Clinical trials are a cornerstone of modern medicine, serving as the primary method for evaluating the safety and efficacy of new treatments, drugs, and medical devices. These trials are meticulously structured into distinct phases, each designed to answer specific research questions while ensuring the safety of participants. The journey of a new therapeutic agent from the laboratory bench to the patient’s bedside is fraught with challenges, and understanding the phases of clinical trials is essential for researchers, healthcare professionals, and patients alike.
Each phase builds upon the findings of the previous one, creating a comprehensive framework that guides the development of new medical interventions. The clinical trial process is not only a regulatory requirement but also a scientific necessity. It allows researchers to gather data that can inform medical practice and public health policy.
The phases of clinical trials—Phase 0, Phase I, Phase II, Phase III, and Phase IV—each serve a unique purpose in this continuum. By delineating these phases, stakeholders can better appreciate the rigorous evaluation that new therapies undergo before they reach the market. This understanding is crucial for informed decision-making regarding participation in clinical trials and for interpreting the results of these studies.
Key Takeaways
- Clinical trials progress through distinct phases to ensure drug safety and effectiveness.
- Phase 0 involves exploratory studies with very limited human exposure.
- Phase I focuses on determining safe dosage and identifying side effects.
- Phase II and III assess efficacy and involve larger participant groups for thorough testing.
- Phase IV monitors long-term effects after the drug is marketed, aiding informed healthcare decisions.
Phase 0: Exploratory Study
Phase 0 trials, often referred to as exploratory studies, represent a relatively new addition to the clinical trial landscape. These trials are designed to gather preliminary data on how a drug behaves in humans, focusing on pharmacokinetics and pharmacodynamics rather than therapeutic efficacy. Typically involving a small number of participants, Phase 0 studies aim to provide early insights into whether a drug is likely to be effective in treating a specific condition.
This phase is characterized by its emphasis on understanding the biological mechanisms at play and determining optimal dosing strategies. One of the key features of Phase 0 trials is their use of microdosing, where participants receive doses significantly lower than those expected to produce therapeutic effects. This approach allows researchers to observe how the drug is metabolized and distributed in the body without exposing participants to significant risk.
