Clinical trials are a cornerstone of modern medicine, serving as the primary method for evaluating the safety and efficacy of new drugs, treatments, and medical devices. These trials are meticulously structured into distinct phases, each with specific objectives and methodologies. The progression through these phases is essential for ensuring that new interventions are both effective and safe for public use.
Understanding the intricacies of these phases is crucial not only for researchers and pharmaceutical companies but also for patients and healthcare providers who may be involved in or affected by these studies. The clinical trial process typically consists of four main phases, each building upon the findings of the previous one. Phase 1 focuses on safety and dosage, Phase 2 assesses efficacy and side effects, Phase 3 confirms efficacy and monitors adverse reactions, and Phase 4 involves post-market surveillance.
Each phase has its own set of goals, participant criteria, and regulatory requirements, which are designed to protect participants while generating reliable data that can inform medical practice. This article delves into each phase of clinical trials, elucidating their significance in the drug development process.
Key Takeaways
- Clinical trials progress through phases 1 to 4, each with distinct goals from safety to long-term monitoring.
- Phase 1 focuses on safety and dosage, involving a small number of healthy volunteers.
- Phase 2 evaluates efficacy and side effects in a larger patient group.
- Phase 3 confirms effectiveness and monitors adverse reactions in diverse populations before approval.
- Phase 4 occurs post-market to ensure ongoing safety and effectiveness in the general population.
Phase 1 Clinical Trials: Exploring Safety and Dosage
Phase 1 clinical trials are the first step in testing a new drug or treatment in humans. These trials typically involve a small group of healthy volunteers, usually ranging from 20 to 100 participants. The primary objective during this phase is to evaluate the safety profile of the drug, determine a safe dosage range, and identify any potential side effects.
Researchers closely monitor participants for adverse reactions, which can provide critical insights into how the drug interacts with the human body. In addition to safety assessments, Phase 1 trials often explore pharmacokinetics—the study of how the drug is absorbed, distributed, metabolized, and excreted by the body. This information is vital for understanding how the drug behaves in different populations and can inform subsequent dosing strategies.
For instance, if a drug is found to be metabolized more quickly in certain individuals, researchers may adjust dosing recommendations accordingly. A notable example of a Phase 1 trial is the testing of the cancer drug imatinib (Gleevec), which initially focused on determining safe dosage levels before moving on to larger studies.
Phase 2 Clinical Trials: Assessing Efficacy and Side Effects
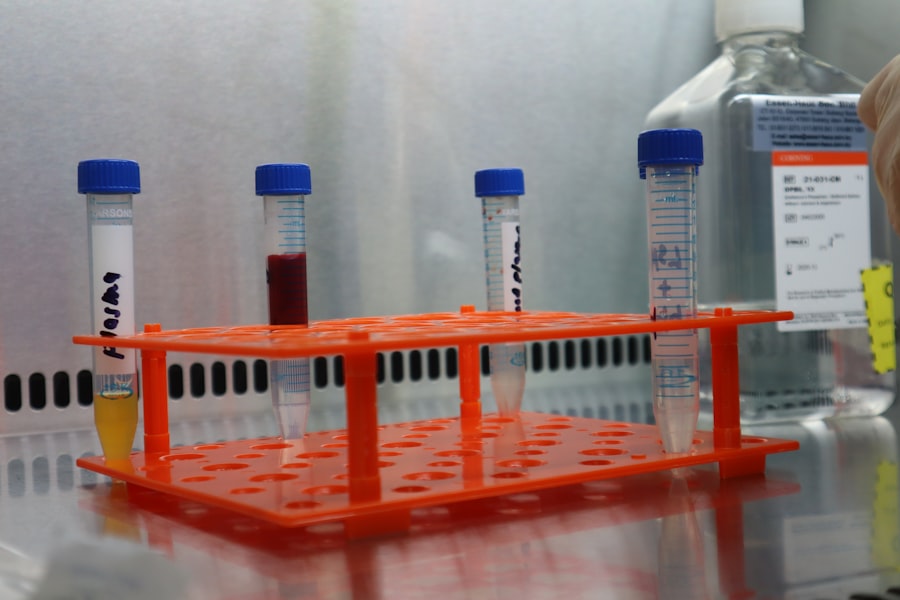
Once a drug has successfully passed through Phase 1 trials, it enters Phase 2, where the focus shifts from safety to efficacy. This phase typically involves a larger group of participants, often ranging from 100 to several hundred individuals who have the condition that the drug aims to treat. The primary goal of Phase 2 trials is to assess whether the drug has a therapeutic effect on the targeted condition while continuing to monitor its safety profile.
During this phase, researchers employ various study designs, including randomized controlled trials (RCTs), to compare the new treatment against a placebo or standard treatment. This comparison helps establish whether any observed effects are due to the drug itself rather than external factors. For example, in a Phase 2 trial for a new antidepressant, participants might be randomly assigned to receive either the new medication or a placebo.
The outcomes would then be measured using standardized scales for depression severity. A successful Phase 2 trial can lead to further investigation in Phase 3 trials, where larger populations are studied to confirm efficacy.
Phase 3 Clinical Trials: Confirming Efficacy and Monitoring Adverse Reactions
Phase 3 clinical trials represent a critical juncture in the drug development process. These trials involve large groups of participants—often thousands—across multiple sites and sometimes even countries. The primary aim is to confirm the efficacy of the drug in a broader population while continuing to monitor for adverse reactions.
