Clinical trials are a cornerstone of modern medicine, serving as the bridge between laboratory research and the approval of new therapies for public use. These trials are meticulously structured into phases, each with distinct objectives and methodologies, designed to ensure that new drugs are both safe and effective before they reach the market. The journey of a new drug typically begins in the laboratory, where scientists conduct preclinical studies to gather initial data on its potential efficacy and safety.
Once a drug shows promise, it enters the clinical trial phase, which is divided into four main stages: Phase 1, Phase 2, Phase 3, and Phase 4. Each phase plays a critical role in the comprehensive evaluation of a drug’s therapeutic profile. The phased approach to clinical trials is not merely a bureaucratic necessity; it reflects a systematic method of risk management and scientific inquiry.
By breaking down the evaluation process into manageable segments, researchers can gather essential data at each stage, allowing for informed decision-making regarding the drug’s development. This structured progression also helps to protect participants by ensuring that only those therapies that demonstrate adequate safety and preliminary efficacy advance to subsequent phases. Understanding these phases is crucial for anyone interested in the drug development process, as they highlight the rigorous standards that must be met before a new treatment can be made available to patients.
Key Takeaways
- Clinical trial phases progress from initial safety testing to post-market surveillance.
- Phase 1 focuses on safety and determining appropriate dosage levels.
- Phase 2 evaluates the drug’s efficacy and monitors side effects.
- Phase 3 compares the new treatment against standard therapies in larger populations.
- Ethical considerations are crucial throughout all phases to protect participant welfare.
Phase 1 Clinical Trials: Exploring Safety and Dosage
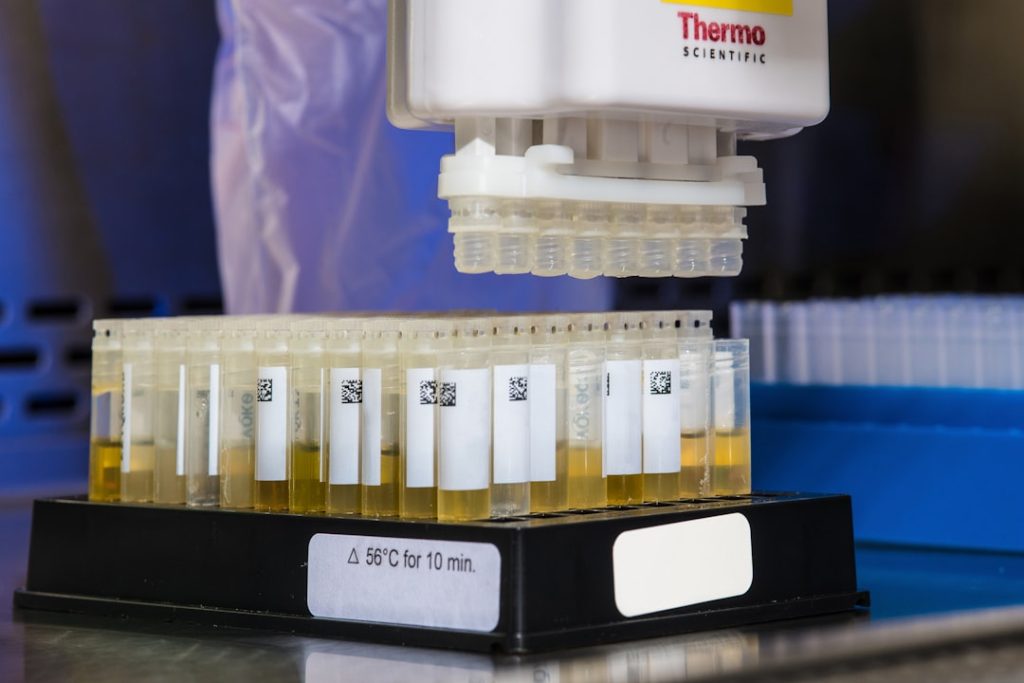
Phase 1 clinical trials are the first step in testing a new drug in humans. Typically involving a small group of 20 to 100 healthy volunteers or patients, these trials primarily focus on assessing the safety profile of the drug. Researchers aim to determine how the drug is metabolized and excreted by the body, as well as to identify any potential side effects.
This phase is crucial for establishing a safe dosage range and understanding how different individuals may respond to the treatment. The data collected during Phase 1 trials inform subsequent phases and help to refine dosing strategies. In addition to safety assessments, Phase 1 trials often explore pharmacokinetics and pharmacodynamics—the study of how the drug moves through the body and its biological effects, respectively.