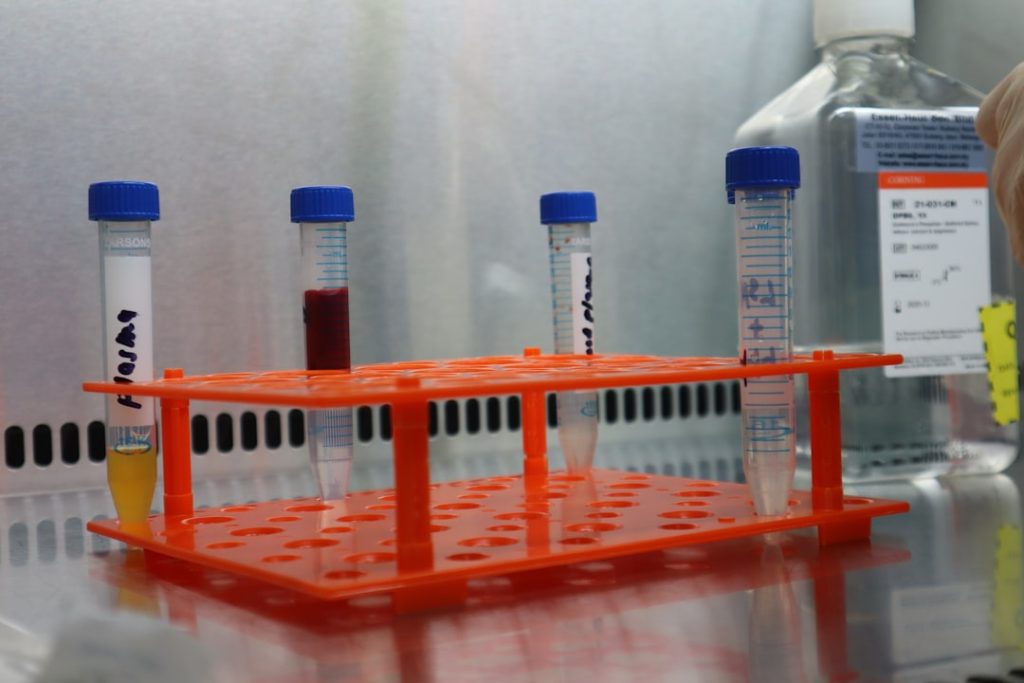
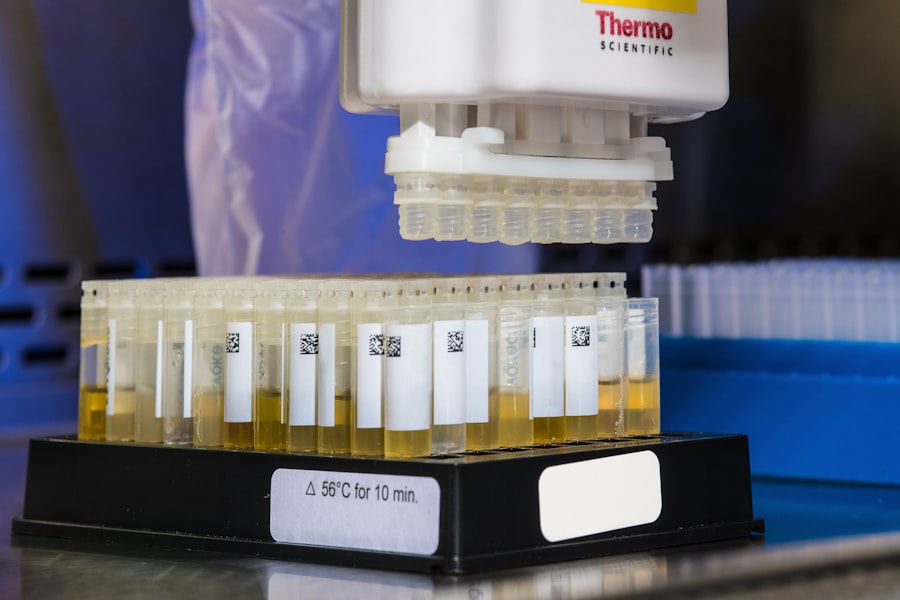
For instance, a Phase 0 study might involve administering a new cancer drug at a dose that is only 1/100th of the expected therapeutic dose. By analyzing blood samples and other biological markers, researchers can glean valuable information about the drug’s behavior in humans, which can inform subsequent phases of development.
Phase I: Safety and Dosage
Phase I trials are primarily concerned with assessing the safety profile of a new drug or treatment. Conducted with a small group of healthy volunteers or patients, these studies aim to identify any adverse effects associated with the drug and determine the appropriate dosage range for further testing. The focus during this phase is on safety rather than efficacy; researchers seek to establish a clear understanding of how the drug interacts with the human body.
Typically involving 20 to 100 participants, Phase I trials are often conducted in a controlled environment where researchers can closely monitor participants for any side effects. For example, if a new chemotherapy agent is being tested, researchers will observe participants for common side effects such as nausea, fatigue, or changes in blood counts. Additionally, they will assess how different dosages affect these side effects, allowing them to identify a maximum tolerated dose (MTD).
This information is critical for designing subsequent Phase II trials, where efficacy becomes a primary focus.
Phase II: Efficacy and Side Effects
Once a drug has demonstrated an acceptable safety profile in Phase I trials, it progresses to Phase II, where the focus shifts toward evaluating its efficacy and further assessing its safety. This phase typically involves a larger group of participants—ranging from 100 to several hundred—who have the condition that the drug aims to treat. Researchers aim to determine whether the drug produces a beneficial effect on the disease or condition while continuing to monitor for side effects.
In Phase II trials, researchers often employ randomized controlled designs to compare the new treatment against a placebo or standard therapy. For instance, if a new antidepressant is being tested, participants may be randomly assigned to receive either the new medication or an existing treatment. This design helps isolate the effects of the new drug from other variables that could influence outcomes.
Researchers will collect data on various endpoints, such as symptom improvement or quality of life measures, which will inform decisions about whether to advance to Phase III trials.
