Clinical trials are a cornerstone of modern medical research, serving as the primary method for evaluating the safety and efficacy of new treatments, drugs, and medical devices. These trials are meticulously designed studies that involve human participants and are conducted in phases, each with specific objectives and methodologies. The process begins with preclinical research, where potential treatments are tested in laboratories and on animal models.
Once a treatment shows promise, it moves into clinical trials, which are divided into several phases: Phase I focuses on safety and dosage, Phase II assesses efficacy and side effects, and Phase III compares the new treatment against standard therapies in larger populations. The significance of clinical trials extends beyond the mere testing of new therapies; they are essential for advancing medical knowledge and improving patient care. By systematically gathering data on how new interventions perform in real-world settings, researchers can identify not only the benefits but also the risks associated with new treatments.
This rigorous process ensures that only those therapies that demonstrate a favorable risk-benefit profile are approved for widespread use. Moreover, clinical trials often provide patients access to cutting-edge treatments that are not yet available to the general public, offering hope in situations where conventional therapies have failed.
Key Takeaways
- Clinical trials are essential for advancing medical knowledge and treatments.
- Negative or sad trial results can significantly affect patients and their families emotionally.
- Ethical considerations are crucial in conducting and reporting clinical trials responsibly.
- Unsuccessful trials provide valuable lessons that guide future research directions.
- Supporting patients and families during difficult outcomes is a key aspect of clinical care.
Importance of Clinical Trial Results
The results of clinical trials hold immense importance for various stakeholders, including patients, healthcare providers, regulatory agencies, and pharmaceutical companies. For patients, trial outcomes can mean the difference between life and death, particularly in the context of life-threatening diseases such as cancer or rare genetic disorders. Positive results can lead to the approval of new therapies that significantly improve survival rates or quality of life.
Conversely, negative results can halt the development of a treatment that may have seemed promising in earlier stages, thereby preventing potential harm to patients. Healthcare providers rely on clinical trial results to inform their treatment decisions. Evidence-based medicine is predicated on the availability of robust data from clinical trials that demonstrate the effectiveness of interventions.
When physicians understand the outcomes of various treatments through well-conducted trials, they can make informed choices that align with the best interests of their patients. Regulatory agencies like the Food and Drug Administration (FDA) or the European Medicines Agency (EMA) depend on these results to evaluate whether a new drug or therapy should be approved for public use. The integrity and transparency of clinical trial results are thus critical for maintaining public trust in medical advancements.
Unfortunate Outcome: Sad Clinical Trial Results
Despite the rigorous design and execution of clinical trials, not all studies yield positive outcomes. In fact, many trials end with disappointing results that can be disheartening for researchers and participants alike. For instance, a high-profile clinical trial for a promising Alzheimer’s drug may show initial signs of efficacy in early phases but ultimately fail to demonstrate significant benefits in larger populations during Phase III trials.
Such outcomes can lead to substantial financial losses for pharmaceutical companies and may also discourage further investment in similar research avenues. The emotional toll of sad clinical trial results extends beyond the research community; it profoundly affects participants who have placed their hopes in these studies. Many individuals enroll in clinical trials out of desperation for effective treatments when conventional options have been exhausted.
When a trial fails, it can feel like a personal loss, not just for the participants but also for their families who have supported them throughout the process. The disappointment can lead to feelings of hopelessness and frustration, particularly when patients have invested time and energy into being part of a study that ultimately does not yield the anticipated benefits.
Impact on Patients and Families
The impact of unsuccessful clinical trial results on patients and their families is multifaceted and often profound. For patients who participated in trials with high hopes for a breakthrough treatment, the news of failure can lead to emotional distress and a sense of betrayal. Many participants may have experienced side effects or endured invasive procedures during the trial, all in pursuit of a potential cure or improvement in their condition.
When these efforts do not result in positive outcomes, it can lead to feelings of disillusionment with the medical system and a loss of trust in future research endeavors. Families also bear the brunt of these disappointing results. They often serve as caregivers and emotional support systems for patients navigating complex health challenges.
