Clinical trial supply management is a critical component of the clinical research process, ensuring that the necessary materials, including investigational drugs, placebos, and other medical supplies, are available when and where they are needed. The complexity of clinical trials, which often span multiple sites and involve diverse patient populations, necessitates a well-coordinated supply chain strategy. Effective management of these supplies is essential not only for the integrity of the trial but also for the safety and well-being of participants.
As the pharmaceutical and biotechnology industries continue to evolve, the demand for efficient clinical trial supply management has become increasingly pronounced. The landscape of clinical trials is marked by rapid advancements in technology, regulatory changes, and shifting patient demographics. These factors contribute to the growing complexity of supply chain logistics.
Clinical trial supply management encompasses a wide range of activities, including demand forecasting, inventory control, distribution logistics, and compliance with regulatory requirements. Each of these elements plays a vital role in ensuring that trials can proceed smoothly and that data collected is reliable and valid. As such, understanding the intricacies of clinical trial supply management is essential for stakeholders involved in the research process.
Key Takeaways
- Effective clinical trial supply management is crucial for the success of clinical studies.
- Common challenges include demand variability, regulatory compliance, and logistical complexities.
- Accurate forecasting and strategic planning help prevent supply shortages and excess inventory.
- Leveraging technology enhances tracking, data management, and overall supply chain efficiency.
- Strong collaboration and adherence to regulatory requirements ensure smooth trial operations and compliance.
Challenges in Clinical Trial Supply Management
One of the primary challenges in clinical trial supply management is the unpredictability of patient enrollment and retention rates. Trials often experience fluctuations in participant numbers due to various factors such as eligibility criteria, patient willingness, and competing studies. This unpredictability can lead to either surplus or shortage of supplies, which can significantly impact the trial’s timeline and budget.
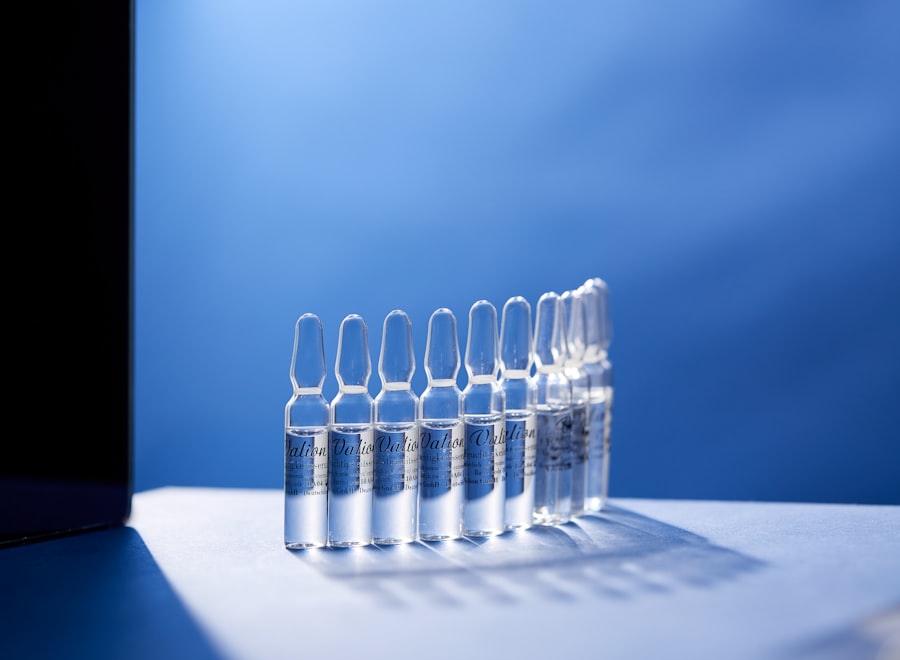
For instance, if a trial enrolls more patients than anticipated, there may not be enough investigational product available to meet demand, potentially delaying the study or compromising its integrity. Another significant challenge is the complexity of global supply chains. Many clinical trials are conducted across multiple countries and regions, each with its own regulatory requirements and logistical hurdles.
This can complicate the procurement and distribution of supplies, as companies must navigate customs regulations, import/export restrictions, and varying storage conditions. For example, temperature-sensitive products may require specialized shipping methods to maintain their efficacy, adding another layer of complexity to supply chain management. Additionally, language barriers and cultural differences can further complicate communication between stakeholders involved in the supply chain.
Strategies for Efficient Clinical Trial Supply Management

To address the challenges inherent in clinical trial supply management, organizations can implement several strategies aimed at enhancing efficiency and effectiveness. One such strategy is the development of a comprehensive supply chain plan that outlines all aspects of the supply process from start to finish. This plan should include detailed timelines for production, packaging, labeling, and distribution, as well as contingency plans for potential disruptions.
By having a clear roadmap in place, organizations can better anticipate challenges and respond proactively. Another effective strategy is to leverage real-time data analytics for demand forecasting. By analyzing historical data from previous trials and current enrollment trends, organizations can make more informed predictions about supply needs.
Advanced analytics tools can help identify patterns in patient recruitment and retention, allowing for more accurate estimates of required supplies. This data-driven approach not only minimizes waste but also ensures that supplies are available when needed, ultimately supporting the trial’s success.
