Inborn errors of metabolism, particularly those affecting the liver, have garnered significant attention in the realm of clinical research, with a focus on conditions such as Intrahepatic Cholestasis (ICH). ICH is characterized by impaired bile flow due to dysfunction within the liver, leading to a buildup of bile acids in the bloodstream. This condition can manifest in various forms, including genetic disorders and drug-induced liver injury, and it poses a considerable challenge for healthcare providers.
The complexity of ICH necessitates a multidisciplinary approach to research, encompassing genetics, hepatology, pharmacology, and patient care. Clinical research in ICH aims to unravel the underlying mechanisms of the disease, improve diagnostic methods, and develop effective treatment strategies. The importance of this research cannot be overstated, as ICH can lead to severe complications such as liver failure, cirrhosis, and even death if left untreated.
As researchers delve deeper into the pathophysiology of ICH, they are uncovering potential therapeutic targets that could revolutionize treatment options for affected individuals. This article will explore the historical context of ICH treatment, current challenges faced by clinicians, recent advancements in research, and the future directions that hold promise for improving patient outcomes.
Key Takeaways
- Ich clinical research focuses on improving treatment for the parasitic disease Ichthyophthirius multifiliis.
- Historical treatments have been limited and often ineffective against Ich infections.
- Current challenges include drug resistance and limited effective therapies.
- Recent advancements involve new medications and innovative treatment approaches.
- Ongoing clinical trials aim to enhance patient outcomes and guide future Ich treatment strategies.
Historical Background of Ich Treatment
The understanding of ICH has evolved significantly over the decades. Historically, the condition was often misdiagnosed or overlooked due to its nonspecific symptoms, which can include jaundice, pruritus, and fatigue. Early medical literature primarily focused on the clinical presentation rather than the underlying causes.
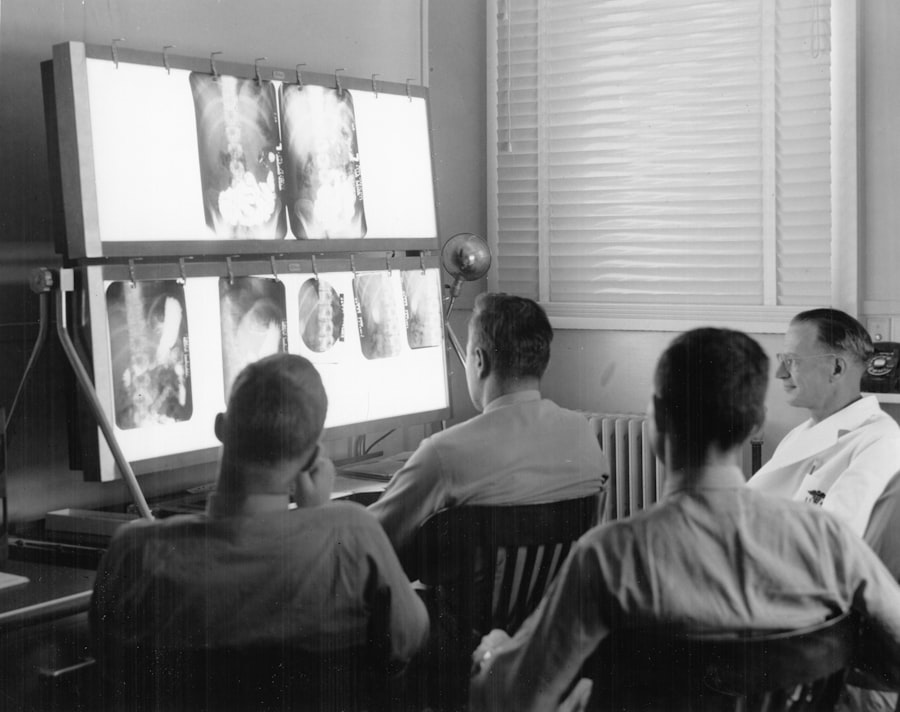
It wasn’t until the mid-20th century that researchers began to identify specific genetic mutations associated with hereditary forms of ICH, such as Progressive Familial Intrahepatic Cholestasis (PFIC). These discoveries laid the groundwork for more targeted approaches to diagnosis and treatment. In the latter half of the 20th century, advancements in imaging techniques and liver biopsy procedures allowed for better assessment of liver function and structure.
This period also saw the introduction of pharmacological interventions aimed at alleviating symptoms associated with bile acid accumulation. Ursodeoxycholic acid (UDCA) emerged as a cornerstone therapy for certain types of cholestasis, demonstrating efficacy in improving liver function tests and reducing pruritus. However, these treatments were often limited in their effectiveness and did not address the root causes of ICH.
As our understanding of the genetic basis of these disorders expanded, so too did the potential for more innovative therapeutic strategies.
Current Challenges in Ich Treatment
Despite advancements in our understanding of ICH, significant challenges remain in its treatment. One of the primary obstacles is the heterogeneity of the condition; ICH can arise from various etiologies, including genetic mutations, autoimmune diseases, and drug-induced liver injury. This diversity complicates diagnosis and necessitates a tailored approach to treatment.
Clinicians often face difficulties in identifying the specific cause of cholestasis in patients, which can delay appropriate management and lead to adverse outcomes. Moreover, existing therapies are not universally effective. While UDCA has shown promise for some patients, it does not work for everyone and may not prevent disease progression in more severe cases.