Phase III: Large-Scale Testing
| Phase | Purpose | Number of Participants | Duration | Key Focus | Typical Outcome |
|---|---|---|---|---|---|
| Phase 0 | Exploratory, first-in-human trials to understand pharmacodynamics and pharmacokinetics | 10-15 healthy volunteers | Several months | Drug behavior in the body at very low doses | Preliminary data on drug action and metabolism |
| Phase I | Assess safety, dosage range, and side effects | 20-100 healthy volunteers or patients | Several months | Safety and tolerability | Safe dosage range and identification of side effects |
| Phase II | Evaluate efficacy and further assess safety | 100-300 patients with the condition | Several months to 2 years | Effectiveness and side effects | Preliminary data on effectiveness and safety profile |
| Phase III | Confirm effectiveness, monitor side effects, compare to standard treatments | 1,000-3,000 patients | 1-4 years | Confirm efficacy and monitor adverse reactions | Comprehensive data for regulatory approval |
| Phase IV | Post-marketing surveillance to detect long-term effects | Various, often thousands of patients | Ongoing after approval | Long-term safety and effectiveness | Information on drug’s performance in general population |
Phase III trials represent a critical juncture in the clinical trial process, as they involve large-scale testing of a new treatment across diverse populations. These studies typically enroll hundreds to thousands of participants and are designed to confirm the efficacy observed in Phase II while further assessing safety in a broader context. The results from Phase III trials are often pivotal for regulatory approval by agencies such as the U.S.
Food and Drug Administration (FDA) or the European Medicines Agency (EMA). In this phase, researchers employ rigorous methodologies, including randomized controlled trials (RCTs) and double-blind designs, to minimize bias and ensure robust data collection. For example, if a new vaccine is being tested for efficacy against a viral infection, participants may be randomly assigned to receive either the vaccine or a placebo without knowing which group they belong to.
This approach helps ensure that any observed differences in outcomes can be attributed to the vaccine itself rather than external factors. The data generated during Phase III trials not only informs regulatory decisions but also provides critical information for healthcare providers and patients regarding the benefits and risks associated with new treatments.
Phase IV: Post-Market Surveillance

Phase IV trials occur after a drug has received regulatory approval and is available on the market. These post-marketing studies are essential for monitoring long-term safety and effectiveness in real-world settings. While earlier phases focus on controlled environments with selected populations, Phase IV trials assess how well a treatment performs across diverse patient demographics and varying clinical conditions.
One significant aspect of Phase IV studies is their ability to identify rare or long-term side effects that may not have been evident during earlier phases due to limited sample sizes or shorter follow-up periods. For instance, after a new diabetes medication is approved, ongoing surveillance may reveal unexpected cardiovascular risks that were not apparent during clinical trials. Regulatory agencies may require manufacturers to conduct these studies as part of their commitment to ensuring patient safety post-approval.
Importance of Understanding Clinical Trial Phases
Understanding the various phases of clinical trials is crucial for multiple stakeholders in healthcare—from researchers and clinicians to patients considering participation in studies. For researchers, knowledge of these phases informs study design and helps ensure compliance with regulatory requirements. It also aids in communicating findings effectively to both scientific communities and regulatory bodies.
For healthcare professionals, being well-versed in clinical trial phases enhances their ability to counsel patients about potential treatment options. Patients who understand these phases can make informed decisions about participating in clinical trials, weighing potential benefits against risks based on their individual health circumstances. Moreover, awareness of ongoing clinical trials can empower patients to seek out innovative therapies that may not yet be widely available.
Making Informed Decisions about Clinical Trials
The journey through clinical trial phases is complex but essential for advancing medical science and improving patient care. Each phase serves a distinct purpose in evaluating new treatments’ safety and efficacy while ensuring that patient welfare remains paramount throughout the process. By understanding these phases, stakeholders can navigate the intricacies of clinical research more effectively.
Informed decision-making regarding participation in clinical trials can lead to better health outcomes for individuals and contribute to broader advancements in medical knowledge. As research continues to evolve and new therapies emerge, maintaining an awareness of clinical trial phases will remain vital for all involved in healthcare—from researchers developing innovative treatments to patients seeking effective solutions for their health challenges.