Schizophrenia is a complex and often misunderstood mental disorder that affects how a person thinks, feels, and behaves. Characterized by a range of symptoms, including delusions, hallucinations, disorganized thinking, and impaired functioning, schizophrenia can significantly disrupt an individual’s ability to lead a normal life. The onset of this disorder typically occurs in late adolescence or early adulthood, although it can manifest at any age.
The exact cause of schizophrenia remains elusive, but it is believed to result from a combination of genetic, biological, and environmental factors. The stigma surrounding schizophrenia often exacerbates the challenges faced by those diagnosed, leading to social isolation and discrimination. The prevalence of schizophrenia is estimated to be around 1% of the global population, making it a significant public health concern.
Individuals with schizophrenia may experience episodes of psychosis, which can lead to severe disruptions in their daily lives. The disorder not only affects the individual but also has profound implications for families and communities. Understanding schizophrenia requires a multifaceted approach that encompasses biological, psychological, and social dimensions.
As research continues to evolve, it is crucial to explore the current treatment options available and the ongoing efforts to improve outcomes for those affected by this debilitating condition.
Key Takeaways
- Schizophrenia is a complex mental disorder requiring ongoing research for better treatments.
- Current treatments include antipsychotic medications but have limitations and side effects.
- Clinical trials are crucial for developing and validating new schizophrenia therapies.
- Recent trials have identified promising new treatments that may improve patient outcomes.
- Future research aims to overcome challenges in trials and enhance care for patients and caregivers.
Current Treatment Options for Schizophrenia
The treatment landscape for schizophrenia has evolved significantly over the past few decades, primarily focusing on pharmacological interventions and psychosocial therapies. Antipsychotic medications are the cornerstone of treatment for schizophrenia, with two main categories: typical (first-generation) and atypical (second-generation) antipsychotics. Typical antipsychotics, such as haloperidol and chlorpromazine, primarily target dopamine receptors in the brain to alleviate positive symptoms like hallucinations and delusions.
However, they often come with a range of side effects, including extrapyramidal symptoms and tardive dyskinesia. Atypical antipsychotics, including risperidone, olanzapine, and aripiprazole, have gained prominence due to their broader efficacy in treating both positive and negative symptoms while generally presenting a more favorable side effect profile. These medications work on multiple neurotransmitter systems, including serotonin and dopamine pathways.
Despite their advantages, adherence to medication remains a significant challenge for many patients due to side effects or lack of insight into their illness. Therefore, integrating psychosocial interventions such as cognitive-behavioral therapy (CBT), family therapy, and supported employment programs is essential in providing comprehensive care that addresses both the biological and psychosocial aspects of schizophrenia.
Importance of Clinical Trials in Advancing Schizophrenia Treatment
Clinical trials play a pivotal role in advancing our understanding of schizophrenia and improving treatment options. These carefully designed studies are essential for evaluating the safety and efficacy of new medications and therapeutic approaches. By systematically testing hypotheses in controlled environments, clinical trials provide valuable data that can lead to regulatory approval and clinical practice changes.
The rigorous methodology employed in these trials ensures that findings are reliable and can be generalized to broader populations. Moreover, clinical trials offer hope to patients who may have exhausted existing treatment options. Participation in these studies can provide access to cutting-edge therapies that are not yet available on the market.
Additionally, clinical trials often include comprehensive assessments of participants’ mental health status, which can lead to improved monitoring and management of symptoms. The collaborative nature of clinical trials also fosters partnerships between researchers, healthcare providers, and patients, creating a shared commitment to finding effective solutions for those living with schizophrenia.
Recent Breakthroughs in Schizophrenia Clinical Trials
Recent years have witnessed significant breakthroughs in clinical trials aimed at treating schizophrenia. One notable advancement is the development of novel antipsychotic medications that target specific neurotransmitter systems beyond dopamine. For instance, drugs like pimavanserin have shown promise in addressing negative symptoms associated with schizophrenia by modulating serotonin receptors.
This represents a shift towards more targeted therapies that aim to improve the overall quality of life for patients rather than merely alleviating acute symptoms. Another area of progress is the exploration of long-acting injectable formulations of antipsychotic medications. These formulations can enhance adherence by reducing the frequency of dosing required compared to oral medications.
Studies have demonstrated that long-acting injectables can lead to better outcomes in terms of symptom management and reduced hospitalizations. Furthermore, research into adjunctive therapies such as cognitive remediation therapy has gained traction, showing potential in improving cognitive deficits often experienced by individuals with schizophrenia. These breakthroughs highlight the dynamic nature of schizophrenia research and the ongoing efforts to refine treatment strategies.
Promising New Therapies for Schizophrenia
| Metric | Value | Description |
|---|---|---|
| Number of Clinical Trials | 1,200+ | Total registered clinical trials related to schizophrenia |
| Phases Distribution | Phase 1: 15%, Phase 2: 40%, Phase 3: 35%, Phase 4: 10% | Percentage of trials in each clinical phase |
| Average Trial Duration | 18 months | Mean length of clinical trials from start to completion |
| Common Primary Outcomes | Symptom reduction, cognitive improvement, relapse rate | Typical endpoints measured in schizophrenia trials |
| Sample Size Range | 30 – 500 participants | Typical number of participants enrolled per trial |
| Geographic Distribution | North America: 45%, Europe: 35%, Asia: 15%, Others: 5% | Location of clinical trial sites worldwide |
| Intervention Types | Pharmacological: 70%, Behavioral: 20%, Combined: 10% | Types of interventions tested in trials |
| Completion Rate | 65% | Percentage of trials completed as planned |
In addition to pharmacological advancements, several promising new therapies are emerging in the field of schizophrenia treatment. One such approach is the use of neuromodulation techniques, including transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT). TMS involves non-invasive stimulation of specific brain regions and has shown potential in reducing symptoms in treatment-resistant cases of schizophrenia.