Importance of Forecasting and Planning in Clinical Trial Supply Management
Forecasting and planning are foundational elements of successful clinical trial supply management. Accurate forecasting allows organizations to anticipate demand for investigational products and other supplies based on various factors such as patient enrollment rates, site activation timelines, and historical data from similar trials. Effective planning ensures that these forecasts translate into actionable strategies that align with the overall objectives of the clinical trial.
The importance of forecasting extends beyond mere inventory management; it also plays a crucial role in budgetary considerations. By accurately predicting supply needs, organizations can allocate resources more effectively and avoid unnecessary expenditures associated with overproduction or expedited shipping costs due to last-minute shortages. Furthermore, robust forecasting can enhance collaboration among stakeholders by providing a shared understanding of supply needs and timelines, fostering a more cohesive approach to trial execution.
Utilizing Technology in Clinical Trial Supply Management
| Metric | Description | Typical Value/Range | Importance |
|---|---|---|---|
| Inventory Accuracy | Percentage of clinical trial supplies accurately recorded in inventory system | 95% – 99% | High – Ensures correct supply levels and reduces risk of shortages or overstock |
| On-Time Delivery Rate | Percentage of clinical trial supplies delivered on or before scheduled date | 90% – 98% | High – Critical for maintaining trial timelines and patient dosing schedules |
| Supply Utilization Rate | Ratio of used supplies to total supplied for the trial | 80% – 95% | Medium – Helps optimize supply quantities and reduce waste |
| Temperature Excursion Incidents | Number of times clinical supplies were exposed to temperatures outside specified range | 0 – 2 per trial phase | High – Affects drug stability and trial integrity |
| Cycle Time for Resupply | Average time taken to replenish clinical trial supplies after request | 3 – 7 days | Medium – Impacts continuity of trial operations |
| Expiry Management Accuracy | Percentage of supplies used or removed before expiry date | 98% – 100% | High – Prevents use of expired materials and reduces waste |
| Returns Processing Time | Average time to process and reconcile returned clinical supplies | 5 – 10 days | Medium – Important for inventory accuracy and cost control |
The integration of technology into clinical trial supply management has revolutionized how organizations approach logistics and inventory control. Advanced software solutions enable real-time tracking of supplies throughout the supply chain, providing visibility into inventory levels at various sites. This transparency allows for timely decision-making regarding restocking or redistribution of supplies as needed.
Moreover, technology facilitates better communication among stakeholders involved in clinical trials. Cloud-based platforms enable seamless sharing of information between sponsors, contract research organizations (CROs), and clinical sites. This collaborative environment enhances coordination efforts and minimizes the risk of miscommunication or delays in supply delivery.
Additionally, electronic data capture (EDC) systems can streamline data collection processes, ensuring that information related to supply usage is accurately recorded and readily accessible for analysis.
Best Practices for Inventory Management in Clinical Trials
Effective inventory management is paramount in clinical trial supply management to ensure that supplies are available when needed while minimizing waste and costs. One best practice is implementing a just-in-time (JIT) inventory system that aligns supply deliveries with actual demand rather than relying on bulk orders that may lead to excess stock. JIT systems reduce storage costs and decrease the risk of product expiration or obsolescence.
Another best practice involves conducting regular audits of inventory levels to maintain accuracy and accountability. These audits help identify discrepancies between recorded inventory and actual stock on hand, allowing organizations to address issues promptly. Additionally, establishing clear protocols for inventory handling—such as labeling, storage conditions, and expiration date tracking—can further enhance inventory management practices.
Collaboration and Communication in Clinical Trial Supply Management
Collaboration among stakeholders is essential for effective clinical trial supply management. The complexity of clinical trials often requires input from various parties, including sponsors, CROs, clinical sites, and suppliers. Establishing strong lines of communication among these groups fosters a collaborative environment where challenges can be addressed collectively.
Regular meetings and updates can facilitate information sharing regarding enrollment progress, supply needs, and any potential issues that may arise during the trial. Utilizing collaborative tools such as project management software can enhance communication by providing a centralized platform for tracking tasks, deadlines, and responsibilities. By fostering a culture of collaboration and open communication, organizations can improve their ability to respond to challenges swiftly and effectively.
Regulatory Considerations in Clinical Trial Supply Management
Navigating regulatory requirements is a critical aspect of clinical trial supply management that cannot be overlooked. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) impose strict guidelines on the handling and distribution of investigational products to ensure participant safety and data integrity.
Organizations must remain vigilant in adhering to these regulations throughout the supply chain process. Compliance with Good Manufacturing Practice (GMP) standards is essential when producing investigational products for clinical trials. This includes ensuring that facilities are properly maintained, staff are adequately trained, and quality control measures are in place to prevent contamination or errors during production.
Additionally, organizations must be prepared for inspections by regulatory authorities at any stage of the trial process, necessitating thorough documentation and record-keeping practices to demonstrate compliance with all applicable regulations. In conclusion, clinical trial supply management is a multifaceted discipline that requires careful planning, strategic execution, and ongoing collaboration among stakeholders. By addressing challenges through effective strategies, leveraging technology for enhanced efficiency, adhering to best practices in inventory management, fostering communication among teams, and navigating regulatory requirements diligently, organizations can optimize their clinical trial supply chains to support successful research outcomes.