The lack of approved therapies specifically targeting the underlying mechanisms of ICH means that many patients are left with limited options. Additionally, there is a pressing need for better biomarkers to monitor disease progression and response to treatment. Current methods often rely on subjective assessments and laboratory tests that may not accurately reflect the patient’s condition or predict outcomes.
Advancements in Ich Treatment Research
Recent years have witnessed significant advancements in ICH treatment research, driven by a deeper understanding of the molecular mechanisms underlying cholestasis. Researchers are increasingly focusing on genetic studies to identify novel mutations associated with various forms of ICH. For instance, whole-exome sequencing has revealed previously unrecognized genetic variants that contribute to cholestatic liver diseases.
These findings not only enhance our understanding of disease pathogenesis but also pave the way for potential gene-targeted therapies. In addition to genetic insights, advancements in pharmacology have led to the exploration of new therapeutic agents that target specific pathways involved in bile acid metabolism. For example, research into farnesoid X receptor (FXR) agonists has shown promise in preclinical models of cholestasis.
FXR plays a crucial role in regulating bile acid synthesis and transport; thus, modulating its activity could offer a novel approach to managing ICH. Clinical trials investigating these new agents are underway, providing hope for more effective treatments that address the underlying causes of cholestasis rather than merely alleviating symptoms.
New Therapies and Medications for Ich
| Metric | Description | Typical Values / Standards |
|---|---|---|
| ICH GCP Compliance Rate | Percentage of clinical trials adhering to ICH Good Clinical Practice guidelines | ≥ 95% |
| Protocol Deviation Rate | Frequency of deviations from the approved clinical trial protocol | < 5% of total enrolled subjects |
| Adverse Event Reporting Time | Time taken to report serious adverse events (SAEs) as per ICH E2A guidelines | Within 24 hours of awareness |
| Subject Enrollment Rate | Number of subjects enrolled per month in ICH-compliant trials | Varies by study phase and indication |
| Data Query Resolution Time | Average time to resolve data queries in clinical trial databases | ≤ 7 days |
| Inspection Findings | Number of critical and major findings during regulatory inspections | Zero critical; minimal major findings |
| Informed Consent Compliance | Percentage of subjects with properly documented informed consent | 100% |
The landscape of ICH treatment is evolving with the introduction of new therapies and medications designed to target specific aspects of bile acid metabolism and liver function. One notable example is obeticholic acid (OCA), an FXR agonist that has shown promise in clinical trials for patients with primary biliary cholangitis (PBC) and other cholestatic liver diseases. OCA works by enhancing bile acid clearance and reducing inflammation within the liver, leading to improved liver function tests and symptom relief.
Another area of exploration involves the use of novel bile acid modulators that aim to restore normal bile flow and reduce toxicity associated with bile acid accumulation. These agents are being investigated for their potential to improve outcomes in patients with both hereditary and acquired forms of ICH. Additionally, researchers are exploring combination therapies that leverage multiple mechanisms of action to achieve better results than monotherapy alone.
Such approaches may be particularly beneficial for patients with complex presentations or those who have not responded adequately to existing treatments.
Clinical Trials and Studies in Ich Treatment

Clinical trials play a pivotal role in advancing our understanding of ICH treatment and evaluating the safety and efficacy of new therapies. Numerous studies are currently underway to assess emerging treatments for various forms of cholestasis. For instance, trials investigating the use of OCA have demonstrated promising results in improving liver biochemistry and reducing pruritus in patients with PBThese findings underscore the importance of rigorous clinical research in establishing evidence-based treatment protocols.
Moreover, ongoing studies are exploring the potential benefits of gene therapy for hereditary forms of ICH. By targeting specific genetic mutations responsible for cholestasis, researchers hope to develop curative approaches that address the root cause rather than merely managing symptoms. The advent of CRISPR technology has opened new avenues for gene editing, allowing for precise modifications that could potentially correct genetic defects associated with ICH.
As these trials progress, they hold the potential to reshape the treatment landscape for patients suffering from this challenging condition.
Future Directions in Ich Treatment Research
Looking ahead, several promising directions are emerging in ICH treatment research that could significantly impact patient care. One key area is personalized medicine, which aims to tailor treatment strategies based on an individual’s genetic profile and disease characteristics. By identifying specific mutations or biomarkers associated with different forms of ICH, clinicians can develop targeted therapies that are more likely to be effective for each patient.
Additionally, there is growing interest in exploring the gut-liver axis and its role in cholestasis. The microbiome has been implicated in various liver diseases, and researchers are investigating how alterations in gut flora may influence bile acid metabolism and liver function. Understanding these interactions could lead to novel therapeutic approaches that leverage dietary modifications or probiotics to improve outcomes for patients with ICH.
Impact of Advancements in Ich Treatment on Patient Outcomes
The advancements in ICH treatment research have profound implications for patient outcomes. As new therapies emerge that target the underlying mechanisms of cholestasis, patients may experience improved quality of life and reduced risk of complications associated with chronic liver disease. Enhanced diagnostic tools and biomarkers will enable earlier detection and intervention, potentially preventing disease progression and improving long-term prognosis.
Furthermore, as clinical trials yield positive results for novel therapies, there is hope for more effective management strategies that can be integrated into routine clinical practice. The shift towards personalized medicine will empower clinicians to make informed decisions based on individual patient profiles, leading to more tailored and effective treatment plans. Ultimately, these advancements hold the promise of transforming the landscape of ICH treatment, offering renewed hope for patients facing this challenging condition and their families.




