Early clinical development represents a critical phase in the journey of a new therapeutic agent from the laboratory bench to the bedside. This stage encompasses the initial human trials that assess the safety, tolerability, pharmacokinetics, and pharmacodynamics of a drug or treatment. Typically, this phase is divided into Phase I and Phase II clinical trials, where the primary focus is on understanding how a drug behaves in the human body and determining its potential efficacy.
The transition from preclinical studies, which often involve animal models and in vitro experiments, to early clinical development is a pivotal moment that can dictate the future of a drug candidate. The significance of early clinical development cannot be overstated. It is during this phase that researchers gather essential data that will inform subsequent stages of drug development.
The outcomes of these trials can lead to critical decisions regarding whether to continue, modify, or abandon a particular therapeutic approach. As such, early clinical development serves as a foundational pillar upon which the entire drug development process rests, influencing not only scientific and medical communities but also regulatory bodies and investors who are keenly interested in the viability of new treatments.
Key Takeaways
- Early clinical development is crucial for assessing the safety and efficacy of new medical treatments.
- It involves key stages such as preclinical studies, Phase I and II trials, and dose optimization.
- Regulatory authorities play a vital role in overseeing compliance and patient safety during early trials.
- Ethical considerations, including informed consent and risk minimization, are fundamental throughout the process.
- Emerging trends like adaptive trial designs and biomarker integration are shaping the future of early clinical development.
Importance of Early Clinical Development in Medicine
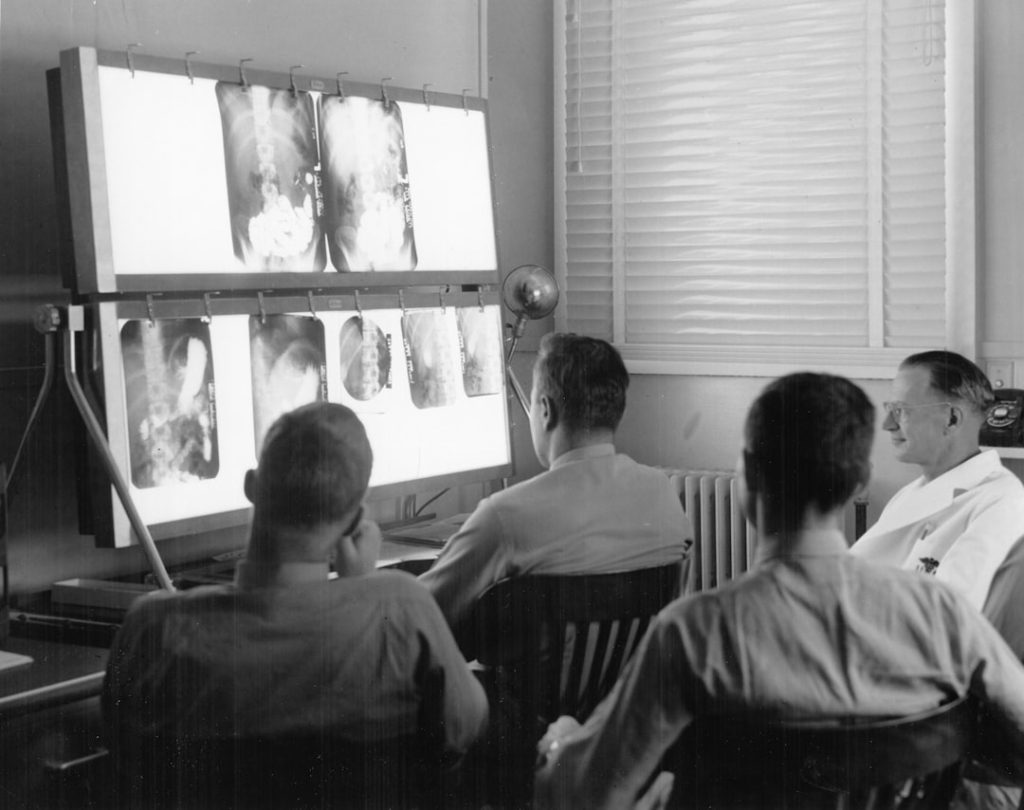
The importance of early clinical development lies in its role as a gatekeeper for drug candidates. It is during this phase that the first human data are collected, providing insights into how a drug interacts with biological systems. This information is crucial for determining whether a drug has the potential to be effective in treating specific conditions.
For instance, in oncology, early clinical trials often focus on identifying the maximum tolerated dose of a new chemotherapy agent while monitoring for adverse effects. The data gathered can help refine dosing regimens and inform subsequent studies aimed at establishing efficacy. Moreover, early clinical development plays a vital role in risk management.
By identifying safety concerns early on, researchers can make informed decisions about whether to proceed with further testing or to pivot their approach. For example, the withdrawal of certain drugs from the market due to unforeseen side effects underscores the necessity of rigorous early testing. The thalidomide tragedy of the 1960s serves as a historical reminder of the consequences of inadequate early clinical evaluation, leading to stricter regulations and more robust testing protocols in subsequent years.
Key Stages and Processes in Early Clinical Development

Early clinical development is characterized by several key stages, each with distinct objectives and methodologies. The first stage, Phase I trials, typically involves a small group of healthy volunteers or patients. The primary goal here is to assess safety and tolerability, often through escalating doses to determine the maximum tolerated dose (MTD).
Researchers closely monitor participants for adverse reactions and collect pharmacokinetic data to understand how the drug is absorbed, distributed, metabolized, and excreted by the body. Following successful Phase I trials, Phase II trials commence, focusing on evaluating the drug’s efficacy in a larger patient population. These trials are often designed as randomized controlled studies that compare the new treatment against a placebo or standard of care.