When a trial fails, family members may feel helpless as they witness their loved ones grappling with renewed uncertainty about their health. The psychological burden can be significant; families may experience anxiety about future treatment options or fear that they have exhausted all avenues for effective care. This emotional strain can lead to increased stress within family dynamics, as members cope with their own feelings of loss while trying to support one another.
Ethical Considerations in Clinical Trials
| Metric | Description | Value | Unit |
|---|---|---|---|
| Trial Phase | Stage of the clinical trial | Phase 2 | – |
| Number of Participants | Total enrolled subjects | 150 | patients |
| Primary Endpoint | Measure of treatment efficacy | Reduction in depressive symptoms | – |
| Baseline Severity Score | Average initial depression rating | 28 | HAM-D points |
| Improvement at 12 weeks | Change in depression score from baseline | 8 | HAM-D points |
| Response Rate | Percentage of patients with significant improvement | 45 | % |
| Adverse Event Rate | Percentage of patients experiencing side effects | 20 | % |
| Dropout Rate | Percentage of participants who discontinued | 10 | % |
The ethical landscape surrounding clinical trials is complex and requires careful navigation to protect participants’ rights and well-being. Informed consent is a fundamental ethical principle that mandates researchers provide potential participants with comprehensive information about the trial’s purpose, procedures, risks, and benefits before enrollment. This process ensures that individuals can make educated decisions about their participation without coercion or undue influence.
However, ethical dilemmas can arise when participants are desperate for treatment options, potentially leading them to overlook risks associated with participation. Moreover, the ethical obligation to minimize harm extends beyond individual participants to encompass broader societal implications. Researchers must consider how trial failures might affect public perception of clinical research as a whole.
If negative results are not communicated transparently or if they lead to public distrust in medical research, it could hinder future studies and delay the development of potentially beneficial therapies. Balancing the pursuit of scientific knowledge with ethical responsibilities is crucial for maintaining integrity within the field of clinical research.
Lessons Learned from Unsuccessful Trials
Unsuccessful clinical trials often provide valuable lessons that can inform future research efforts. Each failed study contributes to a growing body of knowledge about disease mechanisms, treatment responses, and patient populations. For instance, if a trial investigating a new cancer drug fails due to unexpected side effects or lack of efficacy in certain demographics, researchers can analyze these outcomes to refine their hypotheses and improve study designs in subsequent trials.
This iterative process is essential for advancing medical science and ensuring that future studies are better equipped to address the complexities of human health. Additionally, unsuccessful trials can prompt researchers to explore alternative approaches or therapeutic targets that may have been overlooked initially. For example, if a particular drug fails to show efficacy in treating a specific type of cancer, researchers might investigate whether it could be effective in combination with other therapies or in different cancer types altogether.
The insights gained from negative results can drive innovation and creativity within the research community, ultimately leading to breakthroughs that might not have been possible without those earlier failures.
Moving Forward: Future Implications for Research
The implications of both successful and unsuccessful clinical trials extend far beyond individual studies; they shape the future landscape of medical research and treatment development. As researchers analyze patterns from past trials—both positive and negative—they can identify gaps in knowledge that need addressing. This ongoing evaluation fosters an environment where adaptive trial designs become more prevalent, allowing researchers to modify protocols based on interim results rather than adhering rigidly to initial plans.