This phase is essential for providing robust evidence that can support regulatory approval. In Phase 3 trials, researchers often employ double-blind methodologies, where neither participants nor investigators know who is receiving the treatment versus a placebo or standard care. This design minimizes bias and enhances the reliability of results.
For instance, in a Phase 3 trial for a new vaccine, participants would be randomly assigned to receive either the vaccine or a placebo without knowing which they received. The outcomes would be measured based on infection rates in both groups over time. Successful completion of Phase 3 trials typically leads to submission for regulatory approval, as they provide comprehensive data on both efficacy and safety.
Phase 4 Clinical Trials: Post-Market Surveillance and Long-Term Safety
| Phase | Primary Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Safety and dosage | 20-100 healthy volunteers | Several months | Assess safety, determine safe dosage range, identify side effects | Approximately 70% |
| Phase 2 | Effectiveness and side effects | 100-300 patients | Several months to 2 years | Evaluate effectiveness, further assess safety | Approximately 33% |
| Phase 3 | Confirm effectiveness, monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Confirm effectiveness, monitor side effects, compare to commonly used treatments | Approximately 25-30% |
| Phase 4 | Post-marketing surveillance | Various (thousands) | Ongoing after approval | Monitor long-term effectiveness and safety, detect rare or long-term adverse effects | Varies |
Phase 4 clinical trials occur after a drug has received regulatory approval and is available on the market. These trials are often referred to as post-marketing surveillance studies and serve several important purposes. They continue to monitor the long-term safety and effectiveness of the drug in a larger population over an extended period.
This phase is crucial because it allows researchers to identify rare side effects that may not have been evident in earlier phases due to smaller sample sizes. In addition to safety monitoring, Phase 4 trials can also explore new indications for an already approved drug or assess its performance in different populations or settings. For example, a medication initially approved for treating hypertension may undergo Phase 4 studies to evaluate its effectiveness in patients with diabetes.
These studies can provide valuable insights that inform clinical practice and guide healthcare providers in making treatment decisions.
Differences in Study Design and Participant Inclusion Criteria
The design of clinical trials varies significantly across different phases, reflecting their distinct objectives and requirements. In Phase 1 trials, the focus is primarily on safety; thus, inclusion criteria often emphasize healthy volunteers without underlying health conditions that could confound results. Conversely, Phase 2 trials require participants who have the specific condition being studied, allowing researchers to assess therapeutic effects more accurately.
Phase 3 trials expand on this by incorporating diverse populations to ensure that findings are generalizable across different demographics. Inclusion criteria may consider factors such as age, gender, ethnicity, and comorbidities to reflect real-world patient populations. This diversity is essential for understanding how various groups respond to treatment and for identifying any population-specific side effects or efficacy variations.
In contrast, Phase 4 studies may have even broader inclusion criteria as they aim to capture data from everyday clinical practice. These studies often include patients who may have been excluded from earlier phases due to specific health conditions or concurrent medications. This approach helps ensure that post-marketing data reflects actual usage patterns and patient experiences in real-world settings.
Regulatory Approval and Drug Development Process
The journey from initial discovery to regulatory approval is complex and multifaceted. After successful completion of Phase 3 trials, pharmaceutical companies compile extensive data into a New Drug Application (NDA) or Biologics License Application (BLA) for submission to regulatory agencies such as the U.S. Food and Drug Administration (FDA) or European Medicines Agency (EMA).
This application includes detailed information about clinical trial results, manufacturing processes, labeling proposals, and plans for post-marketing surveillance. Regulatory agencies rigorously review these applications to ensure that new drugs meet established safety and efficacy standards before they can be marketed to the public. This review process can take several months or even years, depending on the complexity of the data submitted and any additional information requested by regulators.
Once approved, ongoing monitoring continues through Phase 4 studies to ensure that any long-term effects or rare adverse reactions are identified promptly. The regulatory approval process is not only about ensuring safety but also about balancing risks with potential benefits. Agencies must consider whether the therapeutic advantages of a new drug outweigh any associated risks based on available evidence from clinical trials.
Importance of Understanding Clinical Trial Phases for Patients and Healthcare Providers
For patients considering participation in clinical trials or those seeking new treatment options, understanding the phases of clinical trials is paramount. Knowledge about what each phase entails can empower patients to make informed decisions about their healthcare choices. For instance, patients may feel more comfortable participating in Phase 2 or Phase 3 trials when they understand that these studies are designed to assess efficacy in individuals with their specific condition.
Healthcare providers also benefit from understanding clinical trial phases as they guide patients through treatment options. By being well-versed in the nuances of each phase, providers can better explain potential risks and benefits associated with participation in clinical research. This knowledge fosters trust between patients and providers while promoting informed consent processes that respect patient autonomy.
Moreover, awareness of clinical trial phases can help patients recognize that not all treatments are created equal; some may still be under investigation while others have established safety profiles through rigorous testing. This understanding can lead to more meaningful discussions about treatment plans and expectations regarding outcomes. In conclusion, clinical trial phases play an essential role in advancing medical science by ensuring that new therapies are thoroughly evaluated before reaching patients.
Each phase serves a unique purpose within the broader context of drug development, contributing valuable data that informs clinical practice and regulatory decisions alike. As both patients and healthcare providers navigate this complex landscape, a solid grasp of these phases enhances communication and decision-making processes in healthcare settings.