For instance, researchers may administer varying doses of the drug to different groups of participants to observe how changes in dosage affect both safety and efficacy. A notable example of this is the development of cancer therapies, where initial doses are often escalated until side effects become intolerable or therapeutic effects are observed. This careful titration helps establish a maximum tolerated dose (MTD), which is critical for designing Phase 2 trials.
Phase 2 Clinical Trials: Assessing Efficacy and Side Effects

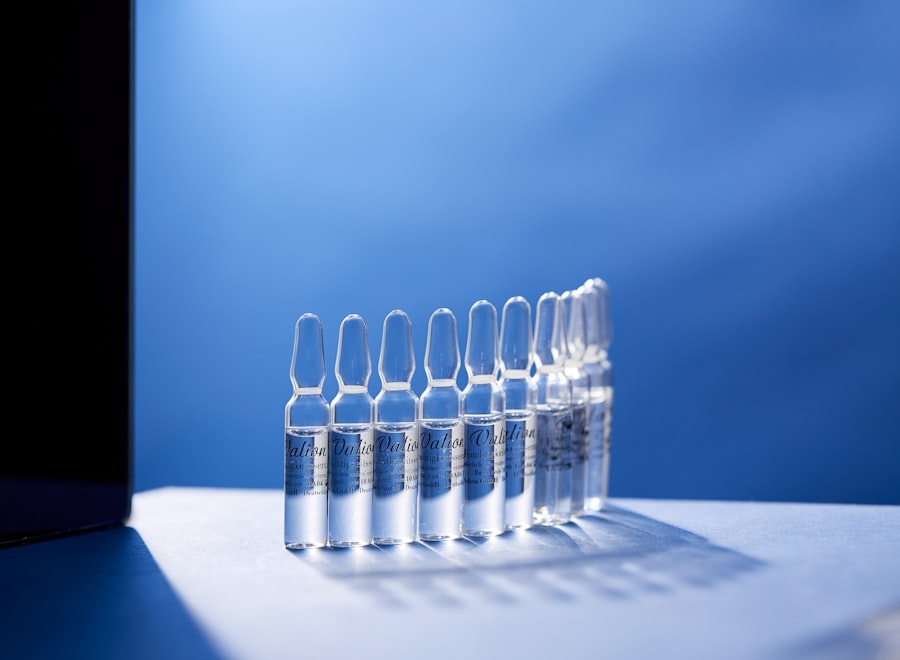
Once a drug has successfully passed through Phase 1 trials, it enters Phase 2, where the focus shifts from safety to efficacy. This phase typically involves a larger group of participants, often ranging from 100 to 300 individuals who have the condition that the drug aims to treat. The primary goal of Phase 2 trials is to evaluate whether the drug produces the desired therapeutic effect while continuing to monitor its safety profile.
Researchers also begin to gather more detailed information about side effects and how they may vary among different populations. Phase 2 trials can be further categorized into two sub-phases: Phase 2a and Phase 2b. Phase 2a trials primarily assess the drug’s efficacy at various doses, while Phase 2b trials focus on confirming efficacy at a specific dose identified in earlier studies.
For example, in the development of antidepressants, researchers may compare different dosages to determine which provides optimal relief from symptoms with minimal side effects. The results from these trials are pivotal; if a drug demonstrates significant efficacy in treating the targeted condition, it will advance to Phase 3 trials, where it will be compared against standard treatments or placebos.
Phase 3 Clinical Trials: Comparing to Standard Treatment
Phase 3 clinical trials represent a critical juncture in the drug development process, as they involve large-scale testing with hundreds to thousands of participants across multiple sites. The primary objective of this phase is to compare the new drug against standard treatments or placebos to determine its relative effectiveness and safety in a broader population. This comparison is essential for regulatory approval, as it provides robust evidence regarding how well the new therapy performs in real-world conditions.
In these trials, researchers employ randomized controlled trial (RCT) designs, which are considered the gold standard in clinical research. Participants are randomly assigned to receive either the new treatment or a control (standard treatment or placebo), minimizing bias and ensuring that results are attributable to the intervention itself rather than external factors. A prominent example of this phase can be seen in the development of statins for cholesterol management; large-scale Phase 3 trials demonstrated their effectiveness in reducing cardiovascular events compared to placebo groups.
