterol | PT12347 | 2024-05-17 | 190 | < 200 | mg/dL | Borderline high |
| Hemoglobin A1c | PT12348 | 2024-05-18 | 5.7 | 4.0 – 5.6 | % | Pre-diabetic range |
| Blood Pressure | PT12349 | 2024-05-19 | 130/85 | 120/80 | mmHg | Elevated |
Clinical tests have yielded significant findings regarding the prevalence and impact of poor sleep quality on health outcomes. For instance, studies utilizing polysomnography have demonstrated that individuals with insomnia often experience reduced total sleep time and increased wakefulness after sleep onset compared to healthy sleepers. Furthermore, research has shown that those with obstructive sleep apnea exhibit disrupted sleep architecture characterized by frequent awakenings and reduced REM sleep, which is crucial for cognitive function.
The results from subjective assessments also reveal alarming trends in sleep quality across different populations. For example, a study involving college students found that nearly 70% reported experiencing poor sleep quality, with factors such as academic stress and irregular sleep schedules contributing to their difficulties. Similarly, surveys conducted among working adults indicate that high levels of work-related stress correlate with increased reports of insomnia symptoms.
These findings underscore the urgent need for targeted interventions aimed at improving sleep quality across various demographics.
Impact of Improved Sleep Quality
Improving sleep quality can have profound effects on both physical and mental health. Research has shown that individuals who achieve better sleep experience enhanced cognitive performance, including improved attention, memory retention, and problem-solving abilities. For instance, a study published in the journal “Sleep” found that participants who engaged in good sleep hygiene practices demonstrated significantly better performance on cognitive tasks compared to those with poor sleep habits.
Moreover, enhanced sleep quality is associated with better emotional regulation and reduced symptoms of anxiety and depression. A longitudinal study indicated that individuals who reported improvements in their sleep patterns also experienced a decrease in depressive symptoms over time. This relationship highlights the bidirectional nature of sleep and mental health; while poor sleep can exacerbate mental health issues, improving sleep can serve as a protective factor against emotional distress.
Additionally, better sleep quality has been linked to improved physical health outcomes, including lower rates of obesity and cardiovascular disease.
Recommendations for Better Sleep

To foster better sleep quality, several evidence-based recommendations can be implemented in daily routines. Establishing a consistent sleep schedule is paramount; going to bed and waking up at the same time each day helps regulate the body’s internal clock. This consistency reinforces natural circadian rhythms, promoting more restorative sleep cycles.
Creating an optimal sleep environment is equally important. The bedroom should be dark, quiet, and cool to facilitate relaxation and minimize disturbances during the night. Utilizing blackout curtains or eye masks can help block out light, while white noise machines or earplugs can mitigate disruptive sounds.
Additionally, limiting exposure to screens before bedtime is crucial; blue light emitted from devices can interfere with melatonin production, making it harder to fall asleep. Incorporating relaxation techniques into pre-sleep routines can also enhance sleep quality. Practices such as mindfulness meditation, deep breathing exercises, or gentle yoga can help reduce stress levels and prepare the mind for rest.
Furthermore, being mindful of dietary choices is essential; avoiding large meals, caffeine, and alcohol close to bedtime can prevent disruptions in sleep patterns.
Conclusion and Future Research
The intricate relationship between sleep quality and overall health underscores the necessity for continued research in this field. As our understanding of the mechanisms underlying sleep improves, so too does our ability to develop targeted interventions for those suffering from poor sleep quality. Future studies should focus on exploring the long-term effects of various lifestyle modifications on sleep patterns as well as investigating the efficacy of emerging treatments for specific sleep disorders.
Additionally, there is a growing need for research that examines the impact of technology on sleep quality. With the increasing prevalence of wearable devices designed to monitor sleep patterns, understanding how these technologies influence behavior and perceptions of sleep will be crucial in developing effective strategies for improving overall well-being.
Resources for Improving Sleep Quality
Numerous resources are available for individuals seeking to enhance their sleep quality. Books such as “Why We Sleep” by Matthew Walker provide comprehensive insights into the science of sleep and practical tips for improving restfulness. Online platforms like the National Sleep Foundation offer valuable information on various aspects of sleep health, including tips for better sleeping habits and resources for finding professional help.
Mobile applications designed for tracking sleep patterns can also be beneficial; apps like Sleep Cycle or Calm provide users with tools to monitor their sleeping habits while offering guided meditations or relaxation techniques to promote better rest. Furthermore, consulting with healthcare professionals specializing in sleep medicine can provide personalized recommendations tailored to individual needs. In conclusion, understanding the complexities surrounding sleep quality is essential for fostering better health outcomes across populations.
By addressing common disorders through clinical methodologies and implementing evidence-based recommendations for improvement, individuals can take proactive steps toward achieving restorative rest that enhances their overall well-being.