The outcomes measured can vary widely depending on the disease being targeted but typically include metrics such as tumor response rates in cancer studies or improvements in symptom scores for chronic conditions. This phase is crucial for establishing preliminary evidence of effectiveness and guiding further development.
Challenges and Considerations in Early Clinical Development
Despite its importance, early clinical development is fraught with challenges that can complicate the process. One significant hurdle is patient recruitment. Finding suitable participants who meet specific inclusion criteria can be time-consuming and may delay trial timelines.
Additionally, competition for patients among multiple studies can exacerbate recruitment difficulties. For instance, in rare diseases where patient populations are limited, researchers may struggle to enroll enough participants to achieve statistically significant results. Another challenge lies in the inherent uncertainty associated with early clinical trials.
The transition from preclinical success to human application does not always yield positive results. Many promising candidates fail during early trials due to unforeseen safety issues or lack of efficacy. This unpredictability necessitates a robust design and thorough planning to mitigate risks and optimize resource allocation.
Researchers must balance ambition with caution, ensuring that they are prepared for both success and failure as they navigate this complex landscape.
Role of Regulatory Authorities in Early Clinical Development
| Metric | Description | Typical Range/Value | Importance |
|---|---|---|---|
| Number of Compounds Screened | Total drug candidates evaluated in preclinical and early clinical phases | 50-200 | Identifies potential leads for further development |
| Phase 1 Trial Enrollment | Number of healthy volunteers or patients enrolled in Phase 1 studies | 20-100 subjects | Assesses safety and dosage |
| Time to First-in-Human (FIH) Study | Duration from preclinical completion to first human dosing | 12-24 months | Measures development speed |
| Adverse Event Rate | Percentage of subjects experiencing adverse events in Phase 1 | 10-30% | Evaluates safety profile |
| Pharmacokinetic (PK) Parameters | Key PK metrics such as half-life, Cmax, and AUC | Varies by compound | Determines drug absorption and clearance |
| Proof of Concept (PoC) Success Rate | Percentage of compounds demonstrating desired biological effect in early trials | 20-40% | Indicates potential efficacy |
| Time from Phase 1 to Phase 2 | Duration between completion of Phase 1 and start of Phase 2 trials | 6-12 months | Reflects development efficiency |
Regulatory authorities play an indispensable role in overseeing early clinical development processes. In the United States, the Food and Drug Administration (FDA) is responsible for ensuring that new drugs are safe and effective before they can be marketed to the public. Before initiating clinical trials, sponsors must submit an Investigational New Drug (IND) application that includes preclinical data, proposed trial protocols, and plans for monitoring safety.
Regulatory bodies also provide guidance on trial design and conduct, helping to ensure that studies adhere to ethical standards and scientific rigor. For example, they may require specific endpoints to be measured or suggest modifications to trial protocols based on emerging safety data. This oversight is crucial for maintaining public trust in the drug development process and ensuring that new therapies meet established safety and efficacy standards before reaching patients.
Ethical Considerations in Early Clinical Development

Ethical considerations are paramount in early clinical development, particularly given the vulnerability of trial participants. Informed consent is a cornerstone of ethical research practices; participants must be fully aware of the potential risks and benefits associated with their involvement in a study. Researchers are tasked with ensuring that consent forms are clear and comprehensible while providing adequate information about the study’s purpose, procedures, and any foreseeable risks.
Moreover, ethical dilemmas can arise when balancing scientific advancement with participant safety. For instance, researchers may face pressure to expedite trials due to competitive market dynamics or public health needs, such as during a pandemic. However, this urgency must not compromise ethical standards or participant welfare.
Institutional Review Boards (IRBs) play a critical role in reviewing study protocols to ensure that ethical considerations are adequately addressed before trials commence.
Emerging Trends and Innovations in Early Clinical Development
The landscape of early clinical development is continually evolving, driven by technological advancements and innovative methodologies. One notable trend is the increasing use of adaptive trial designs, which allow for modifications to trial protocols based on interim results. This flexibility can enhance efficiency by enabling researchers to make real-time adjustments to dosing regimens or patient populations based on emerging data.
Additionally, advancements in biomarker research are transforming early clinical development by enabling more precise patient stratification. By identifying specific genetic or molecular markers associated with disease response, researchers can tailor treatments to individual patients, potentially improving outcomes and reducing adverse effects. For example, targeted therapies in oncology often rely on biomarker identification to select patients most likely to benefit from specific treatments.
Future Directions in Early Clinical Development
Looking ahead, early clinical development is poised for further transformation as new technologies and methodologies continue to emerge. The integration of artificial intelligence (AI) and machine learning into trial design holds promise for optimizing patient selection and predicting outcomes based on historical data. These technologies can analyze vast datasets to identify patterns that may not be apparent through traditional analysis methods.
Moreover, the rise of decentralized clinical trials offers an innovative approach to conducting research outside traditional clinical settings. By leveraging telemedicine and remote monitoring technologies, researchers can reach broader patient populations while minimizing barriers related to travel and access. This shift could enhance patient engagement and retention while providing valuable data from diverse demographics.
As we move forward into an era characterized by rapid advancements in science and technology, early clinical development will continue to adapt and evolve. The ongoing collaboration between researchers, regulatory authorities, and ethical committees will be essential in navigating this complex landscape while ensuring that new therapies are developed responsibly and effectively for patients in need.