The outcomes from these trials not only inform regulatory decisions but also guide clinical practice by providing healthcare professionals with evidence-based recommendations.
Phase 4 Clinical Trials: Post-Market Surveillance
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety and dosage | 20-100 healthy volunteers | Several months | Safety, side effects, pharmacokinetics | Approximately 70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Effectiveness, optimal dose | Approximately 33% |
| Phase 3 | Confirm effectiveness and monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Comparison to standard treatments | Approximately 25-30% |
| Phase 4 | Post-marketing surveillance | Thousands of patients | Ongoing after approval | Long-term effects, rare side effects | Varies |
Phase 4 clinical trials occur after a drug has received regulatory approval and is available on the market. These post-marketing studies are essential for ongoing surveillance of the drug’s safety and effectiveness in a larger population over an extended period. While pre-approval trials provide valuable insights into a drug’s performance under controlled conditions, Phase 4 studies help identify rare side effects or long-term consequences that may not have been evident during earlier phases due to smaller sample sizes or shorter follow-up periods.
One significant aspect of Phase 4 trials is their ability to assess how a drug performs in diverse populations that may not have been adequately represented in earlier studies. For instance, certain demographic groups—such as older adults or individuals with comorbidities—may respond differently to treatments than those included in initial trials. A notable example is the post-marketing surveillance conducted for vaccines; ongoing studies continue to monitor vaccine safety and efficacy as they are administered to millions of individuals worldwide.
This phase ensures that any emerging safety concerns are promptly addressed and that healthcare providers have access to up-to-date information regarding the drugs they prescribe.
Key Differences Between Each Phase
The differences between each phase of clinical trials are marked by their objectives, methodologies, participant populations, and outcomes measured. In Phase 1, the primary focus is on safety and dosage determination with a small group of healthy volunteers or patients; this phase lays the groundwork for understanding how the body interacts with the drug. In contrast, Phase 2 shifts attention toward efficacy and side effects among a larger group of participants who have the condition being treated, allowing researchers to refine dosing strategies based on therapeutic responses.
Phase 3 trials expand upon this foundation by comparing the new treatment against existing therapies or placebos in large populations across multiple sites. This phase is critical for establishing whether a new drug offers significant benefits over current standards of care. Finally, Phase 4 trials serve as an ongoing assessment mechanism after market approval, focusing on long-term safety and effectiveness in diverse populations.
Each phase builds upon the findings of its predecessor, creating a comprehensive framework for evaluating new therapies.
Importance of Clinical Trial Phases in Drug Development
The structured approach of clinical trial phases is vital for ensuring that new drugs are both safe and effective before they reach patients. Each phase serves a specific purpose that contributes to a thorough understanding of a drug’s therapeutic profile. By systematically evaluating safety, efficacy, and long-term outcomes, researchers can make informed decisions about whether to advance a drug through the development pipeline or halt its progress if concerns arise.
Moreover, these phases play an essential role in maintaining public trust in medical advancements. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) rely on data from these trials to make informed decisions about drug approvals.
The rigorous evaluation process helps ensure that only those therapies that meet stringent safety and efficacy standards are made available to patients, ultimately contributing to improved health outcomes and enhanced quality of life.
Ethical Considerations in Clinical Trial Phases
Ethical considerations are paramount throughout all phases of clinical trials. Researchers must prioritize participant safety and informed consent at every stage of the process. In Phase 1 trials, where healthy volunteers may be exposed to unknown risks, ethical guidelines require thorough explanations of potential side effects and rigorous monitoring for adverse events.
Participants must be fully informed about what participation entails and must voluntarily consent without coercion. As trials progress through subsequent phases, ethical considerations continue to evolve. In Phase 2 and Phase 3 trials, ensuring equitable access for diverse populations becomes increasingly important; researchers must strive to include underrepresented groups while also safeguarding vulnerable populations from exploitation or undue risk.
Additionally, transparency regarding trial results is crucial; ethical obligations extend beyond participant safety to include responsibilities toward public health and scientific integrity. Researchers must report findings accurately and promptly, regardless of whether results are favorable or unfavorable. In conclusion, understanding clinical trial phases is essential for grasping how new drugs are developed and evaluated for safety and efficacy before reaching patients.
Each phase serves distinct purposes that contribute to comprehensive assessments while adhering to ethical standards that protect participants throughout the process.