ECT, while traditionally associated with severe depression, is being re-evaluated for its efficacy in managing acute psychotic episodes. Furthermore, there is growing interest in the role of psychosocial interventions that incorporate technology. Digital therapeutics and mobile health applications are being developed to provide real-time support for individuals with schizophrenia.
These tools can facilitate symptom tracking, medication reminders, and access to therapeutic resources, thereby enhancing patient engagement and self-management. As research continues to explore these innovative approaches, there is hope for more personalized treatment options that cater to the unique needs of individuals living with schizophrenia.
Challenges and Limitations in Schizophrenia Clinical Trials
Despite the advancements made in schizophrenia research, several challenges and limitations persist within clinical trials. One significant hurdle is the heterogeneity of schizophrenia itself; the disorder manifests differently across individuals, making it difficult to establish standardized treatment protocols. This variability can complicate recruitment efforts for clinical trials, as specific subgroups may be underrepresented or excluded based on stringent eligibility criteria.
Additionally, the stigma associated with mental illness can deter potential participants from enrolling in clinical trials. Many individuals may fear being labeled or judged due to their diagnosis, leading to lower participation rates. Furthermore, issues related to informed consent can arise when dealing with populations experiencing severe cognitive impairments or psychosis.
Researchers must navigate these ethical considerations carefully while ensuring that participants fully understand the implications of their involvement in clinical studies.
Future Directions in Schizophrenia Research
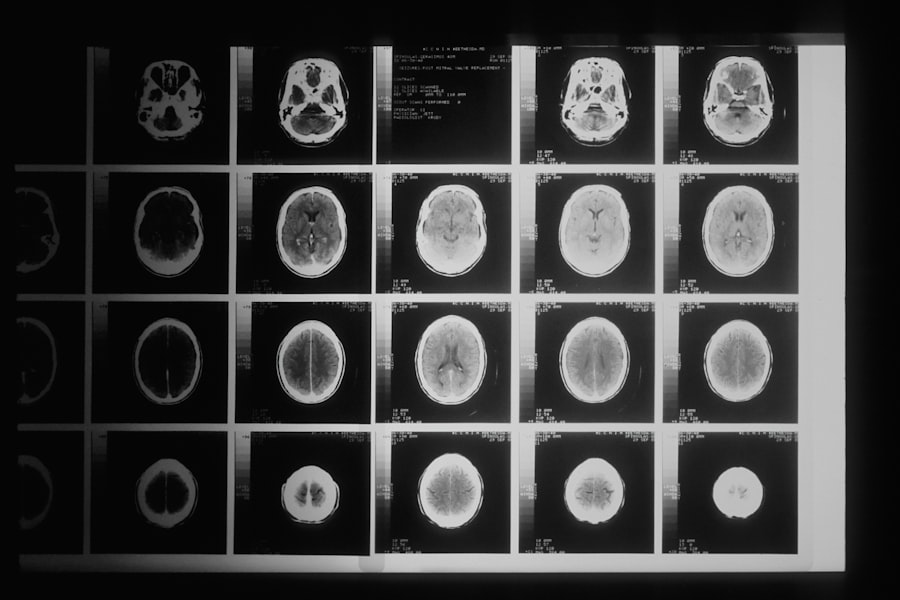
Looking ahead, future directions in schizophrenia research are likely to focus on several key areas aimed at improving treatment outcomes and understanding the underlying mechanisms of the disorder. One promising avenue is the exploration of biomarkers that could aid in early diagnosis and personalized treatment strategies. Identifying specific genetic or neurobiological markers associated with schizophrenia could enable clinicians to tailor interventions based on an individual’s unique profile.
Moreover, there is an increasing emphasis on integrating multidisciplinary approaches that combine pharmacological treatments with psychosocial support systems. Research into holistic models of care that address not only the biological aspects but also the social determinants of health will be crucial in improving overall patient outcomes. Additionally, advancements in neuroimaging techniques may provide deeper insights into brain function and connectivity patterns associated with schizophrenia, paving the way for more targeted interventions.
Implications for Patients and Caregivers
The implications of ongoing research and advancements in schizophrenia treatment extend beyond clinical settings; they profoundly impact patients and caregivers alike. For individuals living with schizophrenia, access to innovative therapies can lead to improved symptom management and enhanced quality of life. As new treatments emerge from clinical trials, patients may experience fewer side effects and better overall functioning.
For caregivers, understanding the evolving landscape of schizophrenia treatment is essential for providing effective support. Caregivers often play a critical role in managing their loved ones’ care and navigating complex healthcare systems. As new therapies become available, caregivers must stay informed about potential benefits and challenges associated with these treatments.
Furthermore, fostering open communication between patients, caregivers, and healthcare providers will be vital in ensuring that treatment plans align with individual needs and preferences. In conclusion, while significant strides have been made in understanding and treating schizophrenia, ongoing research remains essential for addressing the complexities of this disorder. The collaborative efforts between researchers, clinicians, patients, and caregivers will continue to shape the future landscape of schizophrenia treatment and improve outcomes for those affected by this challenging condition.