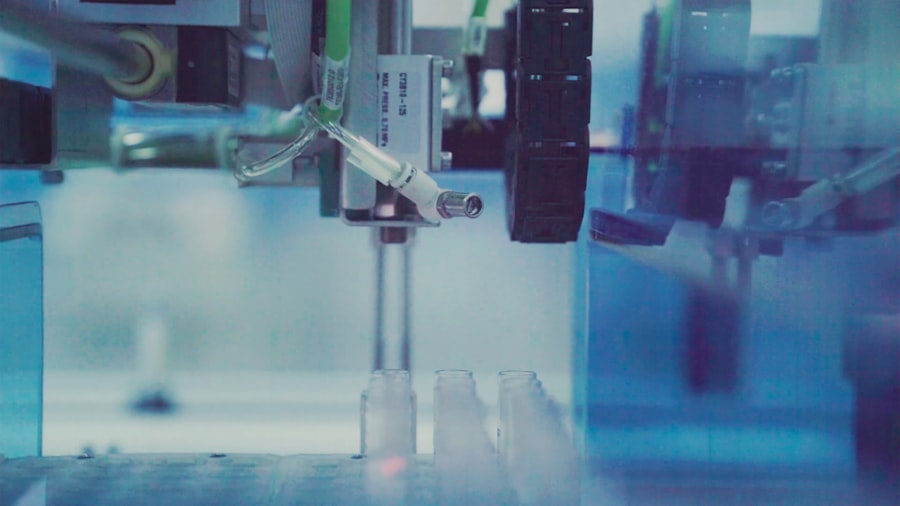
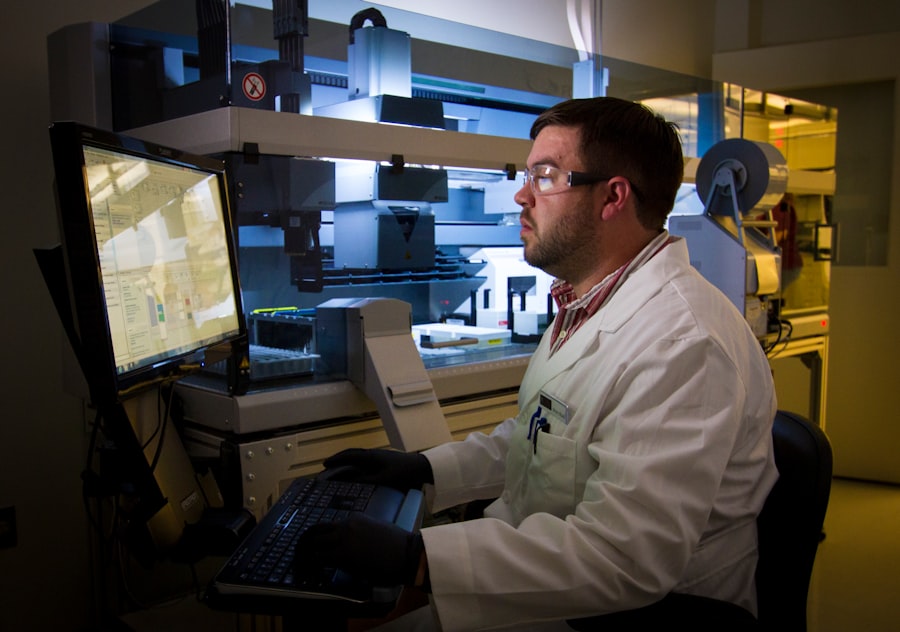
Moreover, advancements in technology and data analytics are revolutionizing how clinical trials are conducted. The integration of artificial intelligence (AI) and machine learning into trial design enables researchers to better predict patient responses based on genetic profiles or other biomarkers. This personalized approach holds promise for increasing the likelihood of successful outcomes while minimizing risks associated with ineffective treatments.
As the field evolves, embracing innovative methodologies will be crucial for overcoming challenges posed by previous trial failures.
Supporting Patients and Families Through Difficult Results
In light of the emotional and psychological toll that disappointing clinical trial results can impose on patients and their families, it is essential to establish robust support systems that address their needs during these challenging times. Healthcare providers play a pivotal role in this process by offering compassionate communication when delivering difficult news. Providing clear explanations about what went wrong in a trial can help demystify the experience for patients and families while fostering an environment where they feel heard and understood.
Additionally, support groups and counseling services can be invaluable resources for individuals grappling with the aftermath of unsuccessful trials. Connecting patients with others who have faced similar experiences can create a sense of community and shared understanding that alleviates feelings of isolation. Mental health professionals specializing in chronic illness can also offer coping strategies tailored to help families navigate their emotional responses effectively.
By prioritizing holistic support for patients and families affected by sad clinical trial results, the healthcare community can help mitigate some of the distress associated with these experiences while fostering resilience moving forward.




